Introduction
The impact of prehospital time on the clinical outcome of trauma patients is a well-known concept in the international trauma community. Reference Tomasich, Marttos, Collaço, Abreu, Namias and Nasr1 A prolonged prehospital interval is associated with increased in-hospital mortality rates, and efficient prehospital care with fast responses is the norm in most countries. Reference Gauss, Ageron and Devaud2-Reference Ruelas, Tschautscher, Lohse and Sztajnkrycer4 Emergency medical services (EMS) play a critical role in prehospital care and are the initial health care providers on scene. They provide immediate medical care and transport patients to a hospital for definitive care. In prehospital settings, EMS providers have to make fast and critical decisions under stress and uncertainty. Reference Peleg, Michaelson, Shapira and Aharonson-Daniel6 In some incidents, the EMS is overwhelmed by the number or severity of casualties, and the event is labeled as a mass casualty incident (MCI). Reference Ben-Ishay, Mitaritonno, Catena, Sartelli, Ansaloni and Kluger5
Multiple triage methods have been developed to guide EMS personnel in their decisions. Reference Kennedy, Aghababian, Gans and Lewis7 MCI triage aims to quickly determine the priority of the patients’ treatment based on the severity of their condition, and allows first responders to assess a large number of patients, with the objective to do the best for the largest number of people with limited resources. Reference Benson, Koenig and Schultz8,9 Another commonly used decision tool is the Field Triage Criteria (FTC). This tool helps EMS personnel to decide which patients need to be transported to a trauma center for optimal care. Both triage methods aim at decreasing mortality and morbidity by improving the efficiency of prehospital trauma care. We hypothesized that efficient prehospital care, results in faster EMS responses during MCIs. The study’s primary aim was to evaluate the prehospital time for patients involved in an MCI and compare this with the prehospital time for patients not involved in an MCI. The secondary aim was to evaluate the effect of triage on prehospital time.
Methods
Study Design
A retrospective analysis was conducted using Florida’s EMS Tracking and Reporting System (EMSTARS) database. All EMS encounters submitted to the EMSTARS database from January 1, 2018 through December 31, 2018 were assessed. Reference Heemskerk, Domingo and Tawk10 The study was performed in accordance with the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement to secure proper reporting and improve methodological quality. Reference von Elm, Altman and Egger11 The EMSTARS Data Use Agreement was signed, and approval of the study was given by the Florida Department of Health. Institutional review board exemption for this study was obtained, and the study was performed according to the Declaration of Helsinki and amendments.
EMSTARS Database and Setting
The EMSTARS database (version 3.4), developed to help collect prehospital data, is used for benchmarking and identifying quality improvement initiatives. 12 It is maintained by the Florida DOH as part of the National EMS Information System project (NEMSIS). Reference Dawson13 The database contains data from 196 EMS agencies covering all 67 counties in Florida. Providers from participating EMS agencies create an electronic patient care record for each response using standardized forms. After filling out the patient’s record, this data is submitted to the EMSTARS database. Some data are mandatory to submit (e.g., specific time points, age, gender) and other data are optional (e.g., use of a triage method). Time is mostly collected automatically to create a precise record. The EMSTARS dictionary lists the collected data in the EMSTARS database, specifies the definitions, and reports which data are mandatory and which are optional to submit. The dictionary is available on the EMSTARS website. 12 The EMSTARS definition used for MCI is defined as an event that overwhelms an agency’s EMS resources.
Outcome Measures
The primary aim of this study was to evaluate the median EMS response time for patients who were involved in an MCI and compare this with the median EMS response time for patients who were not involved in an MCI. Several prehospital time intervals were calculated and used in the analysis (see Table 1 for definitions). The secondary aim was to evaluate the effect of triage on prehospital time.
Table 1. Time interval definitions
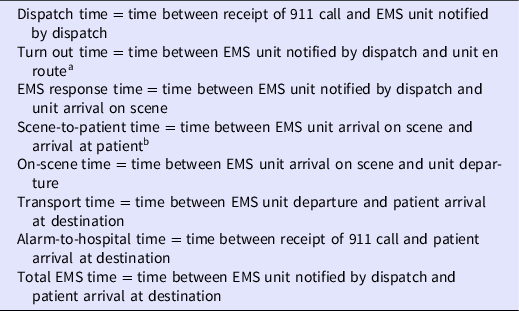
a Time interval within EMS response time.
b Time interval within on-scene time.
