Maternal depressive symptoms are well-documented risk factors for childhood externalizing behaviors (Burke, Reference Burke2003; Cummings, Keller, & Davies, Reference Cummings, Keller and Davies2005; Farmer, McGuffin, & Williams, Reference Farmer, McGuffin and Williams2002; Garber & Cole, Reference Garber and Cole2010; Kouros & Garber, Reference Kouros and Garber2010; Piche, Bergeron, Cyr, & Berthiaume, Reference Piche, Bergeron, Cyr and Berthiaume2011). There is evidence that the high frequency of externalizing behaviors in the toddler years declines significantly through early childhood, and persistence of these behaviors may indicate a risk for the development of aggressive and disruptive behaviors in adolescence and adulthood (Larsson, Viding, Rijsdijk, & Plomin, Reference Larsson, Viding, Rijsdijk and Plomin2008). Externalizing behaviors are two to five times more prevalent in children of mothers displaying clinical levels of depressive symptoms (Bergeron et al., Reference Bergeron, Valla, Breton, Gaudet, Berthiaume, Lambert and Smolia2000; Campbell, Reference Campbell1995; Davies & Cicchetti, Reference Davies and Cicchetti2014; Ford, Goodman, & Meltzer, Reference Ford, Goodman and Meltzer2004; Kouros & Garber, Reference Kouros and Garber2010). This association was confirmed for different age groups: 2–3 years, 6–8 years, 9–11 years, and 12–14 years (Bergeron et al., Reference Bergeron, Valla, Breton, Gaudet, Berthiaume, Lambert and Smolia2000; Martin, Clements, & Crnic, Reference Martin, Clements and Crnic2011).
Despite numerous studies focusing on the developmental consequences of maternal depressive symptoms in young children, most of these relied on cross-sectional data. A limited number of studies longitudinally modeled maternal depressive symptom trajectories, and even fewer considered children's behavioral problems associated with these trajectories (Campbell, Matestic, von Stauffenberg, Mohan, & Kirchner, Reference Campbell, Matestic, von Stauffenberg, Mohan and Kirchner2007; Campbell, Morgan-Lopez, Cox, & McLoyd, Reference Campbell, Morgan-Lopez, Cox and McLoyd2009; Matijasevich et al., Reference Matijasevich, Murray, Cooper, Anselmi, Barros, Barros and Santos2015; Van Der Waerden et al., Reference Van Der Waerden, Galéra, Larroque, Saurel-Cubizolles, Sutter-Dallay and Melchior2015). Although these studies were longitudinal, they measured the children's behavioral problems as a fixed outcome. Three recent studies, all using data from Early Step Multisite Study (recruited from Women, Infants, and Children program participants), investigated both maternal depressive symptoms and child behavioral problems longitudinally (Choe, Shaw, Brennan, Dishion, & Wilson, Reference Choe, Shaw, Brennan, Dishion and Wilson2014; Hails, Reuben, Shaw, Dishion, & Wilson, Reference Hails, Reuben, Shaw, Dishion and Wilson2017; Shaw, Sitnick, Reuben, Dishion, & Wilson, Reference Shaw, Sitnick, Reuben, Dishion and Wilson2016), and addressed the nature of the association between these two processes. The current study aims to add to this literature by examining the longitudinal association of maternal depressive symptoms with child externalizing behaviors while disaggregating the interindividual and intradyad sources of this association.
Aggression, hyperactivity, and oppositionality are normative for toddlers prior to 2 years of age (Maccoby, Reference Maccoby1980). Overt forms of aggressive behaviors peak toward the end of the second year, and start to decline thereafter (Tremblay, Reference Tremblay2000). There is a developmental transition when the externalizing behaviors become atypical (Granic & Patterson, Reference Granic and Patterson2006). Toddlers displaying high levels of these behaviors, and children still exhibiting these behaviors after toddlerhood, were shown to be at a significant risk for continued behavior problems (Campbell, Shaw, & Gilliom, Reference Campbell, Shaw and Gilliom2000; Gilliom & Shaw, Reference Gilliom and Shaw2004; Mesman, Bongers, & Koot, Reference Mesman, Bongers and Koot2001). The transition when typical behaviors become atypical may be triggered by a number of factors, among which are maladaptive parenting behaviors, such as hostile, disengaged, or overly permissive responses to children's acting out behaviors (Belsky, Woodworth, & Crnic, Reference Belsky, Woodworth and Crnic1996; Shaw et al., Reference Shaw, Winslow, Owens, Vondra, Cohn and Bell1998).
