Both (a) public health and medical planning and response and (b) disaster medicine have evolved dramatically in the 16 years since the terrorist attack on September 11, 2001. Given the consequences, complexity, and public concern considered in this paper, we propose the concept of chemical, biological, radiological, nuclear, and explosive (CBRNE) science to emphasize the associated importance of (a) continued progress in the science of each of the CBRNE threats; (b) the spectrum of expertise and resources in 7 components needed for health and medical preparedness; (c) the need for integration of these components, which in itself is a skill; and (d) the characteristics of those who can integrate the knowledge and provide advice to the decision-makers during preparedness and response. Because this knowledge and expertise are critical during response operations, as is first-hand experience in planning and operations, we coin the term CBRNE medical operations science support expert (CMOSSE). The coauthors of this paper and the colleagues whose expertise we represent present the 7 core elements of CBRNE science: (1) basic and clinical sciences, (2) modeling and systems management, (3) planning, (4) response and incident management, (5) recovery and resilience, (6) lessons learned, and (7) continuous improvement. Characteristics of the CMOSSE are then presented. We are not proposing a new specialty or formal certification, but rather providing a description of a skill set to emphasize the critical need for integration among the 7 core elements and the importance of having people with this expertise working with the senior decision-makers during response operations.
The proposed terms CBRNE science and CMOSSE reflect (a) the extensive scientific experience and investment in public health and medical preparedness and response that now inform our response and recovery needs and (b) the recognition that such investment is essential to improving the efficacy of response to CBRNE incidents. The terms are valuable also to inform the public of progress made. Critically, CBRNE incident preparedness and response are best done considering the system of components, integration of common concepts among the threats, and the active avoidance of working in “silos.” An overarching main paper and a detailed electronic appendix provide both the general concepts and the details of the 7 core elements that are important to understand and implement. We are not proposing a new medical specialty or board. However, the CMOSSE includes experts from a range of sectors and we provide background information on the public health and medical emergency disciplines that will likely participate in the development and implementation of the concepts presented.
Although the CBRNE science enterprise concept and capabilities underlie official plans and responses for all 5 types of CBRNE threats, this paper, to demonstrate the critical nature of a systems approach, focuses on the largest and most complex of the national planning threat scenarios—the detonation of a 10-kiloton nuclear device in a major US city.1 While the specifics have been updated, we chose this scenario because planning for a nuclear detonation, which would be a large “no-notice” incident, has required development of a complex systematic framework. This framework could be adapted for all the other less-complex incidents and for other large-scale incidents that occur over days to weeks or longer (eg, biological incidents or a major earthquake). A related activity to establishing the CMOSSE at the operations level is in progress to establish the radiological operations support specialist, another important element to fulfill the need for threat-specific subject-matter expertise during planning and response operations.Reference Alai, Askin and Buddemeier2
The authors of this paper, both inside and outside of government, come from various disciplines. Many are well-recognized subject matter experts (SMEs) on particular aspects of public health and/or medical emergency planning and response. With respect to nuclear detonation incidents, all have contributed meaningfully to crafting and implementing plans and policies; directing basic science or clinical research activities; and/or managing medical countermeasure (MCM) development, procurement, stockpiling, and utilization planning for the US Department of Health and Human Services as it discharges its responsibilities for managing Emergency Support Function #8 (Public Health and Medical Services)3 within the Federal Interagency Operational Plans,4 a component of the National Response Framework,5 and specifically the Nuclear/Radiological Annex.6
THE 7 CORE ELEMENTS
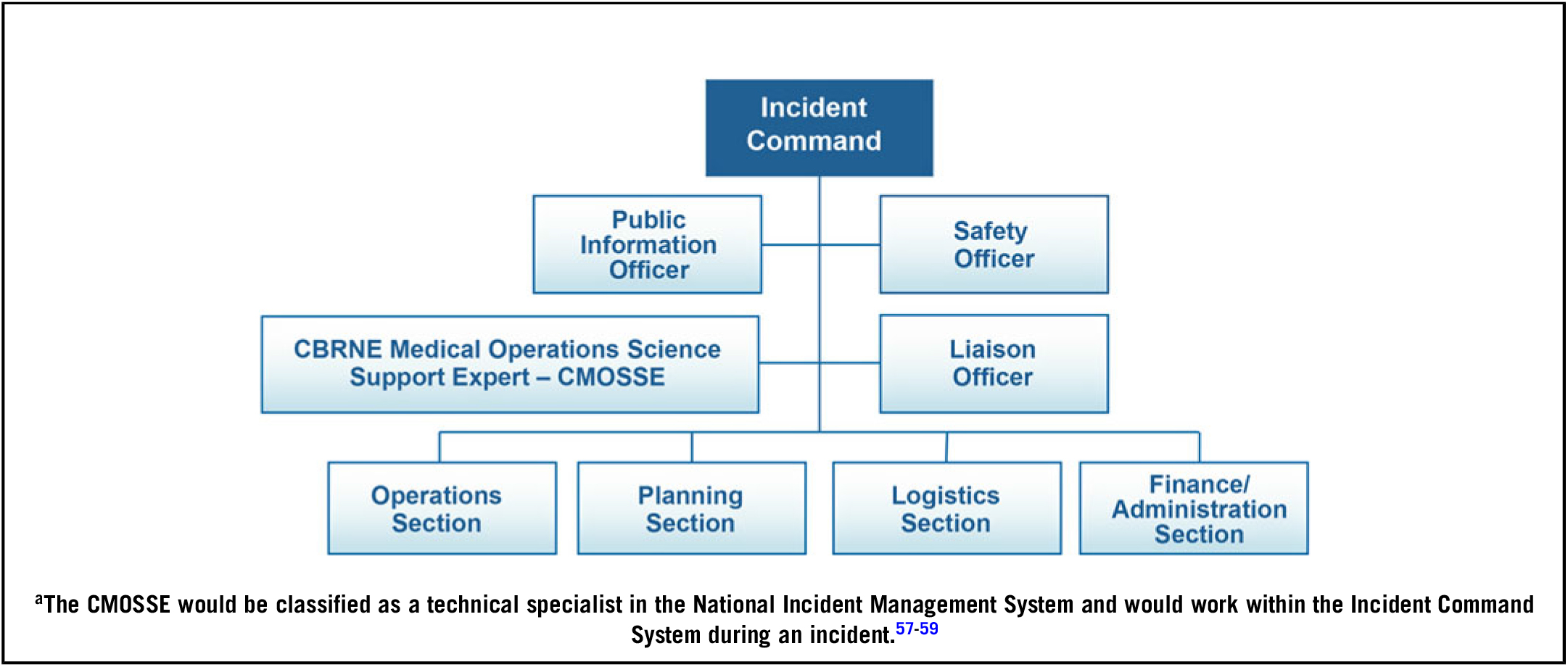
We introduce here 7 core elements of CBRNE science, represented in Figure 1. They are illustrated in a time-oriented and knowledge-based sequence compatible with the preparedness cycle,7 but in reality CBRNE science is a continuum with an interactive systems approach, which is essential to overall program efficacy. The 7 core elements are interdependent, and the order of presentation does not represent a hierarchy. Activities and outputs associated with each element affect and influence all the others. CBRNE science practitioners often have expertise that includes multiple elements.