In the EMSTARS database, 2 triage methods were documented: (1) the method for MCI triage, and (2) field triage using the Field Triage Criteria (FTC). MCI triage is designed to classify patients according to the severity of the injury and help health professionals decide which patient should be treated first. The MCI triage methods used in this dataset were the START triage method (Simple Triage and Rapid Treatment) and the SALT triage method (Sort, Assess, Life Saving Interventions, Treatment/Transport) (see Appendices 1 and 2). Reference Benson, Koenig and Schultz8,9 Patients were classified according to the severity of the injury and assigned to 1 of the following 4 categories: uninjured/minimally injured (green), moderately injured/delayed (yellow), severely injured/immediate (red), or deceased/dead (black). The field triage method evaluated in this study was the FTC. Reference Sasser, Hunt and Faul14 FTC is the most used field triage method in the US and is developed to identify injured patients who are most likely to benefit from specialized trauma center resources. The FTC is not intended for MCI triage, but for the individual patient. It guides EMS personnel to determine which patient should be transported to a trauma center for appropriate treatment. It is published by the Center for Disease Control and Prevention in collaboration with the American College of Surgeons Committee on Trauma and the National Highway Traffic Safety Administration. The FTC consists of 4 steps: physiologic, anatomic, mechanism of injury, and special considerations (Appendix 3). If step 1 or 2 is positive, it is advised to transport the patient to the highest level of care within the trauma system.
In total, 3 analyses were performed. The first analysis compared the response time of transporting EMS units involved in an MCI with EMS units that transported non-MCI patients, the second analysis evaluated the response time when MCI triage (START or SALT) was used and the third analysis evaluated the response time, when field triage (FTC) was used.
Case Selection
For this study, all 2018 EMS activations in Florida were analyzed. A total of 3 subsets were assessed: (1) a subset of unique MCIs, (2) all EMS units dispatched to an MCI, and (3) all EMS units that transported MCI patients to a hospital. Patients were selected if they were recorded as a 911 response (EMSTARS database code (eResponse.05: 911 Response [2205001]) and if EMS registered the patients as part of an MCI (eScene.07: [9923003]). Time intervals were calculated for all transporting EMS units that transported patients to a health facility. Cases with invalid time intervals (i.e., negative time intervals) were excluded from the analysis.
Identifying Unique MCIs
Multiple EMS vehicles can respond to the same MCI. To identify multiple EMS encounters for 1 MCI, all EMS encounters with the same ZIP code and time (with a range of 5 minutes) were identified and evaluated. If this was the same for several EMS units, this was considered as 1 MCI. The following time points were evaluated: (1) the moment the public-safety answering point was alerted, (2) the moment that the dispatch was notified, and (3) the moment that the EMS unit was en route. An EMS unit could transport several patients per unit.
Statistical Analysis
All collected data were extracted from the EMSTARS database. The incidence rate with the binomial 95% confidence interval was calculated by dividing the estimated number of MCIs found in Florida by the total population of Florida in 2018. 15 The Mann-Whitney U test was used to compare 2 groups with unpaired skewed data, and the Kruskal-Wallis test was used to compare more than 2 groups with unpaired skewed data. For these tests, the assumption of homogeneity of variance was tested using the non-parametric Levene’s test. Statistical analyses were performed using SAS Enterprise Guide V7.1 (SAS Institute Inc., Cary, NC) and RStudio V3.6.1 (RStudio, Inc. Boston, MA). For all hypotheses testing, a P < 0.05 was considered significant.
Results
Case Selection
In 2018, 196 of the 285 licensed agencies in Florida (68.8%) submitted their data to the EMSTARS database. In total, 3653281 EMS responses were submitted, and 3262 responses (0.09%) were recorded as an MCI. Of these, 2180 units arrived at the hospital (66.9%). Sometime intervals were excluded because of an invalid negative time value (15 for scene-to-patient time, 1 for on-scene time, and 1 for transport time). It was not possible to calculate the dispatch center time and alarm-to-hospital time for 466 cases because the moment of 911 call was not recorded.
MCI Characteristics in Florida
Among the 3263 documented EMS responses to an MCI, it was estimated that there were 2236 unique MCIs (Table 2). This resulted in an incidence of 10.5 MCIs per 100000 people (95% CI, 10.1 - 10.9) in Florida in 2018. Among the regions in Florida, the highest incidence was seen in region 6, with 19.7 MCIs per 100000 people (95% CI, 18.0 - 21.5), followed by 15.0 (95% CI, 12.8 - 17.5) in region 1, 12.6 (95% CI, 11.5 - 13.7) in region 5, 11.8 (95% CI, 9.4 - 14.9) in region 2, 9.8 (95% CI, 8.9 - 10.8) in region 4, 6.9 (95% CI, 6.3 - 7.6) in region 7, and 4.7 (95% CI, 3.9 - 5.7) in region 3 (Figure 1a). Most MCIs occurred in the late afternoon with a peak between 4:00 PM and 6:00 PM (Figure 1b). The majority of the MCIs (78.5%) resulted in a response of 1 MCI unit.
