The 2014 Ebola virus disease (EVD) outbreak in West Africa was the largest in history with over 28,000 cases. 1 In September 2014, the first domestically acquired EVD cases in the United States were 2 nurses at a Texas hospital who treated an EVD patient who had recently traveled from an Ebola-affected country in West Africa.Reference Chevalier, Chung and Smith 2 These EVD cases heightened concern over vulnerabilities in health care preparedness across the United States and highlighted the need for serious communicable disease training across health care systems to ensure health care workers’ safety. Serious communicable diseases include highly contagious diseases that may: (1) have severe health outcomes and/or high case fatality rates, (2) require public health intervention to prevent or mitigate the spread of disease, and (3) require critical infection prevention precautions for health care workers. These diseases include plague, smallpox, viral hemorrhagic fevers (eg, EVD), and other highly infectious diseases (eg, measles). 3
EVD is a highly fatal disease and signs and symptoms include fever, vomiting, diarrhea, muscle pain, and headache. The incubation period can range from 2 to 21 days. EVD is transmitted through direct contact with blood or body fluids (eg, feces, vomit, or saliva) of a symptomatic infected person or with objects that have been contaminated with infectious blood or body fluids. A cure for EVD does not currently exist, although vaccines and antiviral drugs are being developed.Reference Pavot 4 , Reference Trad, Naughton and Yeung 5 Health care workers treating EVD patients are at particularly high risk of infection, especially when proper personal protective equipment (PPE) and infection control practices are not used. 6 , 7 According to Centers for Disease Control and Prevention (CDC) guidance, PPE recommendations vary based on if the patient is “wet” (eg, exhibiting vomiting or diarrhea) or “dry.” CDC recommends a disposable fluid-resistant gown or coverall, disposable gloves with extended cuffs, disposable facemask, and a disposable full face shield for dry patients. For wet patients, CDC recommends a disposable impermeable gown or coverall, disposable gloves with extended cuffs, disposable boot covers, disposable apron, and a powered air purifying respirator or N95 respirator. 8 , 9
Georgia was at the epicenter of the domestic EVD response during the 2014 outbreak due to being home to one of the first EVD Treatment Centers in the United States, the CDC, and to Hartsfield-Jackson Atlanta International Airport (Hartsfield-Jackson). CDC deployed thousands of its employees to assist with the EVD response in West Africa and Hartsfield-Jackson was 1 of 5 airports in the United States designated to screen travelers from EVD-affected countries. As a result, the Georgia Department of Public Health (DPH) monitored 2960 travelers returning from EVD-affected countries. Active monitoring required travelers to report their temperature and any symptoms to DPH once a day for 21 days from the date of departure from the EVD-affected country.Reference Stehling-Ariza, Fisher and Vagi 10 , 11 If a monitored traveler developed signs or symptoms compatible with EVD during the 21-day monitoring period, the traveler was considered a person under investigation (PUI), and a DPH medical epidemiologist conducted an evaluation assessment to determine whether the PUI needed a medical evaluation at a hospital and transport to the hospital using emergency medical services (EMS). 12 Consequently, a critical component of DPH health care preparedness and response planning for EVD was to ensure health care workers, including EMS personnel, were trained in appropriate PPE and infection control for suspected or confirmed EVD patients.
To address preparedness gaps, between August 2014 and March 2015, DPH conducted a needs assessment of the EVD preparedness of Georgia hospitals and EMS providers (ie, ambulance services) and developed the Infectious Disease Network (IDN). The IDN is a network of hospitals and EMS providers that are specially trained to mount a coordinated response and utilize appropriate PPE and infection control procedures in the event that a PUI for EVD or any serious communicable disease needs a medical evaluation and/or transport. The purpose of this paper is to: (1) present results of the EVD preparedness needs assessment, (2) describe the development and use of the IDN to transport and medically evaluate PUIs in Georgia during the EVD outbreak in West Africa, and (3) present data on PUI medical evaluations and clinical diagnoses.