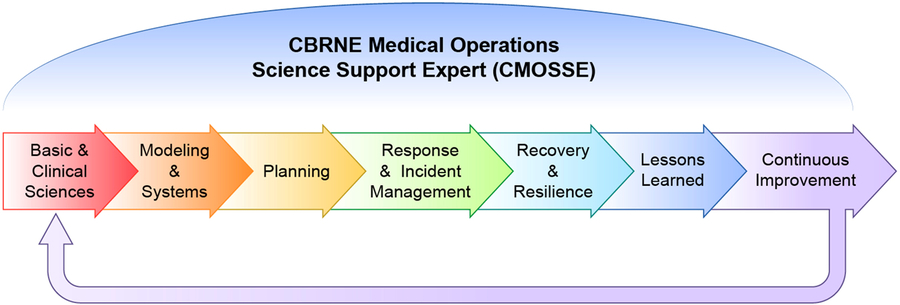
FIGURE 1 Core Elements of CBRNE Science, Overseen by the CBRNE Medical Operations Science Support Expert
CBRNE science comprises the following 7 core elements:
1. Dedication to rigorous, ongoing basic and clinical sciences, including development and plans for effective utilization of MCMs
2. Detailed modeling of CBRNE threats with a systems approach, before, during (where feasible), and after specific incidents and exercises
3. Creation and use of all-hazards plans to serve as a foundation that incorporates detailed planning modifications required for specific CBRNE threats
4. Training and deployment of sophisticated response and incident management personnel cognizant of specific CBRNE issues and the need to embed a CMOSSE near senior incident commanders and senior decision-makers early in and throughout response to an incident
5. Development of recovery and resilience plans accounting for specific CBRNE effects as well as psychosocial impacts on communities
6. Commitment to realistic and honest assessments of lessons learned both from previous incidents and from exercises
7. Commitment to continuous improvement based on new knowledge from the intelligence community and scientific and clinical medicine communities and on experience gained from exercises and actual incidents
Core Element 1
Core element 1 is dedication to rigorous, ongoing basic and clinical sciences, including development and plans for effective utilization of MCMs. Saving lives and mitigating injuries are the primary goals of a public health and medical response for any CBRNE incident. In support of these goals, basic and translational scientific research are needed both preincident and during a response. For example, current basic science strategies for understanding radiation injury include genomic, proteomic, and metabolomic inquiries; cellular- and tissue-level investigation; and animal research. Research topics include mechanisms of disease; biomarkers of disease; prevention, mitigation and treatment of acute and late effects; and devising optimal strategies for ongoing surveillance after radiation exposure and injury.
Applying evolving basic and clinical information improves practice and therefore will guide both research and response strategies. For example, decades of clinical investigations contributed to our understanding of radiation injury. These investigations include studies of the therapeutic use of radiation for cancer treatment, the natural history and treatment of hematologic disorders, radiation effects at organ and tissue levels, and the evaluation of medical consequences of both intentional and unintentional significant radiation exposures from across the globe (eg, Chernobyl, Mayak, Goiânia, Fukushima, nuclear bomb testing, and World War II nuclear detonations).
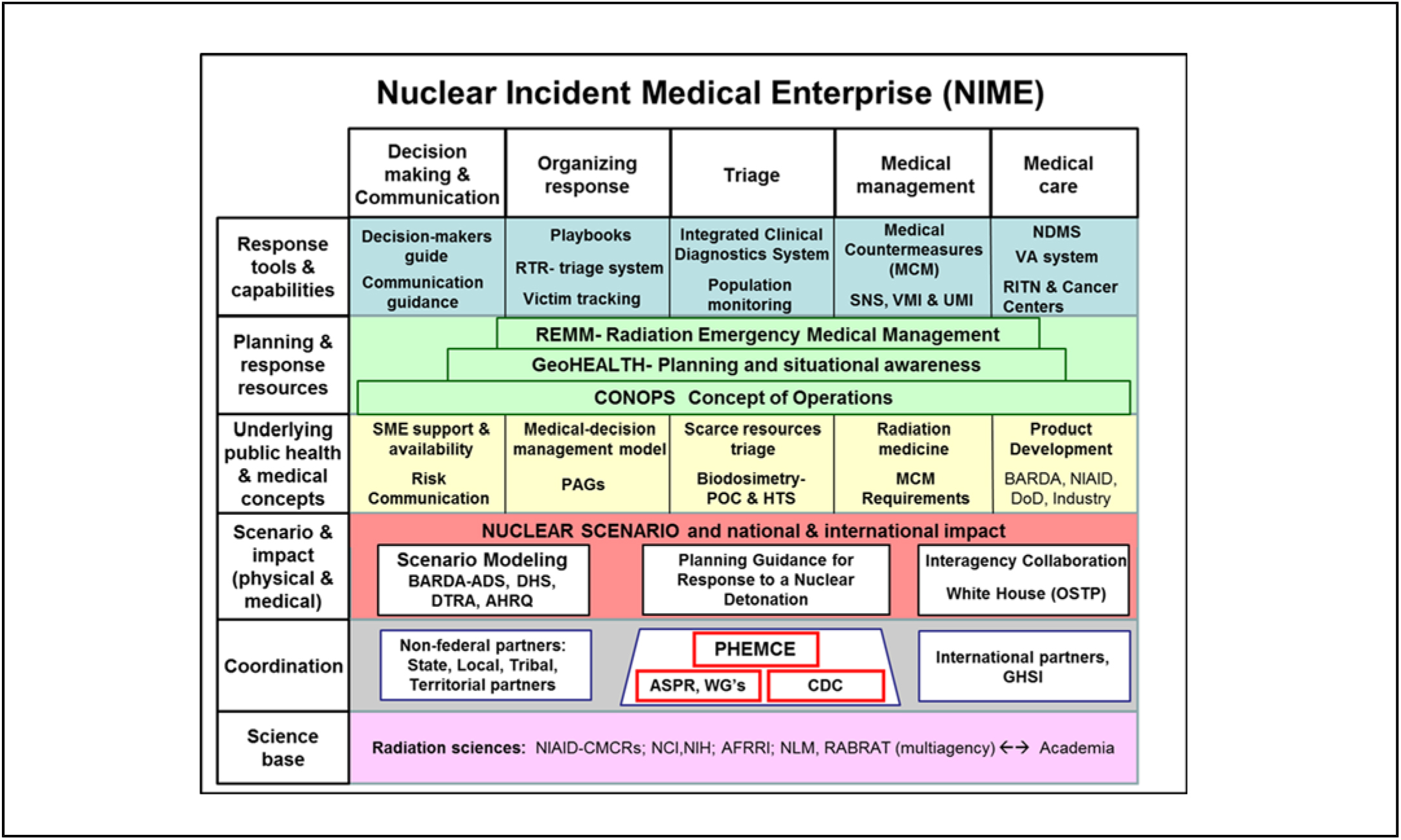
Within the Department of Health and Human Services, under the direction of the Assistant Secretary for Preparedness and Response (ASPR), the Public Health Emergency Medical Countermeasures Enterprise (PHEMCE)8 has a major role in coordinating the development, production, and availability of those MCMs that will be needed following CBRNE scenarios such as a nuclear detonation. Figure 2 depicts PHEMCE agencies, partnerships, and mission components that cooperate both inside and outside the federal government. Clearly the enterprise is vast and complex. (Note: In mid-2018, ASPR realigned; however, the essential functions continue within the new organizational structure.)

