According to the Centre for Research on the Epidemiology of Disasters (CRED), the number of natural disasters worldwide has increased roughly 4-fold in the past 25 years. 1 Additionally, the number of people affected by disasters has increased approximately 3-fold over the same period.Reference Huggel, Raissig and Rohrer 2 Disasters cause widespread life problems,Reference Westaway and Jackson 3 – Reference Ramirez and Peek-Asa 11 economicReference Huggel, Raissig and Rohrer 2 , Reference Noy 12 – Reference Mu and Chen 13 and social losses,Reference Cutter, Boruff and Shirley 14 as well as damage to the environment.Reference Enarson, Meyreles and Gonzalez 15 Of the 1.35 million people killed by natural hazards over the past 20 years, more than half died in earthquakes and the rest died due to weather and climate-related hazards. 1 Three key things are usually reported, both in academic and non-academic reports: the number of casualties, the number of people injured,Reference Ganjouei, Ekhlaspour and Iranmanesh 16 , Reference Mahue-Giangreco, Mack and Seligson 17 and the extent of structural and economic damage.Reference Noy 12 , Reference Shapira, Aharonson-Daniel and Shohet 18 Nevertheless, limited literature is available on the pattern and trends of earthquake-induced deaths and injuries.Reference Shapira, Aharonson-Daniel and Shohet 18 – Reference Smith, Roberts and Knight 20 Knowing the predicted number of deaths and injuries and knowing the patterns and trends are the most crucial factors not only for being prepared for, but also for responding to strong earthquakes effectively.Reference Shapira, Aharonson-Daniel and Shohet 18
The field of disaster epidemiology is an emerging and much needed field at present.Reference Challen, Lee and Booth 21 , Reference Mickalide 22 There are very few studies available that systematically study the impacts of disasters on human health, injuries, and deaths.Reference Challen, Lee and Booth 21 , Reference Khan, Schwartz and Johnson 23 , Reference Mitchell, Jones and Lovell 24 That notwithstanding, in the last couple of decades, some excellent studies have been undertaken by renowned researchers in the fieldReference Westaway and Jackson 3 – Reference Ramirez and Peek-Asa 11 that address the epidemiology of earthquakes. However, these studies mostly address specific parts of the world (such as developed countries) and are mainly conducted in field hospitals,Reference Bozkurt, Ocguder and Turktas 25 – Reference Bai and Liu 27 institutions,Reference Zhang, Li, Carlton and Ursano 28 and localities.Reference De Bruycker, Greco and Lechat 29 – Reference Ellidokuz, Ucku, Aydin and Ellidokuz 31 Moreover, they do not consider the overall deaths and injuries in the event of an earthquake.
A systematic review conducted by Blanchet et al.Reference Blanchet, Sistenich and Ramesh 19 commissioned by Enhancing Learning and Research for Humanitarian Assistance (ELRHA) revealed that only 47 articles focus on injuries and rehabilitation in the context of humanitarian crises, including earthquakes. After applying STROBE criteria, they found 2 articles only.Reference Blanchet, Sistenich and Ramesh 19 This highlights how scarce the literature is in the domain of injury and rehabilitation regarding humanitarian crises, including mega earthquakes. It is necessary to study the effects of a disaster on health and identify the most efficient ways to prepare and respond to disasters in the context of health to save lives.
These disasters are investigable epidemiologically in 2 ways.Reference Armenian, Melkonian and Noji 7 , Reference Peek-Asa, Ramirez and Seligson 10 – Reference Ramirez and Peek-Asa 11 One uses the typical approach of studying the underlying cause of the event. This may include the study of injuries and deaths associated with the disaster itself. It is crucial to know the underlying cause of injuries and deaths so that preventive and mitigating intervention can be planned accordingly.Reference Smith, Roberts and Knight 20 The second way is to use epidemiological tools and methods to probe the mechanisms that alleviate the burden of disaster in its aftermath.Reference Blanchet, Sistenich and Ramesh 19 This may be applied at the stage of disaster preparation or during disaster relief.
