Disasters may impair people of any community throughout the world at any time. Disasters occur at high frequency and exert wide influence, typically causing property damage, injuries, and death. Reference Hou, Lv and Ding1 Sudden disasters have affected more than 1.5 billion people of the world’s population in the past decade Reference McDermott, Hardstaff and Alpen2 and enforced devastating effects on health and medical infrastructure and posed significant challenges to health systems. Reference Giri, Risnes and Uleberg3,Reference Bambarén, Uyen and Rodriguez4
Hospitals may receive an early warning for some natural disasters, eg, hurricanes and floods, and activate their response plans before the occurrence of an event. However, there is no preventive alert for some other natural disasters, such as earthquakes, at present. Some disasters affect a small number of people: therefore, there is a demand for health systems in a short period of time. Still, some others cause large numbers of casualties, followed by the massive demand for health systems. Reference Mehta5 Hospitals, as the cornerstone of any health system, play a crucial role in response to natural disasters. Reference Pouraghaei, Jannati and Moharamzadeh6,Reference Sauer, McCarthy and Knebel7 Hence, they must be necessarily prepared to respond to disaster and avoid it. Reference Sauer, McCarthy and Knebel7 Following to disasters, necessity increases for health care in the affected areas. In this regard, increasing the capabilities of local hospitals for the management of such unusual situations enjoys the highest priority for disaster mitigation measures. Reference Ochi, Tsubokura and Kato8
Hospital managers play crucial roles in managing potential capacity effectively in disasters. Reference Shabanikiya, Gorgi and Seyedin9 A disaster management program enables the hospital staff to give effective response to disaster. Reference Abd elazeem, Adam and Mohamed10 Although hospital preparedness has been emphasized in many reliable study sources, the results of multiple studies have demonstrated that lack of preparedness and high vulnerability is a significant challenge for hospitals to deal effectively with disasters. Reference Bambarén, Uyen and Rodriguez4,Reference Pouraghaei, Jannati and Moharamzadeh6,Reference Paganini, Borrelli and Cattani11,Reference Seyedin, Abasi Dolat Abadi and Sorani12 For example, the hospitals involved in providing relief to those injured in western Iran by the earthquake, which occurred in November 2017 in the Azgeleh-Sarpol-e-Zahab area of Kermanshah province, included many challenges for disaster response. Reference Ahmadi and Bazargan-Hejazi13 Asefzadeh et al. in a review study examined 15 hospital preparedness surveys from 2007 to 2015. The results indicated that 80% of the studies estimated the hospitals’ preparedness at a moderate level (40-60%) and 13% at a low level. Reference Asefzadeh, Rajaee and Ghamari14
While hospitals are exposed to internal disasters, they also play an important role during the disaster response period. Reference Hendrickx, D’Hoker and Michiels15 Frequent evaluation and monitoring to identify weaknesses and proper planning can contribute to improve the hospital safety level and ultimately improve the quality of hospital services. Reference Etchegaray and Thomas16
Health-care system managers must learn the information required in the field of disaster management and make the necessary planning to have a proper performance in disasters. Reference Amiri, Mohammadi and Khosravi17
Maintenance of capability and performance of hospitals upon disasters is important so that they can respond to a large number of patients who encountered the disaster, when performing their ongoing tasks. Reference Ardalan, Sabzghabaei and Najafi18
It is essential for hospitals to address disaster risk management. Reference Sharifi, Arab and Khosravi19 The purpose of disaster risk management is reduction of underlying risk factors and preparedness for an immediate response to the emergency consequences. Reference Baas, Ramamasy and Dey de Pryck20 Disaster risk management is a holistic approach to all hazards for the whole disaster cycle Reference Ciottone, Biddinger and Darling21 including prevention and mitigation, preparedness, response, and recovery. Reference Schipper and Pelling22
Lack of planning and organization to deal with disasters, hospital unpreparedness, and lack of staff training may damage irrecoverably the health-care system. Reference Ojaghi, Nourizadeh and Mahboubi23 Hospitals may be functionally disrupted by disasters due to the high volume of referrals, over-hospitalization, inadequate training, nonstandard and insufficient education, communication system disorders, etc. Reference Ardalan, Najafi and Sabzghabaie24
Disaster risk management reduces the adverse effects of internal and external events that detrimentally influence the organization’s activity. Reference Zarezade, Abolhasani and Eslami25 Paying attention to risk management-based approaches will be very influential in improving hospital safety. Reference Pretagostini, Gabbrielli and Fiaschetti26 Despite numerous studies carried out to assess hospital disaster risk management, the researcher did not achieve an integrated and comprehensive answer concerning the challenges of hospital disaster risk management. Hence, this study aimed to investigate the challenges of hospital disaster risk management so that it can take a step to provide strategies and interventions to remove these barriers and improve the hospital disaster risk management.