FIGURE 2 Public Health Emergency Medical Countermeasures Enterprise Agencies, Partnerships, and Mission Components
The ASPR and PHEMCE build on the accomplishments of their organizational predecessors, including the Office of Public Health Emergency Planning,9 and on legislation for MCM development such as Project BioShield.10 Accomplishments in recent years include, but are not limited to, the following: (1) access to cutting-edge science and technology through workshops convened among federal agencies and with experts from academia and industry; (2) publication of interagency strategic goals and objectives developed for MCM preparedness and plans of action to accomplish these goals;11 (3) development and stockpiling of new products for the Strategic National Stockpile and repurposing previously licensed pharmaceuticals for use as approved MCMs for CBRNE incidents (eg, oncologic products to address the acute radiation syndrome that can occur following radiation exposure). Ongoing work in this area addresses the plans and national capabilities to effectively utilize these MCMs, as well as development of new clinical diagnostics that can most effectively target them to people in need.
The Radiation Nuclear Countermeasures Program of the National Institute of Allergy and Infectious Diseases, which is a component of the PHEMCE, has responsibility for research and development of MCMs, including medical diagnostics, and for other basic biodefense research. Other key members of the PHEMCE are the US Centers for Disease Control and Prevention (CDC), the Food and Drug Administration, and the Departments of Defense, Homeland Security, Veterans Affairs, and Agriculture. Regarding nuclear preparedness issues, the Department of Energy (DOE) is also an important partner. Together these federal agencies and components seek to work together ahead of a CBRNE incident to leverage the basic and clinical sciences to ensure that the right MCMs can be available where and when they are needed.
The concept of CBRNE science supports this work through encouraging PHEMCE leaders to think strategically and across traditional silos to invest wisely in those key scientific opportunities and public health capabilities that are sustainable and most likely to significantly reduce morbidity and mortality from public health emergency threats. Such thinking considers where the most benefit could be achieved within the various planning scenarios and then explores the opportunities present across the full enterprise to respond to that need with the resources available. Within this framework, MCM development programs begin with the end-user in mind, consider the proposed operational picture under which the products would be used, and seek the data needed to support such use. PHEMCE partners develop deployment plans that are exercised and meet scenario-specific timelines. SMEs are recruited to produce evidence-based clinical utilization guidelines and clinical decision support tools to ensure effective use of the products, and support is provided to build medical and public health capacity. MCMs that have dual utility for routine clinical care are sought wherever possible to leverage the clinician’s familiarity, as well as to reduce costs and increase supply chain availability.Reference Coleman, Hrdina and Casagrande12 In these ways, the CBRNE science approach addresses both the complexity and the need for a depth and breadth of knowledge in pursuing an effective MCM enterprise.
Core Element 2
Core element 2 is detailed modeling of CBRNE threats with a systems approach before, during (where feasible), and after specific incidents and exercises.
Planning for optimized public health and medical responses to CBRNE incidents like a nuclear detonation is extremely complex. To better understand and manage this complexity, senior leaders have commissioned formal, iterative computer models that analyze single or multiple aspects of each incident type. The following parameters are among those varied in computer-modeled nuclear detonations: detonation size (kilotons), precise US location, topography, population characteristics (eg, size, density), time of day, weather, height of blast, proximity to critical infrastructure, and type of nuclear device. Outcome variables include various injury types, which can be considered in association with age, gender, subgroups with special needs, and specific preexisting health conditions. Single or multiple effects can be studied by modeling including one or more of the following injury types: radiation exposure; radiation external and internal contamination; superficial and deep thermal (flash or flame) and radiation burns; and various other types of trauma.
Sophisticated computer models can project numbers, locations, types, and severity of specific injuries over time so that plans for response activities and use of MCMs can be optimized both in advance and in real time. Modeling can also help project why, where, and how to best modify routine triage priorities in initial austere conditions and how to optimize staff functions and prioritize scarce resources using ethical and effective protocols as detailed in the Appendix.Reference Casagrande, Wills and Kramer13–Reference Caro, DeRenzo and Coleman15
Modeling can also help identify long-term issues needing consideration. For a nuclear detonation, these issues include, but are not limited to, (1) chronic radiation injury, particularly at higher doses; (2) radiation-induced cancer at lower doses; (3) the scope of medical follow-up needed after radiation injury and/or physical injury; and (4) psychological effects that can be anticipated both near to and far from the detonation zone.
Another component of modeling and systems management is geographic information systems mapping, which presents layers of key information on maps. As a nuclear detonation incident or an exercise unfolds, visualization and tracking are crucial for assessing infrastructure damage; weather; casualty numbers and locations; radiation fallout locations and dose rates; and locations of response assets, including victims and responders in community reception centers, transportation hubs, assembly centers, and major medical centers. These data can be mapped iteratively to assist senior decision-makers over time. Within the Department of Health and Human Services, this is done by the program GeoHEALTH.16 Located in the ASPR Office of Incident Command and Control and housed within the Secretary’s Emergency Operations Center, the GeoHEALTH program maps information in layers that can be turned on and off. These maps are projected on large wall screens visible to the responders and decision-makers present in the Secretary’s Emergency Operations Center to enhance integration of complex information and data sharing.
Core Element 3
Core element 3 is the creation and use of all-hazards plans to serve as a foundation that incorporates detailed planning modifications required for specific CBRNE threats.
The all-hazards response plan is the backbone of US federal responses to large mass-casualty incidents, including CBRNE incidents. All-hazards plans detail anticipated step-by-step actions, including mission assignments, communications, and supporting information needed to help guide decision-making. An incident involving a nuclear detonation uses the all-hazards backbone, but must also include additions and modifications required by a high-radiation zone, management of widespread physical and human radioactive contamination, and massive instantaneous infrastructure destruction. Of note, the CMOSSE’s expertise is especially important when prompt decisions must be made with limited information while recognizing that quick adaptation must be made to the response as new information develops. In addition, senior managers are likely to be unfamiliar with the nomenclature required to describe radiation incidents and the particular issues expected for victims, responders, and the environment.