Early childhood may be a period when children are especially vulnerable to negative developmental outcomes of maternal depressive symptoms. During this period, children depend on their primary care givers for self-regulation, socialization, and care. Kim-Cohen, Moffitt, Taylor, Pawlby, and Caspi (Reference Kim-Cohen, Moffitt, Taylor, Pawlby and Caspi2005) found that maternal depressive symptoms during the child's first 5 years made a unique contribution to their behavioral problems over and above their genetic liability and other co-occurring family risk factors. The heightened vulnerability of children to maternal depressive symptoms in early childhood may arise because children are particularly dependent on their mothers for initiating interactions during this period, and have limited exposure to social settings outside the home (Jaffe & Poulton, Reference Jaffee, Poulton, Huston and Ripke2006; Radke-Yarrow & Klimes-Dougan, Reference Radke-Yarrow, Klimes-Dougan, Goodman and Gotlib2002).
The Cultural Context of the Current Study
In the current study, we use data from a longitudinal and nationally representative survey of families, collected when children were between the ages of 3 and 7, in Turkey. Two important characteristics of the cultural context of this study must be highlighted: the prevalence of patriarchal values and practices, and collectivism. Turkish families are overwhelmingly patriarchal, where a gender-based division of household responsibilities prevail, and fathers tend to have a limited role in the day-to-day caring of young children (Kagitcibasi & Ataca, Reference Kagitcibasi and Ataca2005). Few mothers work and few children attend preschool (OECD, 2010). In the current sample, 98% of children at age 3, 94% at age 4, and 91% at age 5 remained in maternal care, underscoring the overwhelming importance of maternal parenting. In contrast, in the United States, 47% of children at age 3, 68% at age 4, and 94% at age 5 attended preschool or kindergarten (OECD, 2010).
The salience of the motherhood role will be high when women have few roles outside the home. In the current sample, only 13%–21% of the mothers worked outside their homes during child ages 3–7. The economic dependency of the mothers, the lack of availability of roles outside the household, and the hierarchical patriarchal culture (power distance index of 66%; Hofstede, Hofstede, & Minkov, Reference Hofstede, Hofstede and Minkov2010) result in an imbalance of power in the family, favoring the fathers. These conditions constitute an elevated risk for all types of spousal abuse (Haj-Yahia, Reference Haj-Yahia2005).
Based on Hofstede's collectivism-to-individualism ranking, Turkey is 37th out of 93 countries (Hofstede et al., Reference Hofstede, Hofstede and Minkov2010), located closer to the collectivistic end of this distribution. Collectivism is associated with a high value attributed to family connectedness. Three implications of collectivism are relevant for the current study. First, almost all of the mothers in the current sample are married with the biological fathers of their children. Marital disruptions are rarely experienced by the children in Turkey, owing to the low rates of divorce. In this sample, .01% and .03% were divorced when the children were 3 and 7, respectively. Second, the goal of protecting the unity of the family is often associated with an emphasis on parental authority, and obedience-oriented socialization, as well as the protective care of young children. These values often coexist with parental harsh discipline (Kagitcibasi, Reference Kagitcibasi1996). Previous studies documented that Turkish parents used high levels of intrusive and harsh strategies in disciplining their children (Akcinar & Baydar, Reference Akcinar and Baydar2014).