Methods
This study is a systematic literature review and thematic analysis to explore the challenges of hospital disaster risk management. In this study, a systematic review was performed on articles, documents, and reports related to objective of the research. The search time period ranged from January 2010 to January 2020. Persian and international databases included PubMed, Scopus, Web of Science, ProQuest, Google scholar, Sid, Magiran, and Irandoc.
Search components were “Hospital”, “Risk Management”, and “Disaster”. Equivalent words or phrases were obtained in MeSH and Emtree search engines to find the maximum number of articles. In addition, some keywords were completed or revised through related articles or after consultation with experts. The final keywords were divided into 3 groups, as described in Table 1. Then, according to the search engine, the desired syntax was adjusted, and the search was performed (Table 2).
Table 1. Keywords of the study
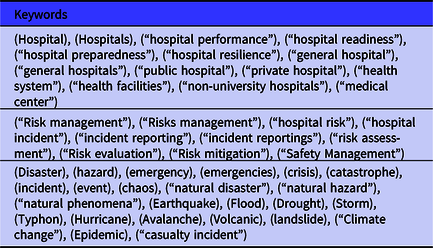
Table 2. Search syntax in PubMed

Inclusion criteria comprised of the types of quantitative, qualitative, and review articles published related to the subject and question of the research, publication in English and Persian, publication date from January 2010 to January 2020, and access to the full text of the articles. Exclusion criteria also included abstracts of congress articles and articles dealing with outside hospital area.
At the end of the search and after deleting duplicate copies, the 2 members of the research team screened articles, books, and documents independently according to their titles and abstracts, taking into account inclusion and exclusion criteria.
The full text of the remaining articles was reviewed by 2 researcher colleagues using a researcher-made form. Low-quality studies or invalid research methods were excluded. The extraction of data from the remaining articles was performed using researcher-made forms. In the event of any dispute, the paper was checked by a third peer, and the research team made the final decision. The forms (critical appraisal checklist and data extraction) were developed and processed during the study.
In addition to a descriptive evaluation in terms of study type and methodology, findings were analyzed relating to the research question and their results, and appropriately selected articles. Thematic analysis of articles was also performed at this stage.
Results
In total, 762 articles and documents were recovered. To avoid repetition, 145 articles were deleted, 414 articles and documents did not meet the objectives of the research, and 191 articles did not follow the eligibility criteria and were excluded. Finally, 12 articles were included in the study. The PRISMA diagram is displayed in Figure 1. The researchers strived to propose honest presentation of results by observance of correct procedure of source writing and intellectual property rights in excerpting the data from the studies.

Figure 1. PRISMA diagram of studies included in the systematic review.
Most documents investigated were qualitative studies. Among them, 7 articles (58.3%) were concerned with Asia, 2 articles (16.6%) on Europe, 2 articles (16.6%) from the United States, and 1 article (8.3%) of Africa were studied. Over 75% of the documents were original articles, and 25% of them included review articles. The results derived from the systematic review are summarized in Table 3.
Table 3. Summary of systematic review results

Thematic Analysis
Based on the given findings, the sources were subjected to the thematic analysis at this phase of study, and the extracted themes were classified, focusing on the thematic variables of the research and summarized in a data table, which included the hospital disaster risk management challenges. The accuracy and perfection of extracted themes were reviewed and confirmed by other members of the research team and some disaster experts. Their results are provided in Table 4.
Table 4. Extracted themes and subthemes as hospital disaster risk management challenges

Discussion
The hospital disaster risk management (HDRM) challenges are as follows.