Threat-specific plans (ie, playbooks) for CBRNE and non-CBRNE incidents have been used for many years. These are internal documents specific to each US government agency and department with a chronological approach to incidents including preparedness, response, and recovery activities. Most were developed to plan for highly detailed and specific hypothetical scenarios of national concern (ie, the National Planning Scenarios).1 Planning for these hypothetical scenarios enables the response to be more easily customized for real-world incidents. As noted in the National Response Framework, for each type of incident one agency or department leads and others follow during a response.5
Medical and public health response planning for a nuclear detonation involves the entire US government, as well as regional, state, local, territorial, and tribal governments; the private sector; professional societies; and international partners. At the federal level, formal plans and activities are reflected in many documents; several key documents are noted in Table 1. Additional guidance is also available from nongovernmental agencies such as the National Council on Radiation Protection and Measurement.25
TABLE 1 Key Nuclear Incident Planning Documents

Extraordinary activities are ongoing to establish and update requirements for developing and utilizing radiation incident–specific MCMs. These include routine medical supplies, specific agents for radiation injury and burns, radiation dose diagnostics, and the capability for timely delivery of supplies when and where they will be needed. Highly technical work is needed for many functions, including the following: (1) setting requirements; (2) developing the concept of operations; (3) determining the cost-benefit of various agents; (4) determining plans for effective and timely deployment; (5) utilizing, when possible, drugs/agents that are already in medical use for other purposes; (6) analyzing existing national supplies; (7) deciding how best to supplement national supplies with additional material in the Strategic National Stockpile or by other mechanisms;26 and (8) developing and incorporating new products, including diagnostics, that might dramatically alter the existing concept of operations. Special SME knowledge and fastidious attention to detail are necessary for addressing such issues as the cold chain for drugs, time window for radiation injury diagnostics (biodosimetry),Reference Sproull and Camphausen27, Reference Sullivan, Prasanna and Grace28 use of diagnostics for internal contamination (bioassay), and the willingness of the private sector to participate.
For all hazards, but especially for huge mass-casualty incidents such as a nuclear detonation, medical and public health response plans are needed for state, regional, city, local, territorial, and tribal locations around the United States, and these activities require federal support and coordination among partners at various levels of government. As such, hazard-specific playbooks are important as elements of these response plans. The Federal Emergency Management Agency has the Radiological Emergency Preparedness Program, with expertise in planning, training, and response to incidents related to nuclear power plants.29 Currently in most, but not all, venues, many nonfederal plans for a nuclear detonation or large radiological dispersal incident were formulated with limited granularity, particularly at the local level where expertise about CBRNE incidents is limited, especially those that involve radiation.30 The limited expertise is understandable given the breadth of day-to-day responsibilities these jurisdictions must address with extremely limited planning resources. Therefore, an important role for federal CBRNE scientists is to engage with nonfederal partners to expedite development of robust and realistic local plans.
One key part of radiation incident medical response planning is training, both classroom and experiential, including participation in exercises in the field, to enable effective implementation of plans. The training needed for responding to a nuclear detonation is far beyond that usually included in disaster medicine courses or health care facility preparedness activities, even for emergency responders and disaster medicine experts. Blumenthal et al.Reference Blumenthal, Bader and Christensen31 identified a major national gap in nuclear and radiological incident training, and recommendations have helped narrow the gap. Various US military and civilian government entities provide high-quality radiation response training.Reference Blumenthal, Bader and Christensen31–Reference Case36 Formal training options include (1) DOE’s Radiation Emergency Assessment Center/Training Site;37 (2) DOE’s Counterterrorism Operations Support;38 (3) Armed Forces Radiobiology Research Institute of the Uniformed Services University training courses;39 (4) CDC and Radiation Emergency Training, Education, and Tools;40 and (5) the Radiation Injury Treatment Network.41 However, despite the availability of these training options, vast national shortfalls in capacity, resources to pay for training, and clinical uptake remain.
Effective planning activities include preparedness exercises7 with tabletop as well as full-scale national, state, and local drills and exercises that include meaningful medical elements. In support of this, federal partners from across the interagency regularly take part in exercises together. Appropriate planning requires that responders address incidents with which they are unfamiliar, including huge radiation mass-casualty incidents. For a nuclear detonation, the following activities may be among those particularly useful to include: (1) use of radiation detection and personal protective equipment; (2) establishing temporary facilities and preparing existing facilities to manage patients and displaced citizens from the radiation environment;Reference Hrdina, Coleman and Bogucki42 (3) clinical familiarity with the use and limitations of diagnostics that will be used to monitor radiation exposure and/or radiation contamination (ie, biodosimetry and bioassay); (4) ability to diagnose and treat acute radiation syndrome; (5) ability to diagnose and treat external and internal radiation contamination; (6) use of radiation triage systems in scarce- and nonscarce-resource settings; and (7) planning for long-term population monitoring after radiation injury and/or for psychological impacts of mass-casualty incidents. As most public health and medical response personnel have never encountered these types of problems, participating in exercises will help to provide additional knowledge and skills and make clear whether and when more training is needed.
Federal support is critical for advancing preparations for responding to a nuclear detonation. For example, the ASPR Hospital Preparedness ProgramReference Hanfling34, 43 and the Radiation Injury Treatment Network are two federally funded cooperative agreements that support large-scale disaster planning, response, and recovery. The Hospital Preparedness Program emphasizes regional coordination of healthcare entities in a health care coalition—particularly hospitals and emergency medical services, but also outpatient services. Integrated community response is critical to ensure appropriate information sharing, patient movement, resource distribution, and coordination of care.
While radiation issues are a small part of the Hospital Preparedness Program, they are the primary focus of the Radiation Injury Treatment Network, which represents this country’s largest cadre of physicians and hospitals with expertise in clinical cancer treatment. Additionally, the CDC’s Public Health Emergency Preparedness cooperative agreements44 support local and state public health partners in building, strengthening, and exercising their abilities to effectively respond to a range of public health threats, including infectious diseases, natural disasters, and CBRNE incidents. The CDC provides guidance and technical assistance to assist state, territorial, and local health departments with their strategic planning to strengthen their all-hazards public health preparedness capabilities. As part of the Public Health Emergency Preparedness Program, CDC’s Cities Readiness Initiative45 is designed to enhance preparedness with life-saving medications and medical supplies in the nation’s largest population centers, where nearly 60% of the population resides, to effectively respond to large-scale public health emergencies including nuclear detonations. State and large metropolitan public health departments use Cities Readiness Initiative funding to develop, test, and maintain plans to quickly receive MCMs from the Strategic National Stockpile and distribute them to local communities. CDC, in conjunction with state public health personnel, also conducts operational readiness reviews to better determine a Cities Readiness Initiative jurisdiction’s ability to implement its MCM plans. Finally, CDC provides extensive training, technical assistance opportunities, and guidance to nonfederal partners on how to receive and make effective use of products from the Strategic National Stockpile.