The third implication of collectivism pertains to the expression of depressive symptoms. Depressive symptoms typically include low mood (sadness, worrying, low self-esteem, and anger), social withdrawal, disrupted sleep patterns, forgetfulness, psychomotor retardation, attention problems, agitation, low energy levels, inability to feel pleasure, and low motivation (American Psychiatric Association, 2000). However, previous studies indicated that in collectivistic cultures, depressive symptoms may present themselves as somatic symptoms, in addition to the common symptoms of depression (Kirmayer, Reference Kirmayer2001). Moreover, an early cross-cultural study of self-reported depressive symptoms established that somatic presentation of depressive affect was highly common across cultures, but especially so in collectivistic cultures (Simon, VonKorff, Piccinelli, Fullerton, & Ormel, Reference Simon, VonKorff, Piccinelli, Fullerton and Ormel1999). Maintaining group harmony is a central goal in collectivistic cultures, and open expression of negative emotions is a threat to that harmony (Hook, Worthington, & Utsey, Reference Hook, Worthington and Utsey2009; Jongwoo et al., Reference Jongwoo, Sunyong, Junghye, Dongkun, Leeheon and Minsoo2004). Zaroff, Davis, Chio, and Madhavan (Reference Zaroff, Davis, Chio and Madhavan2012) argued that, due to their need to maintain group harmony, individuals from collectivistic cultures were more likely to report somatic symptoms of depression than psychological symptoms. In the current sample, the mean scale scores were approximately twice those reported for the original community sample used for scale development (M = 0.59, SD = 0.74 vs. M = 0.28, SD = 0.46 for depressive symptoms, respectively; Derogatis & Melisaratos, Reference Derogatis and Melisaratos1983).
The Link Between Maternal Depressive Symptoms and Child Externalizing Behaviors
The association of maternal depressive symptoms with child externalizing behaviors may involve several mechanisms. A genetic factor may render both the mother and the child vulnerable to adjustment problems (Clarke, Flint, Attwood, & Munafo, Reference Clarke, Flint, Attwood and Munafo2010; Davies & Cicchetti, Reference Davies and Cicchetti2014). Alternatively, a confounding environmental factor may be predictive of both maternal depressive symptoms and child externalizing behaviors (e.g., the presence of an abusive husband/father; Artazcoz, Benach, Borrell, & Cortes, Reference Artazcoz, Benach, Borrell and Cortes2004; Cummings, Goeke-Morey, & Papp, Reference Cummings, Goeke-Morey and Papp2004; Kalmijn & Monden, Reference Kalmijn and Monden2006; Kouros, Cummings, & Davies, Reference Kouros, Cummings and Davies2010). In the current sample, where patriarchal values are prevalent and mothers tend to be economically dependent on their husbands, factors associated with the father may be especially salient.
A third hypothesis is that the children's externalizing behaviors may contribute to the mothers’ depressive symptoms. Parenting a child with externalizing behaviors may present challenges for the mothers. Mothers of children with high levels of behavioral disruptions reported high levels of depressive symptoms (Elgar, McGrath, Waschbusch, Stewart, & Curtis, Reference Eamon and Zuehl2004). Previous research also suggested that the parents lost their confidence in their parenting abilities when children displayed externalizing behaviors. A lack of parenting self-efficacy was, in turn, associated with parenting stress and parental depressive symptoms (Farmer & Lee, Reference Farmer and Lee2011; Nelson, Hammen, Brennan, & Ullman, Reference Nelson, Hammen, Brennan and Ullman2003). Further evidence of a causal link between parenting mastery and depressive symptoms came from parenting interventions, which demonstrated that increases in parenting self-efficacy alleviated depressive symptoms (Beauchaine, Webster-Stratton, & Reid, Reference Beauchaine, Webster-Stratton and Reid2005).
The link from child externalizing behaviors to maternal depressive symptoms may be particularly salient in the cultural context of the current study. Based on Bandura's (Reference Bandura1989) theory of self-efficacy, the salience of the motherhood role is expected to be associated with the strength of the association of parenting self-efficacy with depressive symptoms.
A fourth hypothesis is that maternal depressive symptoms may lead to child externalizing behaviors. Depressive symptoms are known to reduce the capacity for mood regulation (Joormann, Siemer, & Gotlib, Reference Joormann, Siemer and Gotlib2007). Therefore, the mothers who have high levels of depressive symptoms may not effectively model regulation. Children who have an opportunity to observe models who successfully regulate a wide range of emotions are likely to be able to regulate their frustration and anger (Granic & Patterson, Reference Granic and Patterson2006). Previous studies showed that children with depressed mothers exhibited more negative affect, poorer affect regulation, more behavior problems, less cooperation, less frustration tolerance, poorer social skills, and were rated higher on externalizing behaviors than children of mothers without depressive symptoms (Campbell et al., Reference Campbell, Matestic, von Stauffenberg, Mohan and Kirchner2007; Kopp, Reference Kopp1989). One study confirmed the specific role of inhibitory control in the link between maternal depression and oppositional behavior (Choe et al., Reference Choe, Shaw, Brennan, Dishion and Wilson2014).
