Atyphoon (hurricane or cyclone, depending on the geographic location) is a storm system categorized by wind speeds ranging from 119 km/h to over 252 km/h on the Saffir-Simpson scale. Between 1980 and 2009, typhoons caused an estimated 412,644 deaths and 290,654 injuries and affected 466 million people.Reference Doocy, Dick and Daniels 1 The impact of typhoons goes beyond immediate deaths and injuries. Public health and critical infrastructure are frequently damaged, leading to long-term health effects on the population. Studies have demonstrated the negative effect that typhoons have on patients with noncommunicable diseases.Reference Ryan, Franklin and Burkle 2
In 2013, Typhoon Haiyan (referred to as Yolanda by the Philippine Atmospheric, Geophysical, and Astronomical Services Administration [PAGASA]) was the strongest typhoon to make landfall ever recorded. Its maximum wind speed was 315 km/h, giving it a classification of a category 5 on the Saffir-Simpson hurricane scale. Typhoon Haiyan made landfall on the Philippines island of Leyte on November 8. Haiyan affected over 16 million people, killed 6300, and displaced 4 million in 57 cities around the Philippines. 3 The effects from the strong wind and rainfall combined with up to 7-meter storm surges were devastating. On Leyte Island, the 2 major cities affected were Ormoc City, which suffered mostly wind and rain damage, and Tacloban, which experienced severe damage from the storm surge and wind.
Ormoc City is the largest city in the Leyte Province with a population of 191,200 and a surrounding service region of 614 km2. 4 The city contains 5 hospitals: a government hospital and 4 private hospitals. In the first 2 weeks after the typhoon, the government hospital was partially functional and 2 private hospitals were partially functional. The national and international response was great and included international medical teams and field hospitals from many nations.Reference Dew 5
Data are lacking on the illness and injury burden after typhoons. This article focused on examining nonfatal illnesses during the post-acute typhoon period. Our study aimed to improve disaster preparedness for typhoons by providing a descriptive analysis of the medical, surgical, pediatrics, and obstetrics admissions for the Ormoc District Hospital (ODH) catchment during the pre-impact, impact, and post-impact phases of the Typhoon Haiyan disaster in the Philippines.
Methods
Setting
ODH is a 100-bed, level II hospital operated by the Leyte Provincial Government. ODH offers medicine, surgery, pediatrics, and obstetrics and gynecology services as well as a general intensive care unit (ICU), neonatal ICU, and high-risk pregnancy unit. It serves Ormoc City, neighboring municipalities, and geographically contiguous areas. In 2013, the bed occupancy rate was 127%, with 9171 admissions, 16,125 emergency visits, and 60,976 outpatient clinic visits. After Typhoon Haiyan, almost all district (barangay) health centers and hospitals in the region were damaged. ODH sustained 80% damage, including all inpatient wards and operating rooms. The hospital was closed for several days with no medical services from November 8 to 9, 2013, and no surgical services from November 8 to 20, 2013.
The Canadian Red Cross Emergency Response Unit (CRC-ERU) established a field hospital on the grounds of ODH to support the medical needs of the community. The CRC-ERU was part of the Red Cross Health Emergency Response Unit. In Ormoc City, the ERU was deployed as a basic health care unit with surgical capacity, focusing on maternal and child health, inpatient, and surgical services in support of the damaged ODH. The field hospital, staffed with both local and international medical providers, opened 13 days after impact and operated from November 21 to December 21, 2013. The field hospital had 70 inpatient beds, mostly in pediatric and postpartum wards. Within 1 month of operation, the field hospital admitted 1226 patients, performed 114 surgeries, and delivered 418 babies, in close collaboration with the ODH, Ministry of Health, and the Philippine Red Cross. The ODH hospital operating and delivery rooms reopened on December 5 and inpatient wards reopened on December 21.