Underlying all aspects of medical response planning are certain common values expected of decision-makers and health care personnel, such as behaving in an ethical manner and with fairness, honesty, and transparency. During a CBRNE incident, these values will play a critical and prominent role, particularly regarding triage—perhaps more than for almost any other type of CBRNE incident, because of large-scale and initial response environments with austere conditions and limited resources.Reference Casagrande, Wills and Kramer13, Reference Coleman, Knebel and Hick46, Reference Knebel, Coleman and Cliffer47
Communication is essential in the time continuum of an incident, including informing the public of ongoing activities from preparedness to response to advances in knowledge. Radiation incident–specific communications were developed in advance for all levels of federal, state, and local government and for the public sector, with specific details modifiable for the incident as it unfolds.20, 48–52 Ideally, some degree of community preparedness will be active, but as evidenced from historical radiological incidents, the public will (to a degree) fear radiation. Some fears will develop because radiation cannot be detected without a dosimeter and others from the history of nuclear detonations and incidents worldwide. The public’s fears may differ in important ways from the existing incident and not necessarily be justified by scientific data.Reference Sacks, Meyerson and Siegel53 Nonetheless, planners must expect a high level of anxiety and fear. Experts in risk communication as well as SMEs will be particularly important. In that the primary concern after any incident is health and medical effects, clinicians with experience in medical management are critical to assist in communications. Accuracy, honesty, and simplicity will be helpful to successfully communicating with the public. These characteristics will help protect the greatest number of people, maximize trust, and minimize fear and panic.
International radiation response agreements among the United States and other countries, in international collaborations like the Global Health Security Initiative,54 and in agencies such as the International Atomic Energy Agency55 and the World Health Organization,56 are a result of considerable federal activity over the years. These agreements, collaborations, and organizations address procedures to gather and share environmental radiation information, perform radiation dosimetry and/or bioassay, share clinical expertise, and, potentially, provide detection devices, medical equipment, and MCMs across borders.
Core Element 4
Core element 4 is the training and deployment of sophisticated response and incident management personnel cognizant of specific CBRNE issues and the need to embed a CMOSSE near senior incident commanders and senior decision-makers early in and throughout response to an incident.
The first 3 core elements of the CBRNE science enterprise include scientific investigations, the formation of new knowledge, and development of plans for employing this knowledge. However, these are predominantly strategic issues, whereas response activities and incident management are predominantly tactical. Senior response leaders and decision-makers must be cognizant of the scientific basis of what they do in order to optimize the outcome for both responders and the general public.
For example, after a nuclear detonation, even if effective radiation dose-estimation devices and other MCMs are developed, purchased, cached, and prepositioned nationally, they will be ineffective if the tactical implementation (ie, logistics) is not science-based. Certain MCMs need to be available in a very short time frame to be effective. Some need refrigeration. This is true for both radiation and chemical incidents. Strategic implementation of MCM distribution and dispensing is a key element in the nuclear detonation response concept of operations.
After a nuclear detonation, local resources will initially be very scarce in relationship to the need. Consultation with CMOSSEs and other radiation SMEs will be critical to help senior decision-makers most effectively, in real time, optimize and prioritize whatever and whoever is available, at least until reinforcements arrive or victims are transported elsewhere. Rapport and mutual confidence and respect among all senior personnel, built over time, are crucial.
Figure 3 illustrates how the CMOSSE might be positioned within the Incident Command System to maximize scientific input into strategic and tactical decisions. The CMOSSE calls on her/his experience from participating in operations and familiarity with the broad range of SMEs to directly participate and involve additional SMEs as needed. Prior training for senior incident managers and decision-makers at all levels about responding in a highly radioactive environment would also be helpful. A Decision Makers Guide: Medical Planning and Response for a Nuclear Detonation provides both essential and detailed information regarding the underlying concepts of the health and medical issues so that just-in-time information and background information are available for decision-makers who are likely to be unfamiliar with the basic physics and biology concepts involved.24

FIGURE 3 Proposed Inclusion of the CBRNE Medical Operations Science Support Expert (CMOSSE)a in the Incident Command System Organizational Structure
Implementation of the National Incident Management System59 and the Hospital Incident Command System60 will need to be adapted after a nuclear detonation. The radiation environment requires that health care professionals, hospital administrators, managers of emergency venues, and responders understand how to protect themselves and their patients and provide timely, effective care in a radiation environment. Medical encounters may need to be modified in various ways for both first responders and first receivers. A concept under development by the Council on Radiation Protection and Measurement and DOE that can provide additional expertise is the Radiological Operations Support Specialist,Reference Alai, Askin and Buddemeier2, Reference Irwin61 which is a health physics–based special expert cadre.
How federal programs assist state and local preparedness entities through the deployment of SMEs or other experts or the provision of technical assistance is detailed in the Appendix, which includes descriptions of the National Disaster Medical System; surge and healthcare coalitions (eg, the Hospital Preparedness Program); Radiation Injury Treatment Network, supported in part by the US Navy; CDC’s Public Health Emergency Preparedness program; and nongovernmental professional groups (eg, the Council on Radiation Protection and Measurement). A further example is the Federal Radiological Monitoring and Assessment Center, an interagency organization that serves as a federal asset available on request of DOE, Department of Homeland Security, Department of Defense, Environmental Protection Agency, National Aeronautics and Space Administration, Nuclear Regulatory Commission, and state and local agencies to respond to a nuclear or radiological incident.62 Additionally, the Interagency Modeling and Atmospheric Assessment Center coordinates and disseminates federal atmospheric dispersion models and hazard prediction products that can be used alone and as part of GeoHEALTH.16, 63
State and local planners and responders have many types of routine incidents for which to prepare, with little extra time or money for rarely occurring CBRNE incidents such as nuclear detonations. In addition, highly experienced senior local radiation expertise is uncommon. To assist, ASPR and the National Library of Medicine have developed key “just-in-time” tools for use by planners and responders: Radiation Emergency Medical Management,64 and Chemical Hazards Emergency Medical Management.65 ASPR has also established the Technical Resources, Assistance Center, and Information Exchange.66 Additionally, the CDC has published a variety of tools and information for both medical professionals and the public on CBRNE incidents.67
To assist senior decision-makers and incident commanders without experience in CBRNE subject matter, ASPR developed A Decision Makers Guide: Medical Planning and Response for a Nuclear Detonation.24 It is designed for use by incident commanders and decision-makers, who are likely to be elected officials at all levels of government with limited experience and knowledge of the underlying science and complexity of a nuclear detonation. The Decision Makers Guide’s purpose is to bring these decision-makers up to speed quickly on what is involved in a response to nuclear detonation. Additional detailed guides are available from the National Council on Radiation Protection and Measurement.68
In recognition that all responses to mass casualty incidents begin locally with state and federal assets providing support if and when needed, HanflingReference Hanfling, Burkle and Dallas69 and HickReference Hick, Bader and Coleman14 point out the need for federal response immediately following a large disaster like a nuclear detonation (see Appendix for additional details).Reference Carter, May and Perry70–Reference Hauer72 The cadre of national CMOSSEs will come from public and private sectors, and close collaboration on all aspects of CBRNE science will be required.
