In the 18th century, as munitions were incorporated into war, military physicians described shell shock in patients with blast injuries. In the previous century, military surgeons further elucidated the pathophysiology and management of blast injury through research and practical experience on the battlefield.Reference Zuckerman1Reference Born2 The civilian medical force has been largely spared the exposure and thus the training needed for blast-injured patients. Given the present geopolitical landscape and disconcerting trend of increasing terrorist attacks to civilian targets worldwide, however, there is a pressing need to train and prepare physicians in all sectors for dealing with these issues.
In the counterterrorism movement much emphasis has been placed on prevention of attacks with weapons of mass destruction (eg, nuclear, chemical, biological). However, the most frequent weapons in terror attacks are conventional explosive materials detonated in strategic locations, often with the intent to inflict mass injury on innocent civilians.Reference Zuckerman1Reference Born2Reference Arnold, Halpern, Tsai and Smithline3 Fundamental training in blast mechanics, pathophysiology, and management of blast-injured patients has become a requisite of all physicians, surgeons, and emergency medical personnel.
The middle ear is the most sensitive organ to primary blast injury. Tympanic membrane perforation with accompanying hearing loss and tinnitus are common symptoms. Trauma resulting in dizziness and hearing loss can be disorienting to patients, making it difficult for them to cooperate with emergency medical personnel. Although immediate treatment of the ear is, appropriately, not the highest priority in treating a person with blast injuries, a quick otoscopic evaluation can provide helpful clues suggesting the possibility of serious occult injury. Proper diagnosis, simple initial treatment, and referral to a specialist will improve the otologic outcomes for the blast-injured ear.
A MEDLINE literature search (1966–June 2007) with an Ovid interface was performed. Search terms included blast injury, external ear, middle ear, inner ear, tympanic membrane, vestibule, and labyrinth. Articles with topics pertinent to primary blast injury and blast injury to the ear were selected through a search of their titles or abstracts. After an article was selected, a search of its references was performed to identify additional sources. Forty-two articles have been selected from more than 200 screened based on their historical, pathophysiological, and clinical significance specific to primary blast injury and blast injury to the ear.
Our literature review yields no randomized controlled trials. This is not unexpected given the unpredictable circumstances and epidemiology of blast injury. The majority of prognostic data available regarding blast injuries in human subjects are of 2 types. The first is the consistent retrospective cohort study (level 2), in which data about multiple blast incidents are accumulated for a specified period of time. The second is the retrospective case series (level 4), presenting prognostic outcomes among a group of blast victims resulting usually from a specific incident. Specific animal and cadaveric studies (level 5) have been used to better elucidate pathophysiologic principles in a controlled prospective manner. Select nonsystematic review articles (level 5) have been cited for historical content, discussions regarding the physical properties of blast mechanics, and expert opinions. In summation, the articles referenced in the present review include 7 level 2, 19 level 4, and 16 level 5 sources. Clinical recommendations are based on retrospective cohort studies, case series, and standard of care otolaryngologic principles. Stratification of the strength of evidence for each citation is included in the reference section.4
BLAST MECHANICS
An explosion is caused by unstable chemical material that undergoes a rapid and self-propagating exothermic reaction resulting in near-instantaneous expansion of a solid or liquid to a gaseous state. This chemical reaction is accompanied by high temperatures, massive shock, and loud acoustic noise, termed a detonation. The strength of detonation is variable based on the mass and chemical characteristic of the base substance.Reference Langworthy, Sabra and Gould5
Explosive detonation in an open space releases a sphere of high-pressure gases that expand from the point of detonation. This results in compression of the surrounding atmosphere generating an overpressure phenomenon expanding in all directions, or blast wave.Reference Born2Reference Wightman and Gladish6 The leading edge of the blast wave creates a rapid positive pulse or a shock wave that delivers a destructive brisance or shattering effect to objects in its path. The shock front is followed by a short positive pressure wave or blast wind (Figure 1). As air is sucked back into a relative vacuum created at the blast point, a negative pressure phase results, exerting a force that is weaker compared to the positive phase but lasts 3 times as long.Reference Born2Reference Wightman and Gladish6

FIGURE 1 Components of a blast. (Modified from Reference 2.)