Design
This was a retrospective, descriptive analysis of admissions to ODH in Leyte, Philippines, for October to February 2013. Information was collected from hospital logbooks provided by ODH. The characterization included subanalysis of the medical, surgical, and obstetrics admissions. The patients admitted for medical problems were separated into adult and pediatric cases for individual descriptive statistics. The diagnoses were categorized under respiratory, gastrointestinal, injury, cardiovascular, neurology, urology, gynecology, infectious disease, endocrinology, skin, hematology, renal, psychiatry, and toxicology. For infectious disease, diagnoses of pneumonia and tuberculosis were categorized under respiratory, gastroenteritis was included under gastrointestinal, and urinary tract infections were included under urology. The infectious disease category contained diagnoses of fever, sepsis, typhoid fever, dengue fever, tetanus, and measles. The time periods chosen for comparison were the pre-impact, impact, and post-impact phases, each of which was equal in duration. The impact phase was defined as the time from Typhoon Haiyan landfall on November 8 to NGO field hospital closure on December 21, which was 44 days. The statistical significance of the variance in daily patient admissions was compared by using the two-sample variance-comparison test in STATA 13.1 (StataCorp LP, College Station, TX). The chi-squared test was used for categorical variables. Statistical significance was set at P<0.05. ODH provided de-identified data for analysis.
This study received ethical approval from the Republic of Philippines Eastern Visayas Health Research and Development Consortium Ethics Review Committee and the Johns Hopkins School of Medicine Institutional Review Board.
Results
Characterization of Overall Hospital Admission Volume
A total of 1052 patients were admitted in the pre-impact phase (September 25 to November 7), 1156 patients in the impact phase (November 8 to December 21), and 1392 in the post-impact phase (December 22 to February 3). The logbooks for internal medicine and general pediatric patients were missing the first 6 days of daily admissions from September 25 to September 30. The increase in total patient daily admissions from the pre-impact to the impact phase was statistically significant (P<0.00001), as was the difference from the impact to the post-impact phase (P<0.00001). During the few days after impact on November 8, there was a sharp drop in the number of patients admitted (Figure 1). Once health care facilities reopened, there was a surge in patient volume during the impact phase. The post-impact phase showed a gradual decrease in patient volume closer to the levels of the pre-impact phase (P<0.02).
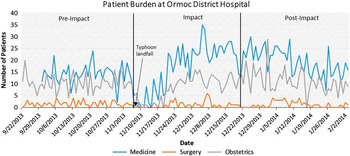
Figure 1 Daily Admissions to the Hospital for Medicine, Surgery, and Obstetrics, Ormoc District Hospital, September 25, 2013, through February 3, 2014. *Includes field hospital admissions during the impact and post-impact phases.
Characterization of Patient Demographics and Diagnoses
Adult Medical Admissions
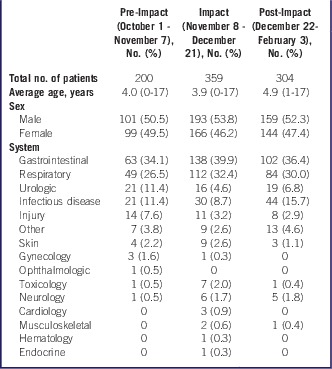
The adult patient hospital admissions increased slightly between the pre-impact and impact phases from 338 to 405 admitted patients (Table 1, P<0.01). The increase was greater during the post-impact phase to 561 (P=0.037). The average number of admissions per day was 8.9 (range, 2-17) during the pre-impact phase, 9.0 (range, 0-19) during the impact phase, and 12.5 (range, 4-21) during the post-impact phase. The most common admission diagnosis varied in each phase, but the incidence of gastrointestinal and respiratory illnesses increased in the impact and post-impact phases.