CBRNE mass-casualty incidents cross international boundaries and borders. The Fukushima nuclear power plant disaster in Japan provided an example of excellent collaboration between US government agencies and international partners. Collaboration was initiated early and continued long after the acute response phase ended. Experts were consulted from many governments, academic centers, professional societies, the locally affected community, and international agencies (eg, the International Atomic Energy Agency). Even more intensive collaboration would be required for the medical response to a nuclear detonation, which is a much larger and more complex incident.
A few of the key US government agencies involved in developing recommendations for the provision of medical care after Fukushima included the DOE’s Radiation Emergency Assessment Center/Training Site37 and the Advisory Team for Environment, Food, and Health.3 A summary of potential on-scene and remote response assets is detailed in the Appendix, including those from the Department of Defense, which also has radiation response teams.
Core Element 5
Core element 5 is the development of recovery and resilience plans accounting for specific CBRNE effects as well as psychosocial impacts on communities.
Planning beforehand for community resilience after a radiation incident will enhance both the short- and long-term outcomes.73 Recovery and resilience are also built into response activities. Stakeholder preparations involve medical and psychological preparation; health care and other personal support systems (eg, food, housing, transportation, utilities, communication systems); and economic analysis to guide initial investment in planning, as well as in restoring the economy. Indeed, operationalizing recovery and resilience occurs as soon as the response begins, ramping up in intensity over time.
The disruption from a CBRNE incident can reach far beyond the epicenter. A nuclear detonation or a large release of radioactive material will disrupt the nation and the entire world, as evidenced by Fukushima and Chernobyl. But disruption due to the surge of evacuees, many of whom may be displaced indefinitely, must be addressed during the response phase to help them adapt to an extraordinarily traumatic experience.
Routine public health issues addressed by the public health system (eg, vaccines and routine community health services) have an impact on daily life, but are particularly important during or after disasters. Access to public health and health care system assets and capabilities are critical to the lives of many citizens, particularly the elderly and those with chronic illnesses. Even a minor disruption, such as one due to extreme weather, can impair health and cause a great deal of stress on people and their caregivers.Reference Fujitani, Carroll and Yanagisawa74 Returning to “normal” is critical. Thus, planning how to get to normal, or the “new normal,” implementing these plans during the response and then ramping up as the response phase moves into the recovery phase is an essential component of community and individual resilience.
For a nuclear detonation or a large release of radiation from another cause, short-term screening of potentially exposed people may be necessary, as well as long-term epidemiological studies. Experiences from Fukushima and Chernobyl demonstrated the importance of such studies. Long-term adverse effects on the community must be projected and planned for in effective public health and medical preparedness and planning.Reference Murakami, Takebayashi and Takeda75 Involving the community in this process will facilitate understanding of the issues and trust in the government. Thus, the public health and health care systems must anticipate disruptions and also the surge that will follow a large-scale incident. The CMOSSE’s familiarity with general medicine and health care systems is particularly useful when anticipating, planning for, and responding to periods of scarce resources and austere conditions in the immediate response and recovery phases.51, 76–88
Recovery after a radiation disaster is complicated. The “new normal” is invariably more difficult for many, and the entire country will be affected. The process of restoring psychological and economic health is complex, and political and security issues are likely to have a substantial impact on society. Definitions of “safe” and “clean enough to allow humans to re-enter and live and work there” will need to be adjudicated. With the underlying radiophobia often present in society, the ability of the CMOSSE and radiation SMEs to provide objectivity and to present information in comprehensible terms with compassionate understanding of suffering and fear is critical. Guidance documents related to “how safe is safe” will help during the response and short-term recovery and can inform the public discussion during long-term recovery.18, 73, 89
Core Element 6
Core element 6 is the commitment to realistic and honest assessments of lessons learned both from previous incidents and from exercises.
Regardless of the type of response or whether it was an exercise or training session, candid post-hoc observations can generate lessons learned and lead to corrected actions and potential improvements for the future (see also core element 7). Typically, immediate review includes an all-hands “hot wash,” which is an open and honest discussion and assessment of the performance of each response group and of the overall system. The hot wash is intentionally not fault-finding. After the hot wash, the after-action review, a formal, structured evaluation, is prepared for leadership. The after-action review includes a description of what happened, an analysis of why it happened, and an assessment of how the action might be done better next time by the participants and those responsible for the plans and the response.
Within the lessons-learned process, the implementation of corrective actions is the mechanism by which exercises and responses to real-world incidents can inform and improve other preparedness cycle components. Corrective actions are the concrete, actionable steps outlined in improvement plans that are intended to resolve preparedness gaps and shortcomings experienced in exercises or real-world incidents. The Corrective Action Program enables users to prioritize, track, and analyze improvement plans. By including the CMOSSE as part of the decision-makers group before and, especially, during an incident, the intent, execution, and outcome of various decisions can be better understood.
Providing knowledge “on-the-fly” requires quick and timely access to peer-reviewed scientific literature and other information. Librarians are experts in library and information science with knowledge and skills to find, review, and organize relevant material and information for CMOSSE use. At ASPR, library and information science experts from the National Library of Medicine and the NIH Library work with ASPR staff and staff from ASPR’s Technical Resources, Assistance Center, and Information Exchange66 to provide timely access to key vetted information resources and analysis. Ideally, these information experts should participate in the lessons learned and corrective action programs, as they may reach further and deeper into literature that is unfamiliar to SMEs and suggest linkages not previously identified. Indeed, the critical role of library and information science is exemplified by the importance of this expertise in the creation of CBRNE science (coauthor AAL) and in the wide range publications that disseminate new knowledge and approaches.24, Reference Coleman, Adams and Adrianopoli49
Lessons learned is the start of the next cycle of ideas and improvements based on turning theory into reality. A unique opportunity for radiation/nuclear response occurred in 2011 for a group of SMEs from multiple US government agencies who advised the American ambassador in Japan on the conduct of the US on-scene response to the Fukushima disaster. The effective response was due, in large part, to leadership that encouraged open discussion, disagreement/debate, and further problem-solving as a team. This experience led to the development of the “medical decision model” for how to work on a nuclear/radiological incident.Reference Coleman, Blumenthal and Casto90, Reference Koerner, Coleman and Murrain-Hill91 This model emphasized the importance of being able to make major decisions with partial information and to adapt, without being “wrong” or “defensive,” as new information emerged. This is a skill common to emergency physicians and oncologists who frequently must make choices as the diagnosis unfolds with the information that they have available at the time. Emergency managers have similar challenges. The medical decision model also strongly encourages SMEs, particularly the CMOSSE defined in this paper, to work directly with the decision-maker, as information is exchanged differently in-person as compared to teleconference, webinars, or in writing.