METHODS
Needs Assessment
DPH performed a needs assessment of hospitals, EMS providers, and the PUI transport and medical evaluation coordination process during August-October 2014 to: (1) identify the number and location of EMS providers in Georgia with PPE for EVD, (2) estimate the prevalence of EMS and hospital personnel trained on PPE usage for EVD, and (3) identify weaknesses of the PUI transport and medical evaluation coordination process. Results of the needs assessment informed the development of the IDN.
The hospital needs assessment collected qualitative information about the prevalence of hospital personnel with PPE training for EVD through e-mail and in-person exchanges with hospital leadership at the 14 regional health care coalitions in Georgia and the Georgia Hospital Association, a non-profit association of hospitals. Health care coalitions are regional multi-agency groups comprised of health care facilities, health care organizations, and emergency management planners that coordinate preparedness and response for disasters and other emergencies that affect health care facilities. Most health care facilities in Georgia are members of a health care coalition and/or the Georgia Hospital Association.
For the EMS needs assessment, a quantitative survey that asked about available disposable coveralls on ambulances or elsewhere in the county was distributed by 10 Georgia regional EMS directors to EMS providers in their region. Other recommended PPE equipment for EVD (eg, gloves, facemask, and N95 respirators) were already a requirement for all ambulances in Georgia. EMS survey results were aggregated by county. Qualitative information was also gathered through e-mail and in-person exchanges with leaders at the DPH Office of EMS and Trauma (Office of EMS) and review of the National EMS Education Standards used to train Georgia EMS personnel to estimate the prevalence of EMS personnel trained on PPE usage for EVD. For the needs assessment of the PUI transport and medical evaluation coordination process, DPH medical epidemiologists were asked about challenges experienced when attempting to coordinate medical transport and evaluation for PUIs.
IDN Development
Between October 2014 and March 2015, DPH developed the IDN network of hospitals and EMS providers to guide, train, and support proper PPE use and infection control procedures for health care workers.Reference Lundstrom, Pugliese and Bartley 13 , Reference Scheckler, Brimhall and Buck 14
The IDN core planning team was comprised of senior-level staff at DPH that oversee the monitoring, transport, and evaluation of PUIs and consisted of 7 members from Epidemiology, the Office of EMS, and Emergency Preparedness and Response. The Office of EMS led the effort to coordinate EMS providers for the network. Hospital participation in the network was coordinated by DPH with assistance from health care coalitions and the Georgia Hospital Association.
Hospital Network Development
DPH adopted a tiered approach to the development of the IDN hospital network modeled on trauma system development which had previously occurred in Georgia. This tiered approach was compatible with guidance from CDC recommending that acute health care facilities be designated as either frontline health care facilities (Tier 3), EVD assessment centers (Tier 2), or EVD treatment centers (Tier 1). 15 The IDN capabilities required for each tier were presented at weekly EVD conference calls open to all health care personnel in Georgia beginning in September 2014.
Between October 2014 and March 2015, of the 105 acute care hospitals in Georgia, 17 hospitals volunteered to be evaluated as an assessment or treatment center and were evaluated through site visits by DPH staff, in collaboration with CDC, according to an assessment tool provided by CDC covering 11 EVD preparedness domains. To be designated as an IDN treatment or assessment center, hospitals had to demonstrate EVD capabilities for care of an EVD patient in facility/patient room infrastructure, patient transportation (ie, interfacility and intrafacility), laboratory safety, staffing, staff training, PPE, waste management, worker safety and health monitoring, environmental infection control, clinical competency, and operations coordination and communcation. 16 , 17 Hospitals were provided with the assessment tool and prepared accordingly before their evaluation. To become a designated EVD assessment center, a facility had to have the capability to safely collect laboratory specimens (ie, blood and urine) for EVD diagnostic testing and to care for an EVD positive person for up to 96 hours. To be a treatment center, hospitals had to meet the same competencies of an assessment center and, in addition, be capable of treating an EVD case until the patient is EVD free, which on average is 22 days.Reference Rainisch, Asher and George 18 Assessment or treatment centers were not required to have the capability to perform on-site routine laboratory testing or EVD diagnostic testing of PUI specimens. Although not required, all treatment centers had on-site laboratories capable of safely processing specimens for routine laboratory testing for a suspected EVD case. If an assessment center did not have laboratory capability for safely processing PUI specimens, the specimen could be sent to a designated treatment center for routine laboratory testing. EVD diagnostic testing for all PUI specimens was performed by the Georgia Public Health Laboratory. The DPH Director of Health Protection provided final approval of hospital designation as an assessment or treatment center based on the evaluation results. All assessment and treatment centers received federal funding administered by DPH to specifically support maintenance of facilities, equipment, and training needed for care of a PUI or confirmed EVD patient. However, all treatment or assessment centers had the option to decline receipt of a PUI based on the operating capabilities on a given day.