Table 2. Characteristics of MCIs (N = 2236)

Abbreviations: EMS, Emergency Medical Service; MCI, mass casualty incident.

Figure 1. a. Frequency of MCIs by Region in Florida (n = 2236). b. Time and Month of Occurrence of Mass Casualty Incidents (n = 2236). Abbreviation: MCI, mass casualty incident.
Characteristics of Patients Transported
In total, 2180 EMS units transported MCI patients to a hospital (66.8%). A total of 14.5% of the EMS units transported more than 1 patient from the incident location to the hospital (Table 3). MCI patients were significantly younger than non-MCI patients (44.2 ± 26.2 vs. 59.6 ± 23.1 years; P < 0.001). Majority of the patients were women (55.8%) and white (58.5%). The main primary symptom for transportation was pain (19.4%), and the main cause of injury was related to a motor-vehicle incident (43%).
Table 3. Characteristics of transporting units (n = 2180)

a Primary symptom was missing for 874 patients.
Prehospital Time for Transported MCI Patients
Time intervals were calculated for all patients transported to a health facility (Table 1 for interval definitions). The prehospital time intervals of MCI patients were compared with all other transported non-MCI patients in the EMSTARS database. Significant differences were found for all prehospital time intervals, except for the turn out time interval (Table 4). MCIs resulted in longer prehospital time intervals, except for the time-to-scene and scene-to-patient time intervals, which were shorter. The median alarm-to-hospital time was 43.74 minutes, and the total EMS time was 39.75 minutes. On-scene time (15.80 min) and transport time (14.10 min) comprised approximately a third of the total alarm-to-door time. The most significant difference between MCI responses and non-MCI responses was seen in transport time (14.10 min vs. 12.52 min; P < 0.001).
Table 4. EMS prehospital time intervals for MCIs and non-MCI patients in Florida in 2018

Abbreviations: EMS, Emergency Medical Service; IQR, interquartile range; MCI, mass casualty incident.
a Minutes are reported as decimal time.
b Mann-Whitney U test.
Prehospital Time with MCI Triage
For 625 patients, an MCI triage method was recorded (START or SALT). Reference Benson, Koenig and Schultz8,9 When a triage method was recorded in the EMSTARS database, this resulted in a significantly shorter median total EMS time (38.12 vs. 40.40 min, P = 0.012) and alarm-to-hospital time (39.37 vs. 45.00 min, P < 0.001). There was no statistical difference in on-scene time (15.53 vs. 15.93 min, P = 0.243) or transport time (13.19 vs. 14.62 min, P = 0.08) when an MCI triage method was used.
Of the triaged patients, 400 were classified as green, 137 as yellow, 76 as red, and 12 as black (Table 5). The total EMS time decreased significantly when the priority of the triage category was higher (H (3) = 5.969, P < 0.011). The total EMS time for red patients was 35.77 minutes, while the total EMS time was 39.07 minutes for green patients.
Table 5. EMS Prehospital Time Using MCI Triage

Abbreviations: EMS, Emergency Medical Service; IQR, interquartile range.
a Median (IQR), min. Minutes are reported as decimal time.
b Kruskall-Wallis test; comparison of the 4 triage categories.
Prehospital Time with Field Triage Criteria
The FTC was used for 710 injured patients and was associated with a significantly shorter alarm-to-hospital time interval (37.55 vs. 45.70; P < 0.001). Steps 1 and 2 of the FTC attempt to identify the most seriously injured patients and help EMS personnel decide which patients should be transported to the highest level of care within the trauma system (Appendix 3). When 1 of the 2 steps was positive, the patient had to be transported to a trauma center. This was associated with significantly longer transport time (17.60 min) and alarm-to-hospital time (43.75 min) (Table 6).
Table 6. EMS prehospital time using field triage criteria

Abbreviations: EMS, Emergency Medical Service; IQR, interquartile range.
a Median (IQR), min. Minutes are reported as decimal time.
b Mann-Whitney U test.
c If step 1 or 2 was positive.
Discussion
MCIs are characterized by an overwhelmed EMS caused by an imbalance between the demand for medical care and the supply of available resources. Reference Ben-Ishay, Mitaritonno, Catena, Sartelli, Ansaloni and Kluger5 This study shows that MCIs resulted in longer alarm-to-hospital times than non-MCIs (43.74 min vs. 39.15 min). Triage methods are developed to help EMS providers make fast and critical decisions. In this study, MCI triage and field triage were associated with shorter alarm-to-hospital time intervals (-5.63 and -8.15 minutes, respectively).