Table 1 Patient Demographics and Admission Diagnoses for Adult Medical Patients Before, During, and After Typhoon Haiyan, Ormoc District Hospital, 2013

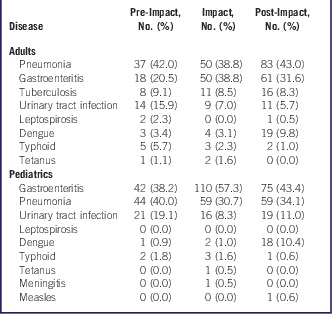
Pneumonia, gastroenteritis, and tuberculosis were the main infectious diseases in all 3 phases (Table 2). There was an increase in the number of gastroenteritis cases from 18 cases during the pre-impact phase to 50 during the impact phase (P<0.00001). There was a slight increase to 61 in the post-impact phase (P=0.80). The incidence of pneumonia increased from 37 cases in the pre-impact phase to 50 during the impact phase (P=0.001) and even higher to 83 during the post-impact phase (P=0.17). Tuberculosis also increased from 8 cases during the pre-impact phase to 11 during the impact phase (P<0.01) and 16 during the post-impact phase (P=0.18). During the post-impact phase, there was an increase in the incidence of dengue fever with 19 diagnoses. There were noticeable increases in the chief complaints related to blood pressure between the impact and post-impact phases (14 to 58, P<0.001). The number of stroke or stroke-like (“right sided weakness”) diagnoses increased from 8 cases during the impact phase to 14 cases during the post-impact phase (P=0.07).
Table 2 Distribution of Infectious Disease Cases for Adults and Pediatrics Before, During, and After Typhoon Haiyan, Ormoc District Hospital, 2013
During the impact phase, the number of skin complaints almost tripled to 17 cases (P=0.0002), which were mostly infected wounds and diabetic ulcers. The incidence decreased to 7 cases during the post-impact phase (P=0.0001).
The injury burden increased slightly from 46 to 58 cases between the pre-impact and impact phases (P=0.18) and decreased to 45 cases during the post-impact phase (P=0.02). During the pre-impact phase, the most common injuries were lacerations or stab wounds but this shifted to motor vehicle collision-related injuries during the impact and post-impact phases (Table 3). From the pre-impact phase to the impact phase to the post-impact phase, there were sharp increases in the number of motor vehicle collision-related injuries from 4 to 23 to 25, respectively. The increase between the pre-impact and impact phases was statistically significant (P<0.00001), whereas the increase between the impact and post-impact phases did not meet the significance criteria (P=0.055). Many injuries due to motor vehicle collisions were listed as “vehicular accidents”; thus, the specific injury and whether the injury required surgical intervention was unknown.
Table 3 Distribution of Injury-Related Diagnoses for Adult Medical Patients Before, During, and After Typhoon Haiyan, Ormoc District Hospital, 2013

Pediatric Medical Admissions
The total number of pediatric admissions increased from 200 during the pre-impact phase to 356 during the impact phase (P<0.00001). During the post-impact phase, the number of admissions decreased slightly to 301 (P<0.01). The average number of admissions per day was 5.3 (range, 0-12) during the pre-impact phase, 8.1 (range, 0–22) during the impact phase, and 6.7 (range, 2-16) during the post-impact phase (Table 4).
Table 4 Patient Demographics and Admission Diagnoses for Pediatric Medical Patients Before, During, and After Typhoon Haiyan, Ormoc District Hospital, 2013
The top reasons for admission at baseline were gastrointestinal, respiratory, urologic, and infectious diseases (Table 2). The incidence of gastroenteritis increased from 42 to 111 cases between the first 2 phases (P=0.0025) and decreased to 73 cases in the post-impact phase (P=0.038). Pneumonia was the primary respiratory diagnosis and increased from 44 to 60 cases between the pre-impact and impact phases (P=0.013) and remained elevated at 58 cases during the post-impact phase. There was a large increase in dengue fever from 2 to 17 cases between the impact and post-impact phases, respectively (P<0.00001).
The skin illnesses were noted primarily as abscesses, burns, and a few diabetic skin complications. The incidence more than doubled to 9 cases during the impact phase (P<0.01) and declined to 3 cases during the post-impact phase (P<0.00001).