Any health care facility that could encounter an ill traveler, and was not a designated assessment or treatment center, was required to be a frontline facility. Frontline facilities and responders included hospitals, private physician practices, urgent care facilities, nursing homes, school nurses, fire, EMS, and law enforcement. Frontline facilities/responders were asked, at a minimum, to be able to “identify, isolate, and inform”: to identify patients with recent travel history to an EVD-affected country and EVD-compatible symptoms; to isolate these patients in a private room and minimize staff exposure; and to inform the hospital infection control practitioner and DPH using 1-866-PUB-HLTH, Georgia’s 24/7 public health phone line. 19 , 20 DPH disseminated guidance on “identify, isolate, and inform” to hospitals and health care providers through health care coalitions, the Georgia Hospital Association, and other professional and government associations via e-mails and in-person meetings.
EMS Network Development
On October 30, 2014, the Office of EMS leadership held a conference call that was open to the 278 EMS providers in Georgia to introduce the IDN and ask EMS providers to volunteer to be a part of the network. To be a part of the IDN, each EMS provider had to ensure that a minimum of 10 EMS personnel completed an Operations-Level course offered by the Office of EMS. The Office of EMS developed the Operational-Level course and a more advanced Technician-Level course to train EMS providers on proper PPE and infection control practices for EVD. The Operations-Level Course is a 1-day course comprised of classroom instruction on modes of transmission for EVD and other serious communicable diseases and hands-on modules covering practical components of transport like PPE donning (putting on) and doffing (taking off) and configuration of an ambulance for transport. The Technician-Level course is an advanced-level 2-day course that includes 1-day of classroom instruction and 1-day of practical components and drills including transport missions for a simulated IDN call. The Technician-Level course was not required for IDN participation, but was optional for EMS personnel who wanted additional training.
The Office of EMS identified a 24/7 central dispatch service that would dispatch IDN EMS providers to any location in the state. The central dispatch service was key to streamlining the coordination of transport by allowing for transport to be easily arranged by a medical epidemiologist with 1 phone call. Additionally, the central dispatch service monitored the daily availability of each IDN EMS provider to transport a serious communicable disease case.
The Office of EMS also established PPE standards and provided the same PPE to all EMS providers that were a part of the IDN to ensure interoperability between EMS personnel.
IDN Standard Operating Guide (SOG) for Medical Evaluation of a PUI
Once the IDN was fully formed in March 2015, DPH coordinated medical transport and evaluation according to the IDN standard operating guide. The IDN SOG outlined the flow of communication and roles and responsibilities of EMS personnel, the receiving hospital, and DPH (see Figure 1). The SOG also established PPE and infection control training and equipment guidelines for health care workers and EMS personnel in the network.