PATHOPHYSIOLOGY OF PRIMARY BLAST INJURY
Injuries sustained from a blast traditionally have been classified as primary, secondary, tertiary, and quaternary.Reference Zuckerman1 Primary blast injury (PBI) refers to trauma sustained from an overpressure phenomenon as the shock wave comes into contact with the body. The gas-filled organs (ear, lung, and bowel) are most susceptible to PBI. Secondary blast injuries result from collisions with energized fragments, shrapnel, or debris that are accelerated by the blast. Tertiary blast injury occurs when the body is accelerated or displaced from its position coming into contact with other objects. This occurs most frequently as the body is propelled and rolled along the ground, striking objects in its path, or it may be ejected off the ground into the air, sustaining injury on impact. Severe tertiary blast injury results in blunt trauma and/or traumatic amputations. Quaternary injuries are those injuries sustained indirectly as result of the blast such as burn injury, inhalation injury, or crush injury sustained with structural collapse.Reference Zuckerman1Reference Chaloner7Reference Sasser, Sattin, Hunt and Krohmer8
Large blasts resulting in mass casualties frequently result in multisystem trauma, the majority of which are due to secondary, tertiary, and quaternary mechanisms. As in any trauma, these injuries must be quickly triaged, and critical patients treated promptly with lifesaving measures. Standard trauma protocols are initiated, putting first priority on airway, breathing, and circulation (ABC).
PBIs, however, are often more subtle and may be overlooked, especially in mass casualty events. Injury to the gas-filled organs of the body is sustained when the shock wave of a blast comes into contact with the human body. Complex interactions proceed at the body surface where pressure differentials develop. As a blast front reaches the body traveling at speeds potentially exceeding the speed of sound, a “blast loading” phenomena results in rapid acceleration at the body surface, creating stress waves that run through the underlying soft tissues.Reference Wightman and Gladish6Reference Stuhmiller, Phillips and Richmond9Reference Mellor10 The speed of sound in air (343 m/s, at sea level) exceeds that of soft tissues in the body (40 m/s), resulting in large pressure differentials at air soft-tissue interfaces.Reference Clemedson and Jonsson11Reference Cooper and Taylor12Reference Mrena, Paakkonen, Back and Pirvola13 Rapid implosion of the gas-containing organ is followed by traumatizing re-expansion. Sheering forces caused by differential acceleration and decelerations in tissues of variable densities result in evulsions and lacerations of internal organs, particularly at fixed attachment points.Reference Zuckerman1
PBI to the organs of the body tends to occur in anatomical succession, depending on the power of the blast and susceptibility of the tissues. The first organ to sustain damage is typically the ear, followed by the lungs, then the large bowel, small bowel, and (in settings of large, powerful, concussive blasts) the solid organs of the abdomen, thorax, and cranium.Reference Born2Reference Wightman and Gladish6 Injury to the lung and abdomen may result in fatal complications such as pneumothorax, hemothorax, pulmonary venous fistula, mesenteric tears, and bowel perforation.Reference Zuckerman1Reference Sasser, Sattin, Hunt and Krohmer8 Onset of PBI may have delayed presentation with silent pulmonary or abdominal injury that can be missed on initial examination.Reference Wightman and Gladish6Reference Mellor10Reference Cooper and Taylor12 The presence of PBI in the middle ear should raise suspicion of more severe occult injury and prompt cautious observation and screening protocols.Reference DePalma, Burris, Champion and Hodgson14Reference Liebovici, Gofrit and Shapira15
BLAST INJURY TO THE EAR
Injury to the delicate and sensitive structures of the middle and inner ears represents the most common type of blast injury.Reference Mrena, Paakkonen, Back and Pirvola13Reference Stien and Hirshberg16Reference Sprem, Branica and Dawidowsky18 Typical symptoms include tinnitus, otalgia, hearing loss, and vertigo. The mass casualties and multisystem traumas encountered from blast injuries appropriately require rapid assessment and transport of patients from the field to emergency medical facilities. Because highest priority is applied to diagnosis and treatment of life-threatening injuries, otologic injury is often missed; however, with simple screening protocols, limited management, and appropriate otolaryngologic referral poor outcome and morbidity can be minimized.
External Ear
Injury to the soft tissue of the ear is caused primarily by secondary, tertiary, and quaternary blast injuries. Common injuries include lacerations, abrasions, contusion, thermal damage, and evulsions.