More inclusive data are needed on overall disaster-induced injuries and deaths.Reference Blanchet, Sistenich and Ramesh 19 Knowing the facts and figures linked to injuries and deaths will help emergency preparedness response, planning, and recovery for a disastrous event such as an earthquake.Reference Shapira, Aharonson-Daniel and Shohet 18 – Reference Smith, Roberts and Knight 20 Unfortunately, many regions with high earthquake incidence and casualties do not have published studies in the research literature, such as Pakistan and Sumatra.Reference Shapira, Aharonson-Daniel and Shohet 18 In principle, this should include critical injuries, the cost of care, time spent in the hospital and later rehabilitation, impact on people’s mental health, impact on those whose houses were destroyed or livelihoods adversely affected, impact on those who were displaced temporarily or permanently, and any other direct human impact.Reference Shapira, Aharonson-Daniel and Shohet 18
METHODOLOGY
We retrospectively analyzed the 346 study subjects who experienced earthquake-induced injuries in the October 2015 Hindu Kush earthquake. We purposely selected 5 districts (Figure 1) in a highly seismically active area in the Hindu Kush region. In the area, more than 100,000 deaths and injuries were reported in the 2005 Kashmir earthquake. In the October 2015 Hindu Kush earthquake, more than 300 deaths and 2,000 injuries were reported. The selected districts were the most severely affected districts with the highest death toll and injuries recorded. The Hindu Kush earthquake caused death and injuries in Afghanistan and Pakistan. A total of 1,490 injuries and 232 casualties were reported after the 2015 earthquake in the Khyber Pakhtunkhwa province of Pakistan. 32
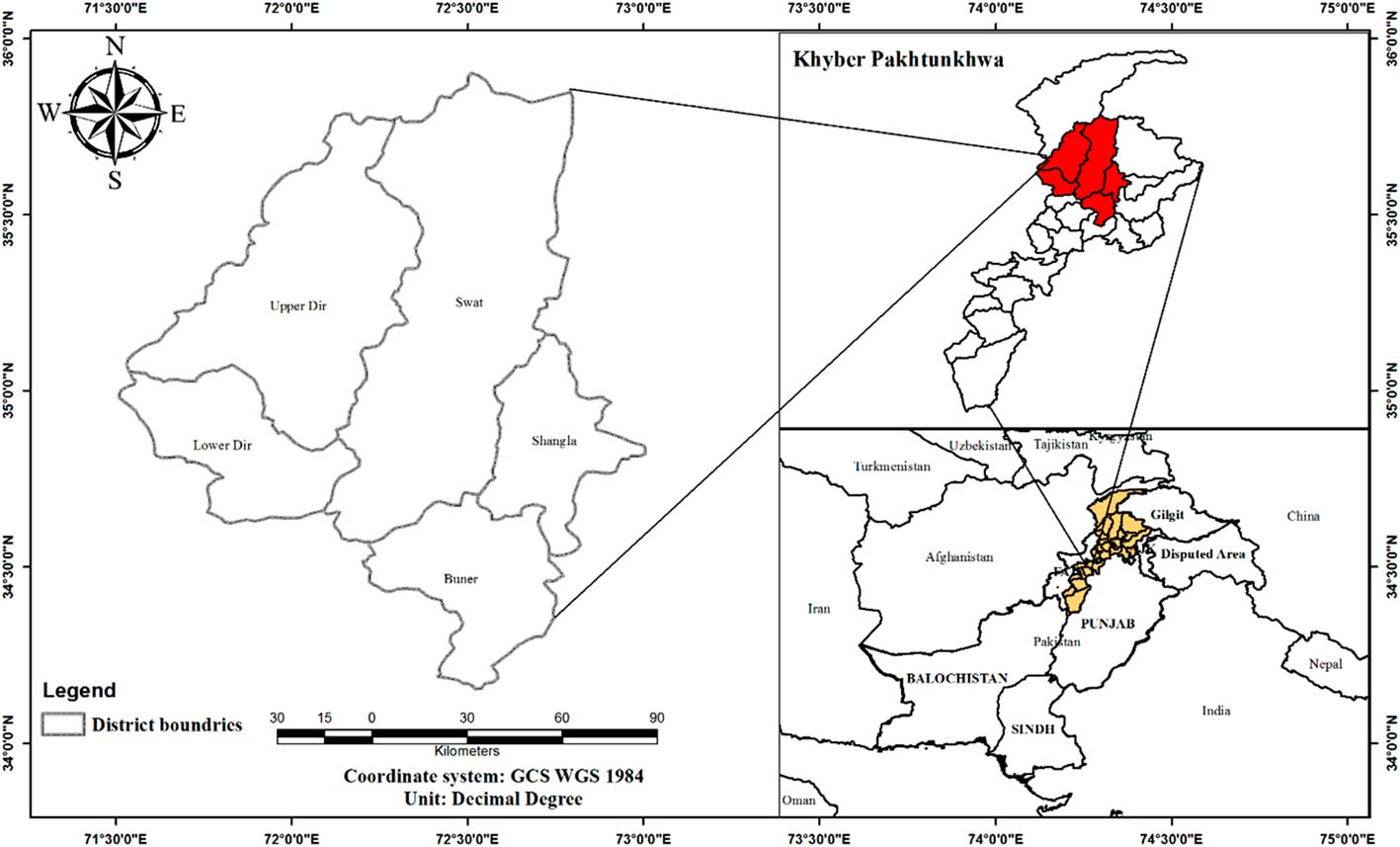
FIGURE 1 Study Area Map.