Technical-Physical Challenges
Structure
Structural change and resetting of physical facilities are among the essential factors to enhance preparedness in disaster response. Reference Aghapour, Yazdani and Jolai27 The results of a study conducted by Montejano-Castillo and Moreno-Villanueva represent that, in many cases, hospitals encounter serious technical constraints imposed by the old age of hospitals and the burnout of buildings. In this respect, it is necessary that new infrastructure to be used for retrofitting or their replacement. Reference Montejano-Castillo and Moreno-Villanueva30 For example, the response of a nonstructural element depends on the safety of the structural element in the event of an earthquake, and the safety of a structural element depends on proper maintenance and the use of seismic technology in its components. Morán-Rodríguez S and Novelo-Casanova in their study, cited the lack of seismic shock retrofitting technology and the requirements of hospitals for proper and periodic maintenance of hospital buildings as reasons for vulnerability in hospitals. Reference Morán-Rodríguez and Novelo-Casanova31
Organizational-Managerial Barriers
Planning
Planning was 1 of the most critical themes extracted from this study. Senior managers’ attention to preventive planning and risk preparedness is a worthwhile investment that is required to be put high on the agenda of the hospital managers. Reference Faghisolouk, Jazani and Sohrabizadeh28 The comprehensive hospital disaster risk management program should cover all hazards, all phases of disaster risk management, and all levels of the hospital. In addition, the necessary resources should be available to managers and employees for the implementation of the disaster risk management plan. 38 Absence of vulnerability assessment program, Reference Radovic, Vitale and Tchounwou34 a large number of decision-making officials, Reference Yarmohammadian, Atighechian and Haghshenas37 and lack of appropriate and well-documented policies and plans to disaster response, are the reasons for the missing of proper hospital disaster risk management. Reference Faghisolouk, Jazani and Sohrabizadeh28,Reference Krishnan and Patnaik29,Reference Morán-Rodríguez and Novelo-Casanova31 For example, the lack of defining evacuation routes and safe points in the hospital for emergencies may be one of the challenges for hospital disaster risk management failures due to absence of appropriate planning. Reference Montejano-Castillo and Moreno-Villanueva30 A written plan is required for preparation but should not lead to “paper plan syndrome” in the hospital. Reviewing and reevaluating disaster plans still remains as significant concern (P7). The absence of a system for monitoring and evaluating the program is one of the most important reasons for the failure of organizational planning. Reference Mosadeghrad and Isfahani39
Surge Capacity
Surge capacity is defined as the ability of an organization for rapid expansion and enhancement of services in response to one or more disasters. Reference Alexander40 A fundamental challenge for planning to surge capacity for disaster recovery is the balance of speed and accuracy. Reference Aghapour, Yazdani and Jolai27 The high pressure outside the hospital, Reference Sammy, Paul and Watson35 poor health systems, Reference Olu, Usman and Manga33 mismanagement of volunteers (related to volunteer recruitment, education, protection mechanisms such as insurance coverage, increased volunteer willingness using incentive mechanisms such as reward systems), Reference Shi, Xu and Gao36 insufficient space to expand emergency activities, shortage of beds for emergency situations, lack of access to hospital in emergencies, Reference Montejano-Castillo and Moreno-Villanueva30 inadequate fire protection equipment, lack of morgue capacity, lack of backup communication facilities, and insufficient means of transport Reference Munasinghe and Matsui32 are among the other challenges posed in the studies associated with surging capacity in hospital disaster risk management.
Communication & Coordination
Many problems of hospital disaster risk management are due to lack of coordination rather than lack of resources. Reference Hendrickx, D’Hoker and Michiels15 Communication and coordination with accountable and supportive foreign organizations, Reference Nekoie-Moghadam, Kurland and Moosazadeh41,Reference Avery and Zabriskie-Timmerman42 as well as national interdisciplinary coordination, leads to correct management. Reference Avery and Zabriskie-Timmerman42 Effective hospital communication and coordination with other organizations and healthcare providers is essential to achieve the best disaster response and provide the optimal healthcare services to disaster casualties. Reference Hendrickx, D’Hoker and Michiels15,Reference Adini, Goldberg and Laor43 Ineffective communication and coordination in the crisis team for various reasons, including inadequate backup communication facilities and the lack of presence and deployment of hospital emergency incident command system (HEICS), are among the challenges and reasons for failure in hospital disaster risk management. Reference Hendrickx, D’Hoker and Michiels15,Reference Munasinghe and Matsui32,Reference Yarmohammadian, Atighechian and Haghshenas37 The successful response to the crisis requires coordination between all departments of the hospital, and cooperation and coordination with the prehospital emergency forces, the Red Crescent, Police, and the fire department, and ensuring the establishment of communication lines. HEICS provides more coordination between hospitals and other organizations involved in emergency events using a logical management structure, job description, generation of clear reporting channels, and creating a common naming system. It necessitates for developing training courses in HEICS for hospital administrators and creating and organizing it in hospitals. Reference Yarmohammadian, Atighechian and Haghshenas37