There was a concerning increase in toxicology cases during the impact phase. During the pre-impact phase, there was one presentation for a snake bite. During the impact phase, there was a statistically significant increase in the number of cases of 7 (P=0.00001). All were kerosene ingestions in children between the ages of 1 and 6 years. During the post-impact phase, there was only 1 case, which was a kerosene ingestion incident in a 3-year-old.
Surgical Procedures
The typhoon severely damaged the operating rooms at ODH, preventing surgical procedures for 13 days. When the NGO field hospital was established on November 21, surgery resumed. The average number of surgical cases per day decreased during the impact phase (1.5 to 0.9), which accounted for the lack of surgical capacity until the field hospital opened. During the impact phase, the average daily number of surgical cases was 0.9. The variance in surgical cases per day between all 3 phases was not statistically significant.
The distribution of patient age and sex did not vary greatly between phases (Table 5). Corresponding to the overall decreased surgical burden was a statistically significantly increased proportion of emergency procedures during the impact phase (P=0.01). A significantly increased proportion of surgeries (86.8%) used spinal anesthesia during the post-impact period (P<0.00001). Spinal anesthesia was used for abdominal and lower extremity surgeries in all phases, and the reason for this shift is unknown.
Table 5 Patient Demographics and Procedures for Surgical Patients Before, During, and After Typhoon Haiyan, Ormoc District Hospital, 2013
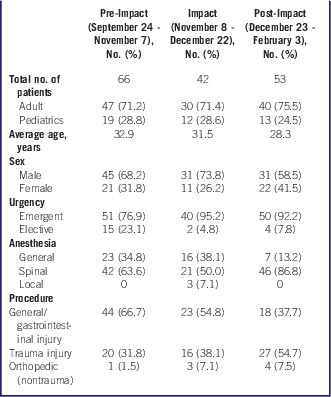
The number of trauma cases decreased from 19 to 14 between the pre-impact and impact phases (P<0.01) and increased to 23 in the post-impact phase (P=0.41). The general/gastrointestinal surgical case load decreased from 44 to 23 between the pre-impact and impact periods (P=0.51) and even further to 18 during the post-impact phase (P=0.04). The majority of general/gastrointestinal surgeries were due to appendicitis. Other cases included bowel obstructions and incarcerated hernia repairs. Nontraumatic orthopedic cases were leg amputations secondary to diabetic foot wounds.
Deliveries and Obstetrics
The average number of deliveries per day decreased transiently during the impact phase from 10.4 deliveries per day to 8.3 deliveries per day (Table 6). This decrease was statistically significant (P=0.025). The rate increased from 8.3 to 11.1 between the impact and post-impact phases (P=0.99).
Table 6 Obstetric Delivery and Newborn Characterization Before, During, and After Typhoon Haiyan, Ormoc District Hospital, 2013

Average gestation time ranged from 38.8 to 39.3 weeks in all phases. Noticeably, during the impact phase, the cesarean delivery rate decreased from 20.9% to 12.6% (P=0.002). The post-impact phase cesarean delivery rate (14.8%) remained less than the pre-impact rate.
Discussion
With the increasing frequency of natural disasters, it is critical to understand the immediate and medium-term health needs of the affected population for planning medical and surgical services during a response.Reference Yamada and Galat 6 The controversies over deployment of foreign medical teams to acute-onset disasters has increased since the earthquake in Haiti, which led to a recent World Health Organization proposal to pre-credential teams. 7 In order to more successfully target these responses, it is important to understand the epidemiology of inpatient and outpatient care after these events. Prior studies have focused mostly on outpatient or mobile clinic visits.
The overall daily patient admissions significantly increased from baseline during the impact phase, despite the hospital being closed for the first few days after Typhoon Haiyan made landfall. The vast majority of the increase was not a direct result of the cyclone, but was related to the resultant damage to infrastructure, especially water and sanitation systems, as well as the reduced access to health care. Our study identified 3 important trends for post-typhoon health care planning: increased infectious diseases, an increase in exacerbated chronic conditions, and the importance of pediatric and obstetric care.