Source: Authors’ own work using open source: Esri DeLorme, USGS, and NOAA.
In our study area, in the 5 selected districts, 391 injured persons were recorded. We attempted to study all 391 individuals but could include only 346 because 45 of them were excluded either because their injuries did not correlate to the earthquake (according to a designated medical committee), complete records were not available, or they refused to participate. The data about the number of dead and injured were collected from the Khyber Pakhtunkhwa Provincial Disaster Management Authority (PDMA KP). The data included the names of injured persons only, their father’s name, their computerized national identity card number, and the Union Council (administrative unit) to which the affected person belonged. Using these data, we approached the district commissioner (the governing administrative official), who kept more in-depth data about the injured and could offer verification of the medical and physical histories of the patients and recommend compensation.
The verification of injured people was comprehensive and validated using a 2-step verification process. First, the local community leader verified that the injury was due to the earthquake. Then, a 5-member committee of medical professionals, including the district health officer, the medical superintendent of the district headquarters hospital (DHQ), the deputy medical superintendent (DHQ), an orthopedic surgeon (DHQ), and a neurosurgeon (DHQ) evaluated the nature of the injury, its severity, and its correlation with the earthquake. Using the evaluation data from this specially designated medical committee, we were able to refine our sampling of the study subjects further, and thus included only people whose injuries could be verified (by the aforementioned medical committee) as resulting from the earthquake. The most significant medical history data, such as the severity of the injury, type of injury, type of fracture, and procedure performed, were collected from the medical committee’s recommendation files. At the last stage, we interviewed the study subjects and collected sociodemographic data using a questionnaire.
RESULTS
In our study, 391 people were reportedly injured and treated in different hospitals across the study area after the October 2015 earthquake. We were able to track and collect data from 346 of these injured people. The analysis revealed that 47.97% were females and 52.03% were males (Table 1). Table 1 shows the demographic characteristics of the injured. Males were more affected than females, but the gap is not significant, and the chi-square test also justifies this. The distribution of gender is approximately equal to the chi-square test, P > 0.05. The age distribution of the injured differs, with most children affected. The second highest affected age demographic after children was the age group of 30–44 years, or middle-aged adults. The chi-square test confirms this with P < 0.001. Similarly, the most affected regarding marital status were married and single; in fact, there is a significant difference in the chi-square test with P < 0.001. The majority of the families had between 5 and 9 members. The chi-square test confirms the uneven distribution in family size with P < 0.001. Family sizes greater than 15 were very rare.
TABLE 1 Demographic Profile of Persons With Earthquake-Induced Injuries

These findings are not significantly different from the previous studies conducted on the earthquakes in the United States, Latin America, and Europe, and even in Asia. Phalkey et al.Reference Phalkey, Reinhardt and Marx 33 conducted a retrospective analysis of injured people in the Gujarat (India) earthquake of 2001 and found that the gender distribution of earthquake-induced injured people treated in hospitals was uniform, with 621 (53.0%) males and 551 (47.0%) females. Other studies outside of Asia found a significant difference in the demographics of the injured regarding gender.
Ardagh et al.Reference Ardagh, Richardson and Robinson 34 conducted a study on the Christchurch earthquake in New Zealand to look into gender disparity among earthquake-induced injured people and concluded that significantly more females (71%) than males (29%) were injured during the primary and secondary shaking. Similarly, other studies from the West found a significant gender disparity among the earthquake-induced injured.Reference Peek-Asa, Ramirez and Seligson 10 , Reference Mahue-Giangreco, Mack and Seligson 17 , Reference Shoaf, Sareen, Nguyen and Bourque 35 These differences are attributable to many factors, including the difference in the infrastructure of the region, cultures, access to health care facilities, data collection, and resilience to disasters.
The data analysis reveals that the mean age of the injured persons during the earthquake was 27.60 years, whereas the youngest and oldest in years were 0.4 and 93, respectively (Table 2 and Figure 2). A systematic review conducted by Doocy et al.Reference Doocy, Daniels and Packer 36 found 31 studies that include age as a risk factor for earthquake-induced injuries. The risk of injuries with age is not well established in the literature. Ganjouei et al.Reference Ganjouei, Ekhlaspour and Iranmanesh 16 and Mahue-GiangrecoReference Mahue-Giangreco, Mack and Seligson 17 concluded that the risk of injury in earthquakes rises with an increase in age.