Mass casualty Incidents
The priority of the EMS is to deliver the fastest possible patient care. However, responses to MCIs are often characterized by inefficient overall control and lack of coordination because of their sudden and infrequent nature. Our study may show this overwhelming aspect by showing that prehospital time intervals are longer when an MCI is declared. A previous study has been published describing the characteristics of MCIs and evaluating prehospital time intervals during MCIs in the United States. Reference Schenk, Wijetunge, Mann, Lerner, Longthorne and Dawson16 Unfortunately, the time intervals are not comparable because they summarized their data with mean and standard deviation, while we used median and interquartile range since our data was strongly skewed. As a result, our time intervals are much shorter. Nevertheless, their conclusion is in agreement with our study as they also found prolonged time intervals for MCIs compared with non-MCIs. Another study evaluated general prehospital time intervals in the United States. Reference Wang, Mann and Jacobson17 In this study, the time intervals (14 min for on-scene and 12 min for transport) were comparable with our non-MCI data (14.78 min for on-scene and 12.52 min for transport). Most of the MCI (n = 1756) resulted in a response of 1 EMS unit. The majority of these units transported more than 1 patient per ride but only documented the demographics of 1 patient. Therefore, the estimate of MCI incidence may be more accurate than the estimate of the number of MCI patients per incident.
MCI Triage
Since mortality and morbidity are time-dependent during an MCI, efficient time management is an important goal. Reference Ruelas, Tschautscher, Lohse and Sztajnkrycer4 Decisions have to be made despite uncertainty and limited resources during an MCI. MCI triage was developed to guide EMS personnel and support decision making for medical management of casualties during MCIs. MCI triage must quickly identify individuals who would most likely benefit from immediate medical attention while not expending valuable resources on those who are not salvageable. Our study results show that total EMS time decreased when the MCI triage category was more urgent without extending on-scene time. The total EMS time was 35.77 minutes for red patients and 39.07 minutes for green patients. We would expect the same trend for on-scene time and transport time; however, yellow patients had longer time intervals for these periods. While both red and yellow patients had conditions that required urgent intervention, red patients had more complex conditions and were the first to be transported to a hospital for critical care. Yellow patients had to wait but needed urgent care. It is conceivable that these patients were treated on-site, resulting in longer evacuation times. Interestingly, black (expectant) patients had the shortest total EMS time, against the expected longer time intervals. During an MCI, not every patient can receive high-quality care directly because of the limited resources. In theory, this category should have a low priority because these patients are either dead or have such extensive injuries that they cannot be saved with the limited resources available. Treatment for these patients would jeopardize the survival of the other victims by diverting limited resources away from salvageable patients. However, in practice, this category is the most challenging for EMS personnel from an emotional and ethical standpoint. The health professional’s mindset has to change from individual emergency care to mass casualty care in which the focus is shifted to the entire patient group. However, this mindset is difficult to learn. Reference Frykberg18 In overwhelming events, triage could help as a decision tool. It allows the health professional to prioritize care services and justifies hard decisions by doing the best for the most.
Field Triage
The FTC are developed to improve the coordination of transport for individual patients. Reference Sasser, Hunt and Faul14 Transporting injured patients to the most appropriate medical care facility is an important decision for EMS personnel and can profoundly impact patient survival. Reference Frykberg18,Reference MacKenzie, Rivara and Jurkovich19 It helps EMS personnel to decide which patients should go to the highest trauma center within the trauma system. A study from 2017 evaluated the implementation of the FTC for general EMS responses and found that the FTC had little effect on total EMS time. The authors suspected this result was due to delays in information dissemination and adoption by EMS providers. Reference Brice, Shofer and Cowden20 Nonetheless, our study shows that the use of the FTC was associated with significantly shorter prehospital time intervals during MCIs. The effect of field triage may be more visible during overwhelming events because triage is more effective in structuring stressful events resulting in more significant time differences. However, when step 1 or 2 of the field triage was positive, this resulted in longer transport time (4.22 min) and total EMS time (6.55 min). This result may be explained by ambulances having to drive a longer distance to the highest trauma center, resulting in longer time intervals.