There was a significant increase in infectious disease admissions after the event. Gastroenteritis and pneumonia were the main medical causes of admission prior to the typhoon for adults and children. Afterwards, there was a statistically significant increase in their incidence. A rise in respiratory infection following hurricanes has been documented given the increase in air pollutants, exposure to mold, and damp environments.Reference Chung, Stock and Smith 8 - Reference Barbeau, Grimsley and White 10
Evidence of disruption of the normal health and public health infrastructure can be found in several disease trends. An investigation of an outbreak of gastroenteritis 3 weeks after Typhoon Haiyan in Kananga, Leyte, determined the cause was likely contaminated water from the municipal water system.Reference Ventura, Muhi and de Los Reyes 11 With the increased volume of water from the rains, chlorine levels at water treatment plants needed more frequent monitoring, which was noted at several locations.Reference Ventura, Muhi and de Los Reyes 11 , Reference Ling, Ye and Cai 12 In addition to the increase in gastroenteritis, another condition potentially related to limited sanitation was seen in the increased incidence of infected wounds and abscesses. This was statistically increased during the impact phase and then decreased during the post-impact phase for adults and children.
Even more concerning was the increased number of admissions for pulmonary tuberculosis in adults. The Philippines has the ninth highest incidence of tuberculosis in the world. 13 At the time of Typhoon Haiyan, there were over 26,000 cases of tuberculosis and 356 cases of multi-drug-resistant tuberculosis. 14 Re-establishing treatment and tracking tuberculosis patients became a priority for the Department of Health and the World Health Organization. The increase in tuberculosis cases seen at ODH was likely the result of interruption in treatment of known cases and possibly lack of access to medication owing to migration away from health care facilities. 14 Rapidly reinstating routine tuberculosis control measures after disasters must be a priority.
An increase in vector-borne diseases is another marker of the impact that typhoons have on the routine public health infrastructure. Dengue fever is endemic in the Philippines and there was an outbreak during the post-impact phase. As in previous studies, this suggests that a water-related disaster can increase the availability of mosquito breeding grounds, while reducing routine mosquito control activities, thus allowing dengue fever to spread.Reference Watson, Gayer and Connolly 15
The impact on chronic diseases, specifically high blood pressure and possible strokes, was seen during the post-impact phase. There was a significant increase in hospital admissions related to blood pressure. The government hospital pharmacy was low on medications during the post-disaster response and to prevent this in the future, more medications for chronic illnesses should be stocked in advance. A Médicins Sans Frontières facility during the recovery phase also noted exacerbation of chronic illnesses, acute respiratory infections, and gastrointestinal illnesses.Reference Martinez Garcia and Brown 16
We did not find a significant increase in admissions for injuries during the impact period. Unlike earthquakes, cyclones cause relatively few injuries. However, our injury distribution showed a unique increase in motor vehicle collision-related injuries and fractures compared to previous storms from 1985 through 2011.1 Hurricanes Marilyn and Opal reported 16% motor vehicle collision-related injuries and Hurricane Katrina reported 9%. 17 , 18 A systematic review of injuries in cyclones found injury rates of 3.8% to 4.5%, with lacerations, blunt trauma, and motor vehicle collision-related injuries being the most frequent.Reference Doocy, Dick and Daniels 1 About one-quarter of the injuries at ODH were due to lacerations or stab wounds, which is similar to Hurricanes Elena and Gloria (22%) and Hurricane Hugo (28%), but less than Cyclone Tracy (41%), Hurricane Andrew (49%), Hurricanes Marilyn and Opal (34%), Hurricane Iniki (55%), and Typhoon Saomei (55%). 17 , Reference Mahajani 19 , 20 - Reference Shen, Feng, Zeng and Zhu 23 There was also an increase in accidental kerosene ingestions after Typhoon Haiyan and 3 gasoline ingestion cases were noted after Hurricane Frederic in 1979.Reference Longmire and Ten Eyck 24 With the loss of electricity after the typhoon, kerosene was used for lanterns and cooking. As a result, there were several cases of children with accidental kerosene ingestion during the impact phase, but only one case during the post-impact period because electricity was being restored to the region.