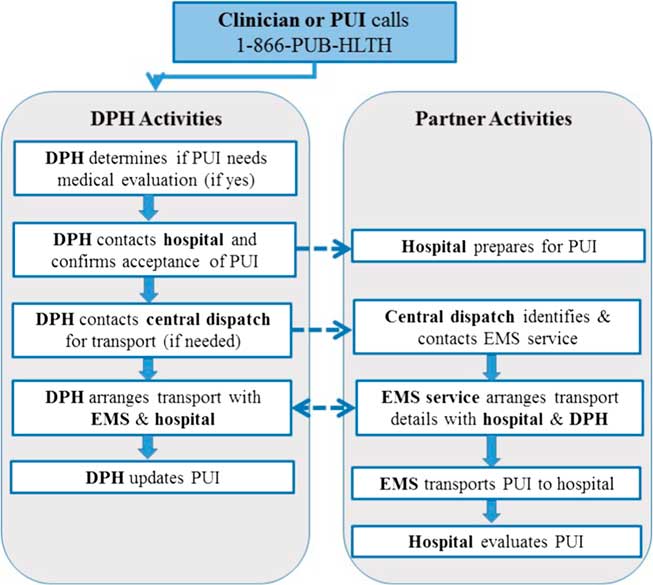
Figure 1 Responsibilities of the Georgia Department of Public Health (DPH) and Infectious Disease Network Partners for the Medical Transport and Evaluation of a Person Under Investigation for Ebola Virus Disease (PUI). Abbreviation: EMS, Emergency Medical Services.
As outlined in the SOG, a DPH medical epidemiologist determined whether a PUI needed a medical evaluation during the evaluation assessment based on the presence of EVD-compatible signs or symptoms, the severity of the signs or symptoms, and the EVD exposure risk classification.Reference Parham, Edison and Soetebier 21 CDC conducted the evaluation assessment for their employees and informed DPH of pending and performed medical evaluations. EVD-compatible signs and symptoms include fever ≥100.4°F (≥38°C), vomiting, diarrhea, muscle pain, headache, abdominal pain, and unexplained bleeding or bruising. The exposure risk categories as defined by CDC were high risk, some risk, low (but not zero) risk, and no identifiable risk. 22 The threshold for medical evaluation of some and high risk PUIs was lower than for low (but not zero) risk PUIs. PUIs presenting with fever and at least one EVD-compatible symptom were sent for medical evaluation, unless the symptoms appeared to be associated with an illness other than EVD. If symptoms appeared to be associated with another illness, PUIs were asked to self-isolate at home and DPH followed them closely until symptoms subsided or worsened. For more complicated cases, which represented around 20% of PUIs, DPH consulted with CDC to determine whether a medical evaluation was needed. The evaluation assessment by DPH medical epidemiologists, and the recommendation of home self-isolation when indicated, was critical in mitigating undue burden on the hospital resources required to coordinate and perform a PUI medical evaluation.
If medical evaluation was warranted, DPH coordinated EMS transport, if needed, and medical evaluation at the nearest IDN hospital. To reduce exposure to other persons including EMS personnel, the medical epidemiologist recommended self-transport to the hospital in a privately owned vehicle if the PUI was able. When self-transporting, the PUI was given special instructions on how to enter the medical facility in order to reduce risk of exposure to others. If the patient was unable to self-transport, the medical epidemiologist contacted the IDN central dispatch service. Central dispatch identified an appropriate IDN EMS provider and communicated to the EMS provider the patient’s pick-up and drop-off location and the type of PPE needed for the patient (ie, wet vs dry). Often, the EMS provider and receiving IDN hospital were in direct communication to arrange details of the patient’s arrival. The medical epidemiologist then communicated the estimated pick-up time to the PUI and/or the frontline contact or provider if the PUI was at a primary care facility or emergency room. The assigned EMS provider transported the PUI to the receiving hospital where the patient received a medical evaluation and specimens were collected for routine clinical laboratory testing and EVD diagnostic testing if necessary. A critical feature of the IDN SOG was a constant flow of communication between partners which included updates on estimated and actual patient pick-up time and estimated and actual patient drop-off time.
PUI Data Collection and Analysis
DPH epidemiologists and information technology specialists developed the Ebola Active Monitoring System (EAMS) to track the symptoms and temperature of monitored travelers and progress notes for symptomatic travelers (ie, PUIs) who needed a medical evaluation.Reference Parham, Edison and Soetebier 21 Data collected included demographics, travel history, exposure history, clinical symptoms, IDN transport use, clinical notes from medical evaluations, and diagnostic and treatment information. DPH and CDC jointly monitored CDC employees who had traveled to EVD-affected areas. Patient symptoms and diagnostic and treatment information were entered directly into EAMS by a DPH epidemiologist or CDC staff. For this analysis, progress notes were reviewed to determine the total number of PUIs, medical evaluations, wet or dry IDN transports, and final clinical diagnoses for PUIs. If a final or probable diagnosis was not documented, we assigned a final diagnosis based upon clinical symptoms. If a diagnosis was not documented and clinical symptoms were non-specific, diagnoses were categorized as unknown. Transport times were calculated based upon review of EMS data maintained by the Office of EMS.