Clinical Relevance
This study takes advantage of a large dataset that covers all counties of Florida. By analyzing empirical data instead of experimental data, this study has a key strength in understanding MCIs in the prehospital setting. A recent study highlighted the importance of prehospital time on survival in trauma patients. Reference Gauss, Ageron and Devaud2 Our current study showed that MCIs were associated with longer EMS time intervals resulting in a longer alarm-to-hospital time (4.59 minutes extra). This finding suggests opportunities for improvement in prehospital care for MCI patients that can be centered on reducing prehospital time. MCI triage and field triage were both associated with shorter total EMS response intervals, and implementation of these triage methods may improve prehospital care for MCI patients.
Limitations
First, 33.1% of the licensed EMS agencies in Florida did not submit their data to the EMSTARS database. Therefore, the results may not be generalizable to the entire state of Florida. In the future, the quality of the database could be improved by increasing the submission rate of EMS agencies.
Other limitations are inherent to the retrospective design of the study. Retrospective research is prone to errors and missing data due to inconsistent or inaccurate data collection. Some data fields in the EMSTARS database are optional and not mandatory to submit. It is conceivable that some optional data were not submitted, resulting in under-reporting of the outcome. To prevent bias from under-reporting, we propose that the DOH makes more variables mandatory based on specific conditions. For instance, the variable “Triage Classification for MCI Patient” should become mandatory when an EMS encounter is recorded as an MCI. In the current situation, it is possible to submit MCI data with no data value stored for the variable “Triage Classification for MCI Patient.”
Another problem is inaccurate data collection. Negative time intervals were excluded from the analyses, but positive incorrect values remained unnoticed. To enhance the quality of the EMSTARS database, mechanisms should be developed to prevent wrong data submission.
Finally, interesting variables are missing in this retrospective database study. It was not possible to extract information about which MCI triage method (START or SALT) was used. Another informative variable would be the reason why an MCI was registered as an MCI.
Implications
It is important to distinguish MCI triage from field triage. MCI triage prioritizes patients by the severity of injury to allocate limited resources when local resources are overwhelmed. In contrast, field triage matches patients with the right resources when enough resources are available. Both triage methods were associated with shorter total EMS time and alarm-to-hospital time intervals. MCIs are by definition overwhelming, and it is hypothesized that triage may structure the situation by providing a step-by-step roadmap of what to do. It helps EMS personnel make faster decisions, which may lead to shorter prehospital time intervals. Based on this rationale, we recommend that EMS agencies should use triage during MCIs and implement these methods in their MCI protocol. If an EMS agency does not have an MCI protocol, it is recommended to develop it. MCIs are infrequent and by definition overwhelming. Clinical exposure is low and preparedness is therefore essential. Planning for MCI preparedness is the key to a successful outcome.
Directions for Future Research
Future studies should evaluate the clinical relevance of faster prehospital responses during MCIs. Our study only evaluated time and did not focus on the accuracy of the triage methods or clinical outcomes. Reference Newgard, Schmicker and Hedges21 Previous studies have shown that faster prehospital responses are associated with improved survival. Reference Gauss, Ageron and Devaud2,Reference Blackwell and Kaufman22 Future research should therefore investigate this for MCIs.
Conclusion
The time between the injury to definitive medical care in prehospital care is key to optimal survival for trauma patients. Reference Gauss, Ageron and Devaud2 This study shows that MCIs resulted in longer prehospital time intervals than non-MCIs. This finding suggests that additional efforts are needed to reduce the prehospital time for MCI patients. MCI triage and field triage were both associated with shorter total EMS intervals. Triage works as a decision tool helping EMS personal to make fast and critical decisions. It seems that triage could also help in reducing prehospital time. Future studies are necessary to evaluate this hypothesis.
Data Availability Statement
The data and materials are available to strengthen the transparency and reliability of the study. The additional data could be requested by sending an e-mail to the corresponding author. ©2020 Mayo Foundation for Medical Education and Research.
Acknowledgments
The authors would like to thank Junwei Jiang and the Florida Department of Health for their assistance in retrieving and managing the data files for this study. This study is derived from the European Master of Disaster Medicine Thesis of Johan L Heemskerk. In addition, the authors would like to acknowledge and thank all participating EMS providers and EMS agencies who support and provide data to Florida’s EMSTARS.
Conflict of Interest
The authors have no conflict of interest to declare. This article is the result of a thesis submitted to the Free University of Brussel, Belgium, and the University of Eastern Piedmont, Italy, in partial fulfillment of the requirements for the Master of Science in Disaster Medicine (European Masters in Disaster Medicine).
Ethics Statement
Approval for this study was granted by the Institutional Review Board of the Florida Department of Health. The study is performed according to the Declaration of Helsinki and amendments.
Supplementary material
To view supplementary material for this article, please visit https://doi.org/10.1017/dmp.2021.40