TABLE 2 Age Distribution of Those Injured During the 2015 Earthquake


FIGURE 2 Age Distribution of the Injured People.
Source: Field survey (2017).
In contrast, Sami found that, in the October 2005 earthquake in Pakistan, the highest number of injuries was concentrated in the age group of less than 30 years old.Reference Sami, Ali and Zaidi 37 However, Shoaf et al.Reference Shoaf, Sareen, Nguyen and Bourque 35 concluded mixed findings in 2 different areas while analyzing the injuries from the California earthquakes of 1987, 1989, and 1994.
Among the 180 males wounded during the earthquake, 65% (117) were single, 35% (63) were married, and none were widowed, whereas among the 166 females, 41% (68) were single, 51% (85) were married, and 8% (13 of 166) were widowed. We attempted to assess the relationship of family size to the risk of being injured, but due to incomplete information and confounding factors, such as the presence of all family members at home during the earthquake, the duration of the earthquake, and so on, we could not establish any association or analyze the risk of being injured about family size. However, we did carry out a descriptive analysis of the injured persons. The average family size of the injured during the earthquake was about 8, whereas the smallest and largest family sizes were 3 and 15, respectively (see Table 2; Figure 3).

FIGURE 3 Histogram Showing the Distribution of the Family Size of the Injured Persons.
Source: Field survey (2017).
The level of education of the study population in different epidemiological studies has barely been taken into consideration. This is why there is no evidence available to correlate the nature and severity of injuries with the affected person’s educational history. Mahue-Giangreco et al.Reference Mahue-Giangreco, Mack and Seligson 17 and Tang et al.Reference Tang, Zhao and Lu 38 found that the education level of the population might influence the level of seriousness of their injuries in an earthquake. We attempted to analyze the educational status of our study population. Our findings revealed that 22.8% of injured people do not have any education at all, whereas 33% have a primary-level education only.
Marano et al.Reference Marano, Wald and Allen 39 analyzed earthquake-induced deaths from September 1968 to June 2008 and concluded that 77.7% of earthquake-induced deaths were linked to ground-shaking related damage. According to So,Reference So 40 if the 316,000 officially reported deaths from Haiti’s 2010 earthquake were included, the previously reported 77.7% of deaths due to building damage would be more than 80%.Reference So 40 Similarly, Coburn and SpenceReference Coburn and Spence 41 and Marano et al.Reference Marano, Wald and Allen 39 concluded that earthquake-induced injuries and deaths are mainly due to building collapse. Consequently, knowing the type of injuries and their association with the severity of injury with building types will help the design of effective and efficient earthquake emergency-response plans.
The distribution of injured persons at various building types by gender can be seen in Table 3. Concrete block masonry in cement buildings was the most common, with about 21% of males and 29% of females injured in these buildings. Pearson’s chi-square test was used to examine the relationship between building types and the gender of those injured during the earthquake. The P value is higher than the 0.05 level of significance. Therefore, we can conclude that there is no relationship between the building type and the gender of the injured persons during the earthquake.
TABLE 3 Building Type and Gender Disparity of the Injured

Different studies across the world have studied the types of injuries induced by earthquakes in the affected population.Reference Armenian, Melkonian and Noji 7 , Reference Ganjouei, Ekhlaspour and Iranmanesh 16 , Reference Bai and Liu 27 , Reference Dhar, Halwai and Mir 42 – Reference Kuwagata, Oda and Tanaka 47 However, there are considerable variations in their classification because very few have used standard tools like the International Statistical Classification of Diseases and Related Health Problems, 10th revision (ICD 10).Reference Zhang, Li, Carlton and Ursano 28 , Reference Lu-Ping, Rodriguez-Llanes and Qi 48 To analyze the epidemiology of injuries more systematically, we used the ICD 10.
Table 4 shows the different types of injuries sustained by our study subjects. This compilation uses the broad classifications of ICD 10. We found that the highest number, 20.23% (70 of 346), of injuries in earthquakes fall into the class of “Injuries to an unspecified part of the trunk, limb, or body region (T08-T14).” It was followed by the category of “Injuries to knee and lower leg (S80-S89),” which accounted for 15.61% (54 out of 346), and “Injuries involving multiple body regions (T00-T07)” comprised 14.74% of the total injuries (51 out of 346). The details of all injuries can be seen in Table 4.