The British Royal Navy conducted a 6-day mission to several affected islands providing outpatient services.Reference Butterworth 25 The most common conditions they treated were soft tissue injuries, infected lacerations, chronic malnutrition, gastrointestinal infections, and many chronic medical conditions (ie, tuberculosis). A national medical rescue team sent by the Chinese government established temporary facilities in Abuyong because the local hospitals were not functioning.Reference Ling, Ye and Cai 12 They provided care for 10 days and of the 827 internal medicine patients, the top diagnosis was tuberculosis, followed by “lung infection.” Although the exact percentages are not given, ODH also had a higher proportion of tuberculosis and pneumonia cases.
There were fewer surgeries after the hospital was damaged. Most of the surgeries during this time period were for appendicitis and bowel obstructions. Noticeably, the percentage of surgeries that were elective dropped from 23.1% during the pre-impact period to 4.7% and 7.8% during the respective impact and post-impact periods. The significantly decreased proportion of elective cases was likely because of the resource-constrained environment. If the surgery needed could be performed electively, during a post-disaster setting, it would be postponed.
Two special population groups had particular needs following the cyclone: pediatrics and obstetrics/gynecology. When the NGO field hospital was operational, there was a decreased cesarian delivery rate and no maternal mortality. In an area devastated by a natural disaster of large magnitude and damaged health care facilities, this is unexpected. Having international aid assist with equipment, resources, and personnel likely contributed to this improvement. This decrease was sustained after ODH was operational again. There were no documented cases of pregnancy complications such as preeclampsia at ODH, which was seen by Médicins Sans Frontières in Tanauan and Tacloban, but these cases may have been seen at other medical facilities in Ormoc City.Reference Martinez Garcia and Brown 16
Pediatric cases increased significantly after the typhoon, but their distribution differed from the outpatient cases reported from a pediatric hospital in Cebu established 7 days after typhoon landfall.Reference Albukrek, Mendlovic and Marom 26 The most common diagnoses at the Cebu hospital were upper respiratory tract infections (36.7%), trauma (10.6%), skin infections (8.7%), otitis (4.2%), and gastroenteritis (4.1%). At ODH, upper and lower respiratory tract infections were 32.4% of all pediatric admissions, whereas these were 40.1% of admissions at the Cebu hospital. Gastrointestinal illness was considerably higher (39.9%) than seen at Cebu (4.1%), but the pre-impact incidence at ODH was known to be elevated (34.1%). Of note, the Israeli Defense Force pediatric hospital was set up 1 week earlier than the one at ODH and only provided services for 11 days. Thus, they may have been able to record more acute but minor trauma cases that did not require admission.
Limitations
The data were derived from written logbooks that had some incomplete entries and unknown acronyms. The logbooks could have been missing entries. The first 6 days of the pre-impact phase were missing. The medical diagnoses were the diagnoses upon admission and not discharge; thus, the actual diagnosis could have been different. Some of the admission diagnoses were listed as symptoms; thus, the actual medical conditions were not recorded. It is unknown whether the patients listed with injuries in the medical logbook had surgeries (if needed) listed in the surgical logbooks. The data were de-identified so repeat patient visits were not accounted for. Another limitation was not having the data from previous years at the same time of year to assess whether some of the trends were due to seasonality. The trends seen in this weather event may not be generalizable to different settings.
Conclusions
ODH had a significantly increased number of cases of infectious diseases, exacerbations of chronic health conditions, and pediatric admissions. Immediate intervention to restore both public health and primary care services may prevent many of these illnesses. Post-cyclone health care needs for hospital planning should focus on preventing and treating infectious diseases, resuming care for chronic conditions as quickly as possible, and providing specialized services for pregnant women and children. In areas with mosquito-borne illness (dengue fever, malaria), vector control should be emphasized.
Acknowledgment
Special thanks to Brixio Echo (Philippines Red Cross) who provided insight on logbook interpretation.