RESULTS
Needs Assessment
Prior to development of the IDN, hospital leaders reported that most hospital personnel were not trained in appropriate PPE usage for EVD. Only 1 hospital within the metro Atlanta area had personnel who were trained on appropriate PPE for EVD due to the presence of a serious communicable disease unit at their facility.
For the survey of PPE available to EMS providers by county, 20 counties did not respond or did not have an EMS provider in their county and were not included in the results. Of 139 counties, 27% (37) had PPE for EVD on at least 1 ambulance in the county, 16% (22) did not have PPE on ambulances but it was available from a fire department or elsewhere in the county, and 58% (80) did not have any PPE on or available to ambulances in the county. Information gathered from leaders at the Office of EMS and review of the National EMS Education Standards used to train Georgia EMS personnel indicated that EMS personnel were not trained on how to practice appropriate infection control, including PPE use, for EVD. 23
Interviews with DPH medical epidemiologists who coordinated transport for PUIs indicated that there was not a streamlined system for coordinating transport and medical evaluation of a suspected EVD case. In order to arrange medical transport of a PUI, a medical epidemiologist had to contact 1 of 3 senior managers at the Office of EMS who would then have to identify and contact an EMS provider to arrange transport. There were no specific protocols that outlined responsibilities and communication flow between hospitals, EMS provides, and DPH to ensure a coordinated approach.
IDN Hospitals and EMS Providers
After evaluating 17 hospitals for IDN designation, in March 2015, Georgia designated 14 hospitals to be a part of the network. Nine were designated as assessment hospitals and 5 were treatment hospitals. Assessment hospitals are geographically distributed throughout the state in order to minimize travel times for PUIs. As of March 2017, 1 assessment hospital and 1 treatment hospital chose to discontinue participation in the network leaving 12 designated hospitals.
In October 2014, 17 EMS providers agreed to participate in the IDN. One EMS provider chose to discontinue participation and as of March 2017, 16 EMS providers are a part of the IDN. From November 2014 to July 2016, 281 EMS personnel completed the Operations-Level course and 38 EMS personnel completed the Technician-Level course offered by the Office of EMS.
Medical Evaluation of PUIs
Between October 25, 2014 and December 29, 2015, DPH monitored 2960 travelers (Table 1). Of these travelers, 295 (9.9%) were PUIs who reported at least 1 EVD-compatible sign or symptom during the 21-day monitoring period. Medical evaluations were performed on 40 (13.6%) PUIs at IDN hospitals. Of the 40 medical evaluations, 8 (20%) were tested for EVD and none were positive. The most common diagnoses were upper respiratory infection (25%, n=10) and gastrointestinal illness (25%, n=10). The IDN was used to transport 7 PUIs for medical evaluation. The majority of PUIs used private transportation to get to the health care facility. The time from when the initial transport request was made by the medical epidemiologist to the arrival of the PUI at the receiving hospital was, on average, 2 hours (range: 1-4 hours). The length of time the patient was in the ambulance in route to the hospital was <1 hour for all transports.
Table 1 IDN Use, Medical Evaluations, and Diagnoses of PUIs
Abbreviations: IDN, Infectious Disease Network; PUI, person under investigation for having Ebola virus disease.
a Wet—include vomiting or diarrhea.
b Dry—do not include vomiting or diarrhea.