Rules and Regulations
Presence of bureaucracy, Reference Montejano-Castillo and Moreno-Villanueva30 lack of law for the regulation and standardization of hospital disaster response programs, Reference Krishnan and Patnaik29,Reference Yarmohammadian, Atighechian and Haghshenas37 the involvement of administrative managers in activities, constant changes in rules, Reference Yarmohammadian, Atighechian and Haghshenas37 followed by the lack of enforcement of regulations for prevention and disaster risk reduction Reference Morán-Rodríguez and Novelo-Casanova31 are the challenges concerning rules and regulations in the implementation of hospital disaster risk management. Hence, some vital measures include preparation of legal guidelines for hospitals and regulatory requirements for their implementation, removing complex and restrictive administrative processes, including emergency incidents management in the job descriptions of managers, and evaluating hospital managers related to them. Reference Yarmohammadian, Atighechian and Haghshenas37
Political Will and Commitment
Rapid change in appointed officers, Reference Montejano-Castillo and Moreno-Villanueva30 lack of commitment of managers, Reference Olu, Usman and Manga33,Reference Yarmohammadian, Atighechian and Haghshenas37 and insufficient political will Reference Olu, Usman and Manga33 due to unfavorable political atmosphere Reference Shi, Xu and Gao36 are the key challenges raised upon implementation of hospital disaster risk management strategies regarding lack of commitment and political will. When senior managers of hospitals are not committed to implementing risk management programs, employees will not feel their own resonsibility for the committed performance of the organization’s agenda. The absence of senior executives in meetings and committees, lack of their striving to change the policies, structure, and culture of the organization indicates to the employees of the organization that there is no serious consensus among managers in the organization to implement the program. Reference Wiesman, Melnick and Bright44
Culture, Motivation
The absence of a risk reduction culture and administrative culture for crisis management Reference Montejano-Castillo and Moreno-Villanueva30,Reference Yarmohammadian, Atighechian and Haghshenas37 and the lack of development of hospital risk management culture Reference Sammy, Paul and Watson35 were among the barriers to implementation of hospital disaster risk management related to culture. The lack of officials support Reference Yarmohammadian, Atighechian and Haghshenas37 was one of the other challenges posed in the studies. Poor incentives Reference Sammy, Paul and Watson35 and the lack of a competitive environment to improve the status quo result in a lack of motivation and a sense of need for hospital disaster risk management. Reference Yarmohammadian, Atighechian and Haghshenas37 The role of leadership in creating motivation among employees, creating of voluntary service culture, and supporting and accompanying employees are very crucial in the implementation of disaster risk management programs. The organization should have an appropriate appreciation and reward system, and employees should be appreciated and rewarded for the execution of the organizational program. Reference Moseley45
Knowledge
Risk management is not carried out scientifically in most hospitals in Iran. Reference Faghisolouk, Jazani and Sohrabizadeh28 Some organizational factors, including inadequate data collection, Reference Sammy, Paul and Watson35 cause a lack of awareness of existing vulnerability problems. Reference Morán-Rodríguez and Novelo-Casanova31 The other reasons for the weakness of hospital disaster risk management include the absence of scientific and academic programs on disaster management Reference Radovic, Vitale and Tchounwou34 and the lack of scientific evidence on the flow of disaster risk management in long-term development plans. Reference Olu, Usman and Manga33 It is essential that the necessary training related to the development and implementation of risk management programs to be provided for the managers so that a new attitude be created among them in this area. Reference Faghisolouk, Jazani and Sohrabizadeh28
Financial Barriers
Budget
Multiple studies demonstrate that a lack of financial resources is a significant barrier versus proper preparedness to deal with disasters. Reference Montejano-Castillo and Moreno-Villanueva30,Reference Mortelmans, Van Boxstael and De Cauwer46 Budget allocation to preparedness and response to health emergencies should be based on gaps or needs analysis. Reference Munasinghe and Matsui32 The results of the study carried out by Montejano-Castillo and Moreno-Villanueva indicate that, in many cases, hospitals do not have sufficient financial resources, despite presence of a safety index and accurate assessment tools. Lack of funds (budget) makes it difficult to update some equipment or recruit more staff or build more rooms to expand the hospitals. Reference Montejano-Castillo and Moreno-Villanueva30 The absence of clear and adequate financial resources for disaster risk management Reference Montejano-Castillo and Moreno-Villanueva30,Reference Olu, Usman and Manga33 and prevention programs, vulnerability reduction projects, and hospital autonomy granting operations within 3-5 d after the occurrence of a disaster Reference Morán-Rodríguez and Novelo-Casanova31 are among the financial barriers pointed out in various studies, which can disrupt hospital disaster risk management by creating adverse consequences such as inability to deploy and implement the HEICS Reference Yarmohammadian, Atighechian and Haghshenas37 and update existing equipment. Reference Montejano-Castillo and Moreno-Villanueva30