TABLE 4 Injury Classification Using ICD-10

DISCUSSION
Presently, it is widely recognized that with a growing population, more people will be exposed to devastating disasters, including earthquakes.Reference Doocy, Daniels and Packer 36 It is well documented in Third World countries because they are less resilient to disaster and suffer the most deaths/injuries per shock.Reference Kahn 49 Earthquakes are classified as the most devastating disaster regarding lives lost and injuries. 1 For this reason, there is a serious need to undertake more multidimensional studies to get an insight into the pattern of human factor damage as the result of an earthquake so that evidence-based earthquake emergency preparedness and response interventions can be designed accordingly. Until recently, only a limited number of studiesReference Shapira, Aharonson-Daniel and Shohet 18 , Reference Doocy, Daniels and Packer 36 , Reference Kahn 49 have researched the global pattern of earthquake-induced injuries and deaths, and, consequently, the findings vary greatly.
Over the past 2 decades, researchers have started analyzing the pattern and nature of disaster-induced injuries. A study by Alexander analyzed the pattern of casualties in 43 earthquakes across the globe, recorded from 1993 to 1996.Reference Alexander 6 Alexander found an annual average mortality and morbidity rate of 7,960 and 35,560, respectively.Reference Alexander 6 The study found that the ratio of death to injury was 1:4.4. In another study, Bissell et al.Reference Bissell, Pinet, Nelson and Levy 50 concluded that the death to injured ratio was 1:151 in an analysis of the earthquake in Northridge, California. Our findings also varied from the findings of AlexanderReference Alexander 6 and Bissel et al.Reference Dhar, Halwai and Mir 42 Our analysis showed that the death to injury ratio in the 2015 earthquake in Pakistan was 1:6.42.
Not only has the ratio of deaths to injuries varied in different studies from different parts of the world but so too have the patterns of injuries and the attributed socio-demographic indicators. One study on the earthquake in China by Zhang et al.Reference Zhang, Li, Carlton and Ursano 28 reported that males and females injured were 48% and 52%, respectively. Another study from China by Yang et al.Reference Yang, Wang and Zhong 51 reported that the study population of earthquake-induced injuries was 43.90% male and 56.10% female. It is crucial to note that the magnitude of the earthquakes in all of these studies did not differ much, but the human impact varied significantly. This was confirmed in our study. Therefore, it can be argued that the research findings on one earthquake may not apply to design disaster-response plans for another part of the world. This is because the geography, culture, environment, and public health capacities of all countries differ substantially.
CONCLUSION
It is a well-established fact that the number of people exposed to earthquakes is increasing rapidly just as the population itself is growing. At present and with existing knowledge, humans cannot prevent earthquakes. Fortunately, the impacts of earthquakes can be mitigated. In this regard, the first step is to understand the pattern, nature, and extent of earthquake-induced injuries and deaths. We attempted in this study to analyze an earthquake in the Hindu Kush region, a region in the most seismically active and most difficult to reach area. It is likely that this study missed some of the injured who did not approach hospitals for treatment or did not claim compensation and was consequently excluded from our sampling frame. A complete up-to-date functional demographic and updated health database would need more data and information to close the existing knowledge gap. Developing an innovative approach to recording the maximum possible amount of data for every individual affected in the event of an earthquake will be of great importance to understanding the pattern of earthquake-induced injuries and deaths. This will guide both disaster management organizations and medical professionals in planning their preparedness and response accordingly. This will be possible only if every single earthquake across the world is analyzed and the data and information are studied to develop standard operating procedures and other measures to respond to earthquakes according to demographics and geographic profiles and earthquake characteristics.
Acknowledgments
We are grateful to the government of Khyber Pakhtunkhwa, Pakistan, and the Directorate General Health Services for allowing us to access the complete District Health Information System database.
Conflict of Interest Statement
The authors declare no conflict of interest. The founding sponsors (Higher Education Commission of Pakistan) had no role in the design of the study; in the collection, analyses, or interpretation of the data; in the writing of the manuscript; and in the decision to publish the results.
Ethical Consideration
Ethical approval for this study was approved by the doctoral study research committee of the Asian Institute of Technology, Thailand. Patient consent was obtained while the interviewer administered the questionnaire.
Funding Source
The primary author is thankful to the Higher Education Commission of Pakistan for funding the author’s doctoral study. Also, many thanks are given to the University of Granada (Spain) and Erasmus Mundus for funding the research mobility collaboration between the coauthors, which otherwise would not have been possible.