Tympanic Membrane
The tympanic membrane is exquisitely sensitive to variations in atmospheric pressure as it functions to transmit minute pressure oscillations encountered by impulsive and continuous sound waves. Blast overpressure enters the external auditory canal stretching and displacing the tympanic membrane (TM) medially. Pressures greatly exceed that of impulsive or continuous noise. A spectrum of injury may be observed as the elastic and compliant properties of the TM are overwhelmed. Injury may range from intratympanic hemorrhage in minor cases to total tympanic membrane perforation in powerful blasts (Figure 2). Perforations may be unilateral or bilateral, small or complete, and single or multiple. The shape of the laceration may be smooth and linear, punched out, or ragged with the edges inverted or everted. The location of lacerations is almost exclusive to the pars tensa and only infrequently involving the pars flaccida.Reference Garth19Reference Kerr and Byrne20

FIGURE 2 Normal and perforated right tympanic membrane. Normal tympanic membrane and corresponding anatomic landmarks (left). Subtotal traumatic perforation depicting irregular perforation with exposed middle ear, surrounding blood clot, and burn (right).
A limited number of animal and human studies have demonstrated the physical limits of the tympanic membrane resulting in perforation.Reference Richmond, Fletcher, Yelverton and Phillips21Reference Zalweski22Reference Blake, Douglas, Krohn and Zuckerman23Reference Hirsch24Reference White, Bowen and Richmond25 In 1906, Zalweski conducted experiments on fresh cadeveric eardrums. He reported that minimal and maximal pressures of TM rupture resulted at 5.4 and 43 psi, respectively, with mean pressure of 23 psi. There was little difference between male or female subjects or left or right ears. There was a higher incidence of rupture at lower pressures with elderly adults and scarred, thinned, or inflamed ears.Reference Richmond, Fletcher, Yelverton and Phillips21Reference Zalweski22 Kerr observed that children in the same proximity to blasts were able to avoid perforations that were otherwise sustained by adults, suggesting that the pediatric tympanic membrane is more compliant and resistant to perforation.Reference Kerr and Byrne20
The vector at which the concussive wave approaches the head will have variable effect on TM trauma. Experiments have shown that a shock wave that passes the head in an anteroposterior vector produces a lower peak overpressure at the TM than a wave with a lateral-to-medial incident vector.Reference Richmond, Fletcher, Yelverton and Phillips21Reference James, Pickett, Burdett and Cheesman26 Thus, a blast detonated to the side of an individual places the subject at greater risk for ipsilateral TM rupture than if it were detonated directly in front of the person. Studies also suggest a shadow phenomenon, in which the contralateral ear is protected by the head as the incident wave of the blast front passes around the subject.Reference Richmond, Fletcher, Yelverton and Phillips21Reference James, Pickett, Burdett and Cheesman26
Middle Ear
Injury to the middle ear structures also occur with blast trauma. Disruption of the ossicular chain is reported with varying incidence. Kerr and Byrne and Pahor reported no injury to the auditory bones among 92 individuals,Reference Kerr and Byrne20Reference Pahor27 whereas Singh and Ahluwalia reported 4% incidence in their series.Reference Singh and Ahluwalia28 In larger blasts, the incidence of ossicular damage appears to be more common. Chandler et al present case studies in which 4 of 5 soldiers had ossicular damage in 5 of 10 ears, after a large explosive device was detonated prematurely.Reference Chandler and Edmond29 The men were exposed to overpressures in excess of 200 dB (85 psi), suggesting that larger blast pressures result in higher incidence of ossicular disruption.
Blast-related TM perforations have been associated with increased incidence of cholesteatoma, or keratoma, within the middle ear and mastoid cavity. Cholesteatomas are potentially destructive lesions that can erode and destroy important structures of the middle ear, temporal bone, and base of the skull. Sequelae of disease can cause conductive and sensorineural hearing loss, vestibular disturbances, cranial nerve palsy, as well as central nervous system complications (eg, brain abscess, meningitis), making it a potentially fatal lesion. Traumatic implantation of epithelial debris and subsequent proliferation of squamous epithelial tissue within the tympanic cavity is the proposed mechanism of traumatic cholesteatoma formation. Seamon et al reported a 12% incidence of squamous epithelium in the middle ear from a series of 110 Vietnam war veterans with blast-related TM perforations.Reference Seaman and Newell30 In another consecutive series of 147 patients by Kronenberg and colleagues, a 7.6% incidence of cholesteatoma in 210 ears were observed.Reference Kronenberg, Ben-Shoshan, Modan and Leventon31 Furthermore, the incidence of cholesteatoma increases with larger perforation size and central location. In the same study, 2 cholesteatomas were observed in the middle ear after spontaneous healing of TM perforation with conservative management. These were observed at 10 and 22 months.