Lessons learned requires that new information is discussed and then formulated in ways that are useable for core element 7 as well as in the entire CBRNE science spectrum (Figure 1). Thus, lessons learned may lead to major new approaches as those who served as “boots on the ground” during the response can provide valuable input into all 7 elements. This input may bring forth ideas that can have substantial impacts on research, development, and implementation plans. Lessons learned in a nuclear incident will include all 7 core elements of CBRNE incident management, and the CMOSSE is critical at each major stage.
Core Element 7
Core element 7 is the commitment to continuous improvement, based on new knowledge from the intelligence community and scientific and clinical medicine communities and on experience gained from exercises and actual incidents.
For core element 7, we aim to incorporate strategic and technical advances identified, analyzed, and recommended in association with experiences in the other 6 core elements, especially lessons learned. Progress results when new ideas are welcomed by academicians, policy makers, program leaders, industry, and funders, which thus encourages the application of leading-edge science to the critical needs of the nation. To make progress and incorporate new knowledge into improved planning, response, and ultimate outcomes requires SMEs in specific areas and CMOSSEs who can integrate the subject matter into the complex system of CBRNE incidents.
An example of the depth of knowledge and tools required for CBRNE science is the US government’s Nuclear Incident Medical Enterprise,Reference Coleman, Sullivan and Bader92 which conceptually applies to all CBRNE threats (Figure 4).
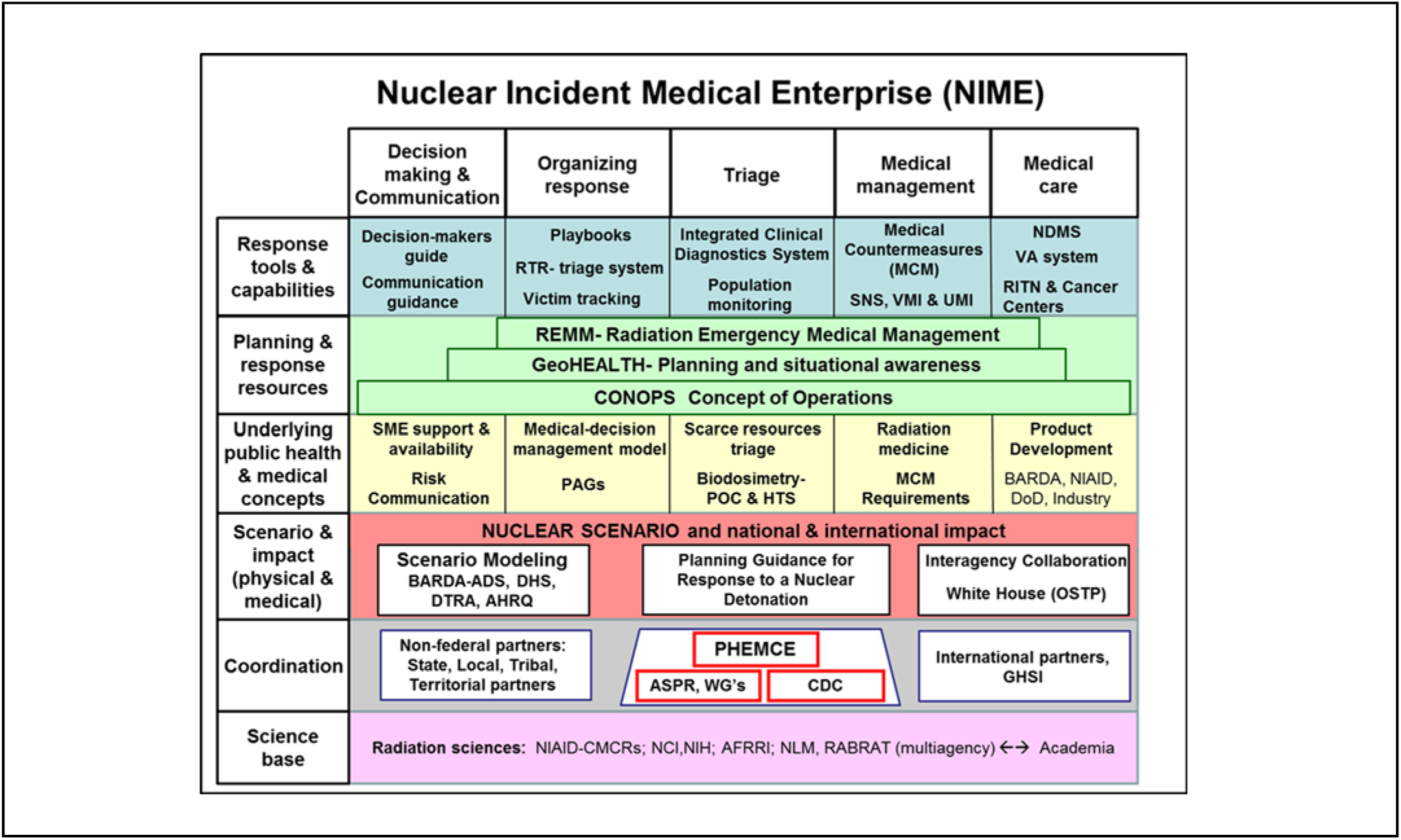
FIGURE 4 Nuclear Incident Medical EnterpriseReference Coleman, Sullivan and Bader92
Within the Nuclear Incident Medical Enterprise, the horizontal boxes represent the time-phases of the medical response to a nuclear incident. The top row, “Response tools and capabilities,” is what the public would see put into action during the response to a nuclear incident. How these response tools and capabilities originated is based on the items noted vertically in each column. Nuclear Incident Medical Enterprise is science-based (bottom row), with coordination among all the players and participants done by the PHEMCE. Scenarios are used for planning purposes.