DISCUSSION
The IDN has strengthened public health infrastructure and health care preparedness in Georgia by creating a network of specially trained health care workers. The IDN has also streamlined communication in response to a suspected or confirmed serious communicable disease case that needs medical transport, evaluation, and/or treatment. In doing so, the IDN has enhanced community preparedness and responder safety and health, critical public health preparedness capabilities outlined by CDC. 24
Challenges to Implementation
Once the IDN was implemented, communication between partners continued to be refined based on challenges encountered during previous transports or medical evaluations. The ongoing effort to maintain preparedness is resource intensive and may have contributed to 1 EMS provider and 2 hospitals choosing to no longer participate in the IDN. Another challenge is maintaining trained hospital and EMS personnel in spite of staff turnover. The criteria for EMS provider participation in the IDN seeks to address this by requiring that a minimum of 10 EMS personnel from each EMS provider complete training provided by the Office of EMS. IDN assessment and treatment hospitals also seek to maintain a core number of EVD-trained personnel through implementation of their own training protocols, which was a requirement for IDN designation.
Limitations
A formal evaluation of the efficacy of the IDN in improving coordination of PUI transport and medical evaluation and health care worker preparedness has not been performed. The needs assessment was rapidly implemented in response to an ongoing international outbreak, and as a result, some data was collected through personal communications. A small number of PUIs were medically evaluated and/or transported prior to the development of EAMS and the IDN. However, little information was available on these PUIs and, as a result, these patients were not included in our data.
Sustainability of the IDN
Ongoing training with network hospitals and EMS personnel will be critical to the sustainability of the IDN. Training for new EMS personnel and refresher training for existing personnel is held annually by the Office of EMS with IDN EMS providers across the state. IDN hospitals are responsible for the maintenance of training among their health care workers, however, training support is available through DPH and CDC. Assessment and treatment hospitals will be re-evaluated every 3 years to ensure tier-specific capabilities continue to be met. The IDN hospitals and EMS providers hold quarterly meetings with DPH to discuss best practices for maintaining preparedness capabilities for transport and treatment of serious communicable disease patients. The IDN was developed to respond to any serious communicable disease, not just EVD, which increases the long-term utility and sustainability of the IDN. The IDN has been used to transport, treat, and/or evaluate other serious communicable disease cases in Georgia, such as Middle East respiratory syndrome coronavirus (MERS-CoV) and Lassa fever. In addition, IDN development has coincided with efforts to improve overall infection control surveillance and practices in Georgia health care facilities. Supplemental federal funds for EVD were critical to the development of the IDN. These funds will be exhausted in 2017 and alternate funding sources will need to be identified to maintain IDN training and equipment needs and to expand the network.
CONCLUSION
Despite challenges during development and implementation, the IDN was successfully implemented because of strong relationships with EMS providers and health care coalitions in the state. DPH engaged partners during the conceptualization process and partners were actively engaged throughout planning. The components that were key to the operationalization of the IDN were providing training and equipment for EMS personnel, ensuring hospitals have the appropriate infrastructure and training to manage a serious communicable disease patient, establishing a central dispatch center, defining responsibilities among partners, and structuring the communication flow between partners. A major key to the success of the IDN was the buy-in and support of DPH leadership through the development and implementation process.
Widespread transmission of EVD has ceased in West Africa, although, there is always risk of EVD or other serious communicable diseases being introduced to the United States from travelers. 25 As a result, infectious disease response planning and coordination should remain a top priority for the public health and the emergency preparedness communities. Even with advanced health care systems and infrastructure in the United States, when serious communicable disease cases occur, integrated infectious disease response systems among hospitals and EMS providers will be critical to preventing or mitigating a major outbreak.
Acknowledgments
The authors thank the collaborators at CDC and the Office of the Assistant Secretary for Preparedness and Response, the health care coalitions, and the Georgia Hospital Association; all staff at the Georgia Department of Public Health who assisted with the monitoring of travelers and coordination of medical transport and evaluation. The authors also thank EMS providers and hospitals that comprise the IDN.
Disclaimer
The Centers for Disease Control and Prevention provided funding to support this publication. The conclusions, findings, and opinions expressed by authors in this article do not necessarily reflect the official position of the U.S. Department of Health and Human Services, the Public Health Service, the Centers for Disease Control and Prevention, or the authors’ affiliated institutions.