Inner Ear
Damage to the auditory and vestibular components of the inner ear are also observed in blast injury. The typical patient with blast injury will experience a temporary hearing threshold change defined as a sudden profound sensorineural hearing loss and/or tinnitus that is transient and self-resolving in nature. Most regain hearing within hours; for others resolution is slower, after days to weeks. A smaller portion of individuals are left with permanent hearing loss and tinnitus.Reference Mrena, Paakkonen, Back and Pirvola13Reference Cohen, Ziv, Bloom, Zikk, Rapoport and Himmelfarb17Reference Kerr and Byrne20Reference Chandler and Edmond29Reference Miller, McGahey and Law32
The mechanism of hearing loss can be conductive, sensorineural, or mixed with conductive loss attributed to TM perforation and ossicular damage. The mechanisms of sensorineural hearing loss or transient threshold changes are thought to be due to traumatic changes to the reticular lamina of the organ of Corti, which results in changes in the permeability of electrolytes over the membrane altering the endolymphatic milieu. As the reticular lamina regenerates, hearing and tinnitus symptoms generally resolve. Permanent hearing loss has been attributed to irreversible hair cell damage and detachment of segments of the organ of Corti according to findings on electron microscopy.Reference Hamernik, Turrentine, Roberto, Salvi and Henderson33Reference Roberto, Hamernik and Turrentine34
Vertigo is considered a rare complication of blast injury and has been more commonly attributed to secondary or tertiary mechanisms that cause concussive injury to the central nervous system, rather than inner ear damage.Reference Kerr and Byrne20Reference Pahor27 Peripheral vestibular etiologies to consider include benign paroxysmal positional vertigo (BPPV), perilymphatic fistula, and acute trauma to the utricle and saccule of the inner ear.Reference Cohen, Ziv, Bloom, Zikk, Rapoport and Himmelfarb17Reference Kerr and Byrne20Reference Pahor27Reference Singh and Ahluwalia28
BPPV in patients with blast injury is thought to be a result of canalithiasis, a process in which free-floating densities are dislodged within the perilymphatic fluid of the semicircular canals. These canaliths exert a force upon the cupula of the crista ampularis that is paradoxically perceived as motion. Symptoms are typically elicited with sudden head or body movements resulting in vertigo and nystagmus lasting only seconds to minutes and resolving with discontinuation of the motion.
Vertigo in the setting of unstable, fluctuating, or worsening sensorineural hearing loss may suggest a perilymphatic fistula, a pathologic communication between the middle ear and the vestibular structures. The disregulation of perilymphatic pressures results in intermittent disequilibrium and senorineural hearing loss.
Temporal bone autopsies of blast victims have found rare cases of utricle and saccule disruption suggesting another possible peripheral vertiginous cause.Reference Cohen, Ziv, Bloom, Zikk, Rapoport and Himmelfarb17Reference Pahor27
ASSESSMENT AND MANAGEMENT OF BLAST EAR INJURY
Initial Examination by Emergency Care Providers
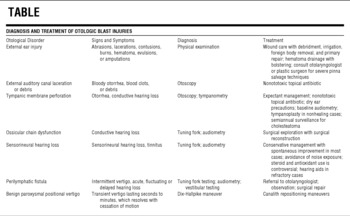
A basic history and examination by emergency care personnel can be used to screen blast victims for otologic sequelae quickly. History should include an assessment of hearing loss, ringing, pain, ear discharge, and vertigo. An otoscope and a tuning fork are used in the physical examination. The otoscopy provides a magnified assessment of the external auditory canal and TM. Lacerations, burns, fluids, or foreign body material may be observed in the external auditory canal. TM perforations or effusions are signs of middle ear trauma. Tuning fork examination using Weber and Rinné tests provides a gross assessment of hearing and differentiation between conductive and sensorineural hearing loss. Finally, facial nerve function also should be documented (Table).