Human Barriers
Education and Exercise
Education and exercise will lead to an increase in the knowledge and skills of hospital health professionals Reference Munasinghe and Matsui32 and enhancement in their preparedness. Reference Arab, Khankeh and Mosadeghrad47 Lack of public empowerment, Reference Sammy, Paul and Watson35,Reference Yarmohammadian, Atighechian and Haghshenas37 insufficient knowledge in managers, Reference Faghisolouk, Jazani and Sohrabizadeh28,Reference Yarmohammadian, Atighechian and Haghshenas37 and scarcity of experienced and competent managers Reference Yarmohammadian, Atighechian and Haghshenas37 are important reasons for the absence of proper hospital risk management. Thus, using specialized and trained people in the field of crisis management in various departments along with hospital preparedness Reference Munasinghe and Matsui32 and the appointment of qualified and competent managers Reference Yarmohammadian, Atighechian and Haghshenas37 are assumed as necessary actions. Hospitals will not enjoy appropriate response capacity without effective education. Reference Reilly and Markenson48 In this respect, Munasinghe and Matsui, in their study, considered the unpreparedness of the Sri Lankan hospital mainly due to insufficient education and exercise. Reference Munasinghe and Matsui32
Commitment, Motivation, Culture, Staff Shortage
The reactive and nonpreventive treatment in all hospitals is also one of the barriers that prevents hospital staff being involved in hospital safety works. Lack of risk reduction culture in hospitals, absence of commitment Reference Montejano-Castillo and Moreno-Villanueva30 and motivation in managers and employees, Reference Montejano-Castillo and Moreno-Villanueva30,Reference Yarmohammadian, Atighechian and Haghshenas37 their willingness to carry out preventive measures immediately after the occurrence of a disaster and not before it, Reference Montejano-Castillo and Moreno-Villanueva30 and staff shortage Reference Sammy, Paul and Watson35 are among the hospital disaster risk management challenges regarding human resources that must be taken into account seriously. Motivated and committed employees are more involved in the organization and play a substantial role in achievement of the organization. Reference Mosadeghrad, Ebneshahidi and Abdolmohammadi49 Given the occurrence of previous losses, educating and informing of managers at all levels is an essential point for promotion of a risk reduction culture in hospitals. Reference Montejano-Castillo and Moreno-Villanueva30
Conclusion
With regard to rising occurrences of disasters and their adverse effects on the health-care systems, especially hospitals, and the importance of implementing hospital disaster risk management, policy-makers and managers need to be aware of these challenges so that they can upgrade the hospital disaster risk management by finding strategies and solutions to implement them and eliminate these obstacles. The challenges of HDRM were raised in the form of 4 main themes: technical-physical barriers, organizational-managerial barriers, financial barriers, and human barriers in this study. They also included 17 sub-themes (inappropriate physical structure, lack of proper planning, the inadequate capacity surging, lack of communication and coordination, inadequacy of rules and regulations, lack of commitment and political will, absence of risk reduction culture within the organization and among staff, lack of organizational motivation, insufficient knowledge, lack of budget, inadequate education and exercise, lack of motivation among staff, absence of commitment among staff, and staff shortage due to the crisis). The recognition of these challenges can help develop a roadmap to improve hospital disaster risk management. The limitation of this research was that the methodology of the studies was not similar, and the instruments used in different studies were not the same.
Suggestions for Future Research
This study was designed and performed merely to examine the challenges of hospital disaster risk management. The researchers recommend conducting further investigations aimed at exploring strategies to improve the hospital disaster risk management, examining the impact of the implementation of strategies for upgrading the hospital disaster risk management, and conducting systematic reviews of studies published after 2020.
Acknowledgments
The authors thank the distinguished referees who contributed to the quality of this study with their constructive comments.
Author Contributions
All authors participated in data analysis, preparing the initial version and revising the article. Finally, all of them approved the final version for publication.
Conflict of Interests
The authors have no conflict of interest in this work.
Ethics Approval
This study is part of the PhD thesis was approved by the Research Ethics Committee of the Aja University of Medical Sciences by obtaining the ethics code IR.AJAUMS.REC.1398.251.