For the various steps in the response (columns), specific resources and capabilities will be used and are made available. These capabilities and assets would be used in combination with the underlying science base and planning scenarios during the various steps of the response. Making all of this work in a coordinated way during an incident requires a concept of operations with a focus on actionable information, a means of running the response based on the rapidly changing situational awareness (eg, GeoHEALTH), and just-in-time public health and medical information for responders (eg, Radiation Emergency Medical Management). These resources and capabilities are under continuous improvement and development. In order to continuously improve, effective collaboration of all these elements in the Nuclear Incident Medical Enterprise is required. While complex, the Nuclear Incident Medical Enterprise is indicative of the systems-based approach necessary for CBRNE science to operate and of how the subject matter expertise goes well beyond just general disaster medicine. Thus, the need for active participation in planning and response by the CMOSSE is apparent and CMOSSE should be an integral part of the emergency management team, ideally on-site when possible during a response.
The following are components of continuous improvement of CBRNE science involving a broad range of expertise:
Knowledge: Research and development are supported within government, including collaborations with and support provided to academia, research institutions, and industry.
Broad constituency, including outside organizations: These include the Council on Radiation Protection and Measurement, the Radiation Injury Treatment Network, the National Association of County & City Health Officials, and others.
US government: The US government promotes science preparedness activities to establish and sustain a scientific research framework that can enable emergency planners, responders, and the whole community to better prepare for, respond to, and recover from major public health emergencies and disasters.93 The federal government develops programs such as the PHEMCE and has high-level coordination through the Office of Science and Technology Policy (eg, Planning Guidance for Response to Nuclear Detonation).18 Additionally, the NIH has initiated activities to further time-critical research in response to disasters, including the NIH Disaster Research Response Program and the Intra-NIH Disaster Interest Group, to help facilitate collaborations across the NIH (see Appendix).Reference Miller, Yeskey and Garantziotis94, 95
Professional societies: The potential for formalizing the CMOSSE qualifications will be discussed with the Society for Disaster Medicine and the Association of State and Territorial Health Officials. The Radiation Research Society and Health Physics Society emphasize and support the science behind nuclear and radiological incidents.
Academia: Academic institutions have established programs that focus on public health, disaster medicine, health security, and related fields. A pioneering program and an example was that of the University of Pittsburg Medical Center, which is now based at Johns Hopkins Bloomberg School of Public Health (Johns Hopkins Center for Health Security).96
Back to the laboratory: As the science of human disease and injury relating to CBRNE threats advances, opportunities arise for new therapeutic and diagnostic products. Additionally, as gaps in capabilities are identified and prioritized for remedy through the preparedness, planning, response, and recovery processes, groups such as ASPR Biomedical Advanced Research and Development Authority stimulate research and development that can help close those gaps. Awareness of the gaps and new advances can also reveal other issues that require basic research, including with the National Institute of Allergy and Infectious Diseases and other NIH programs, to contribute to advances in preparedness, planning, response, and recovery. This closes the loop from lessons learned back to the need for new knowledge.
CBRNE science in development: ASPR continues to hone and improve its internal processes and productivity through organizational restructuring, acquisition and use of new resources, and adapting its focus to new threats and issues as they arise. In regard to the CMOSSE, a recent restructuring has created the ASPR CBRNE Expert Science Group, which is the CMOSSE put into practice.
NEXT STEPS FOR CBRNE SCIENCE
CMOSSE
The need for the types and levels of expertise encompassed by the CMOSSE is apparent. CBRNE science practitioners work in government, academia, industry, and the private sector. CBRNE science expertise involves knowledge far broader and deeper than that required of physicians certified in disaster medicine. Not all CMOSSE practitioners are physicians or certified by the American Board of Emergency Medicine, nor do we propose that this be a formal medical board. We recommend the formation of a group to consider a formal compilation of CMOSSE competencies and designation by a multidisciplinary, public and private sector team (see Appendix for more details).
Accepting and Embracing Change
The evolving challenges of CBRNE threats, the development of new MCMs (including diagnostics), emergence of new science, and changes in the practice of clinical medicine require SMEs and CMOSSE to continuously look for new opportunities for improvement. For success, these key points must be recognized and accepted:
Science advances and clinical care changes.
Improvements in capabilities and solutions beget changes in policy.
Plans should not be static.
Changes must be communicated in a timely fashion.
Buy-in at all levels is key and sustainable support is essential.
CONCLUSION
This paper and the accompanying Appendix present the complexity of planning for and responding to the public health and medical issues arising from one of the most difficult types of CBRNE incidents potentially facing the United States and the world—a nuclear detonation. In recent years, effective preparedness and response activities were sponsored and advanced by both government and the private sector. New collaborations and partnerships were forged. While more is always needed, a recognition of the progress made is warranted. As advancements in planning for a nuclear detonation response are made, other less-complex CBRNE incident scenarios can utilize the CBRNE science enterprise as well.
The many aspects of CBRNE science engage experts of various specialties in service to the country. The complexity of the enterprise is clear, as is the value of a systems-based approach. Recognition of both CBRNE science as a distinct competency and the creation of the CMOSSE designation informs the public of the enormous progress already made and broadcasts an opportunity for new talent to enter the various disciplines of this large, new field. Next steps include committing to develop future systems-based CBRNE response plans. These systems-based plans will require integration of CBRNE science, with the consideration of a formal compilation of competencies for designation of CMOSSE by a multidisciplinary team spanning the public and private sectors.
Acknowledgements
The authors thank RADM Ann R. Knebel, former Director of Preparedness Planning, DHHS/ASPR and Shayne Brannman, DHHS/ASPR for their comments and contributions to this important endeavor. An extensive effort to draft and edit this paper over the year in preparation was done by Joanna Prasher, CDC, and coauthors Bader, Coleman, Cliffer, and Livinski. The following individuals provided extensive suggestions, edits, and discussion, and their inclusion in the acknowledgments and not as coauthors does not minimize their contributions: Joanna Prasher, CDC; Susan Gorman, DHHS/ASPR; Robert Whitcomb, Jr, CDC. The authors thank all who have participated in discussions about this topic over the last few years.
Author Contributions
CN Coleman, JF Koerner, JL Bader, C Hrdina, and R Hatchett contributed equally to the development of this concept and this paper. Other authors are listed in the order in which their sections appear.
Disclaimer
For the following authors, the contents of this manuscript are their personal and professional opinions and not policy of their agencies or institutions: C. N. Coleman, J. F. Koerner, C. Hrdina, K. D. Cliffer, J. L. Hick, M. K. Mansoura, S. V. Nystrom, M. J. Marinissen, L. Wathen, J. M. Appler, R. Casagrande, D. Estes, P. Byrne, E. M. Kennedy, A. A. Jakubowski, D. M. Weinstock, N. Dainiak, D. Hanfling, A. L. Garrett, N. N. Grant, D. Dodgen, T. F. MacKAY, M. Treber, M. J. Homer, G. Korch, R. Hatchett. The content of this article is not opinion or policy of the US government.
Sources of Support
None.
Supplementary material
To view supplementary material for this article, please visit https://doi.org/10.1017/dmp.2018.163.