TABLE 1 Diagnosis and Treatment of Otologic Blast Injuries
Screening for Primary Blast Injury
Standard trauma protocols and lifesaving measures should always be addressed first in the assessment and management of patients with blast injury. After basic lifesaving measures and severe injuries have been addressed, a focused secondary examination should include otoscopic evaluation of the TM and external auditory canal. DePalma et al suggest that careful examination by handheld otoscopy can provide valuable information with regard to patient risk for other primary blast injury. Despite its poor sensitivity, TM perforation raises suspicion for occult PBI to the lung and abdomen, which notoriously have late-onset presentation.Reference DePalma, Burris, Champion and Hodgson14Reference Liebovici, Gofrit and Shapira15 Because of potentially fatal complications associated with visceral PBI, a screening and observation protocol is recommended.
Victims presenting with isolated TM perforation without evidence of further trauma should be observed for a 6- to 8-hour period with oxygen saturation monitoring and a screening chest x-ray to rule out occult PBI. Patients who remain symptom free may be discharged with abdominal and pulmonary precautions, whereas those with positive radiological findings or who become symptomatic are to be treated with supportive measures.Reference DePalma, Burris, Champion and Hodgson14Reference Liebovici, Gofrit and Shapira15
Patients with an intact TM in the absence of respiratory or abdominal complaint are ruled out for PBI. Exceptions to consider include pediatric patients who were in close proximity to the blast or individuals with cerumen impaction of the external auditory canal. These patients are relatively protected from TM perforation. Children have been shown to have a remarkably compliant TM and cerumen impaction can function like earplugs in the external auditory canal.Reference Kerr and Byrne20Reference Richmond, Fletcher, Yelverton and Phillips21 Therefore, a 6-hour observation period with chest x-ray and oxygen saturation monitoring may be warranted to rule out occult PBI in these individuals.
External Ear
Injuries of the external ear are managed like other soft tissue injuries. Strict attention is given to foreign body removal, cleaning and irrigation of wounds, and repair of lacerations. Auricular hematoma is to be drained and bolstered. Soft tissue defects are to be repaired primarily when auricular cartilage is exposed.
For cartilage degloving with soft tissue loss or amputations, burying the exposed or devascularized tissue in a postauricular pouch may salvage the pinna cartilage.Reference Garth19Reference Miladick and Carraway35 In the case of an amputated pinna, the skin is either denuded or dermabraded and the amputation is primarily repaired. The tissue is then buried in a postauricular pouch to avoid tissue necrosis (Figure 3). After 2 to 3 weeks the buried pinna is removed from the pouch and either skin grafted or allowed to epithelialize secondarily. This procedure may require consultation with an otolaryngologist or a plastic surgeon.

FIGURE 3 Postauricular pouch for salvage of degloved cartilage or avulsed pinna. Injury resulting in pinna avulsion with exposed cartilage. Local wound care is performed. A postauricular pocket is created with an incision in the postauricular sulcus and subcutaneous undermining over the mastoid. The devascularized tissue is denuded or dermabraded with attention to preserving the periosteum. Tissue and cartilage is then primarily repaired and buried within the pouch to avoid necrosis and tissue loss.
Middle and Inner Ears
Tympanic Membrane Perforation
Treatment of TM perforations is typically expectant. If the eardrum is not visible because of cerumen impaction or blood clots, then the perforations can be carefully suctioned and cleaned by an otolaryngologist. When a specialist is unavailable the ear should be kept clean and dry with appropriate referral. Nonototoxic antibiotic eardrops are indicated for TM perforations or ear canal lacerations, which help to irrigate and clear the canal of debris.Reference Garth19 Ototoxic topical ear drops, including aminoglycoside preparations, are rarely associated with hearing loss or vestibular dysfunction in the setting of middle ear perforations and are generally avoided in favor of quinilone preparations such as ciprofloxin or ofloxacin.Reference Roland, Stewart and Hannley36
Small- to moderate-size TM perforations typically have an excellent prognosis with spontaneous resolution in the majority of cases.Reference Garth19Reference Kerr and Byrne20Reference Pahor27 For irregular perforations with everted TM flaps, realignment may improve the chances of healing. Perforations most frequently resolve in the first 3 months after injury. Tympanoplasty is indicated if spontaneous resolution is not observed after close observation, although some debate exists about the optimal timing of the procedure.Reference Sprem, Branica and Dawidowsky18Reference Kronenberg, Ben-Shoshan, Modan and Leventon31Reference Gapany-Gapanavicius, Brama and Chisin37 Any ear drum perforation runs the risk of cholesteatoma formation, especially those that are larger and do not resolve spontaneously. Follow-up to screen for potential cholesteatoma formation is indicated biannually for a minimum of 2 years in these patients.Reference Garth19Reference Kronenberg, Ben-Shoshan, Modan and Leventon31Reference Cripps, Glover and Guy38
Hearing Loss
Baseline audiometry in all patients with blast injury has been advocated because hearing deficits are common and not always noted by patients.Reference Garth19 Conductive hearing loss suggests middle ear pathology such as TM perforation, middle ear effusion, or ossicular chain dysfunction. TM perforation and middle ear effusion are treated expectantly, with spontaneous resolution in most cases. Repair by a qualified otologic surgeon is indicated in the setting of ossicular discontinuity with significant conductive hearing loss.
There is no proven treatment for patients with sensorineural hearing loss. Controversy exists about the use of systemic steroids in this setting. Advocates for treatment generally recommend a short tapered dose in patients without contraindications, although there is no consensus on dosage.Reference Cope and Bova39 Benefit may be derived from antioxidant therapy in cases of acute sensorineural hearing loss, but, again, supporting evidence for this claim is deficient.Reference Durrat, Ahmad, Seidman and Seidman40 Auditory precautions are recommended because there is evidence that avoidance of further auditory insult results in higher recovery rates.Reference Argyros41Reference Melinek, Naggan and Altman42
Interval audiometric evaluation is standard when documenting hearing loss and in recovery. Most cases resolve spontaneously; however, in cases of persistent sensorineural hearing loss, hearing aids or other amplification devices may be indicated.
Vertigo
Dizziness in blast victims is rarely due to inner ear dysfunction, with the majority of cases attributed to central causes. Dizziness, imbalance, and vertigo are transient in the majority of cases, resolving spontaneously. On initial examination, the clinician should screen patients for sensorineural hearing loss using a tuning fork. A patient with fluctuating sensorineural hearing loss in the presence of vertigo raises clinical suspicion for perilymphatic fistula and should be evaluated by an otolaryngologist. In many cases a fistula will resolve spontaneously; however, in cases of persistent perilymphatic leak, exploration and repair may be indicated to preserve hearing and to improve debilitating symptoms.Reference Garth19
BPPV is the most common type of vertigo in the setting of trauma. It is diagnosed using the Dix-Hallpike maneuver, in which a person is leaned back from a sitting to a supine position, with the head turned 45° to the right or left side and extended about 20°. Positive tests classically show rotary nystagmus. BPPV can be treated successfully in approximately 80% of patients with canalith repositioning maneuvers including the Epley (Figure 4) and Semont maneuvers.Reference Herdman, Tusa, Zee, Proctor and Mattox43

FIGURE 4 The Epley maneuver for benign paroxysmal positional vertigo is a 5-step process. Between each maneuver there is a 30- to 60-s pause to allow for canalith repositioning and resolution of vertiginous symptoms. It begins with the patient in an upright position (A). The patient is briskly laid back into a supine position with the neck extended and turned 45° toward the affected ear (B). The head is then turned to the opposite side with the unaffected ear facing down (C). The head and body are turned further in the same direction with the face positioned down (D). The clinician then briskly returns the patient to a seated position (E). Patients are instructed to remain in an upright or semirecumbent position for 24 h to maintain the head in a vertical position after the procedure.
Blast-injured victims with persistent vertigo in excess of 2 weeks and fluctuation or deterioration of hearing need to see an otolaryngologist for a complete audiovestibular evaluation.
CONCLUSIONS
Blast injury has become increasingly common, requiring preparedness, training, and planning for all medical personnel. Otologic complaints are among the most common symptoms of blast victims. Simple otoscopic evaluation is an essential element in the initial assessment of every victim. The presence of tympanic membrane perforation raises suspicion of occult injury, prompting further workup to rule out blast lung or abdominal injury. Simple treatment and appropriate referral for audiometric and otolaryngologic evaluation are indicated in blast-injured patients exhibiting symptoms of hearing loss, ear pain, drainage, tinnitus, or vertigo.
Each reference below has been evaluated by strength of evidence as follows4:
• Level 1, randomized controlled trials
• Level 2, prospective cohort studies
• Level 3, case control studies
• Level 4, retrospective case series
• Level 5, expert opinion without explicit critical opinion, animal research, or based on basic science physiologic principles