In addition to this direct link between maternal depressive symptoms and child externalizing behaviors, two indirect processes may operate via parenting behaviors. Maternal depressive symptoms (e.g., fatigue, difficulty in concentrating, and low interest in daily activities) are risk factors for a harsh or nonresponsive approach to the child, leading to adverse psychosocial outcomes in children (Field, Reference Field1992; Giallo, Cooklin, & Nicholson, Reference Giallo, Cooklin and Nicholson2014; Wang, Wu, Anderson, & Florence, Reference Wang, Wu, Anderson and Florence2011). Depressive symptoms were associated with maternal negativity and harsh parenting (Carter, Garrity-Rokous, Chazen-Cohen, Little, & Briggs-Gowan, Reference Carter, Garrity-Rokous, Chazen-Cohen, Little and Briggs-Gowan2001; Turney, Reference Turney2012) partly due to the mothers’ negative evaluations of themselves and their children (Goodman et al., Reference Goodman, Rouse, Connell, Broth, Hall and Heyward2011). Past findings indicated that mothers with high depressive symptoms perpetuated (or even unwittingly encouraged) externalizing behaviors because they perceived high levels of child negativity, selectively responded to misbehavior, and responded harshly and coercively to misbehavior (Eamon & Zuehl, Reference Eamon and Zuehl2001; Elgar et al., Reference Elgar, McGrath, Waschbusch, Stewart and Curtis2004; Granic & Patterson, Reference Granic and Patterson2006; Harnish, Dodge, Valente, & Conduct Problems Prevention Research Group, Reference Harnish, Dodge and Valente1995).
Elevated depressive symptoms may also lead to a lack of maternal responsiveness and engagement (Carter et al., Reference Carter, Garrity-Rokous, Chazen-Cohen, Little and Briggs-Gowan2001; Elgar et al., Reference Elgar, McGrath, Waschbusch, Stewart and Curtis2004; Turney, Reference Turney2012), that may lead to compromised mother–child attachment (Atkinson et al., Reference Atkinson, Paglia, Coolbear, Niccols, Parker and Guger2000; Martins & Gaffan, Reference Martins and Gaffan2000) especially in early childhood. Specifically, children of mothers who had depressive symptoms displayed high rates of attachment insecurity (Campbell et al., Reference Campbell, Brownell, Hungerford, Spieker, Mohan and Blessing2004). Most important, insecure attachment was associated with maladaptive socioemotional outcomes for the child (Elgar et al., Reference Elgar, McGrath, Waschbusch, Stewart and Curtis2004).
Several studies examined the effects of maternal depressive symptom trajectories on children's behavioral outcomes. Some of these studies modeled depressive symptom trajectories starting from pregnancy (Cents et al., Reference Cents, Diamantopoulou, Hudziak, Jaddoe, Hofman, Verhulst and Tiemeier2013; Guyon-Harris, Huth-Bocks, Lauterbach, & Janisse, Reference Guyon-Harris, Huth-Bocks, Lauterbach and Janisse2016; Van Der Waerden et al., Reference Van Der Waerden, Galéra, Larroque, Saurel-Cubizolles, Sutter-Dallay and Melchior2015), and others starting from infancy and early childhood (Campbell et al., Reference Campbell, Matestic, von Stauffenberg, Mohan and Kirchner2007, Reference Campbell, Morgan-Lopez, Cox and McLoyd2009; Gross, Shaw, Burwell, & Nagin, Reference Gross, Shaw, Burwell and Nagin2009; Matijasevich et al., Reference Matijasevich, Murray, Cooper, Anselmi, Barros, Barros and Santos2015). These longitudinal studies found that children of mothers who had increasing, chronic, and/or high depressive symptom trajectories had higher levels of behavior problems than children whose mothers had low or decreasing trajectories of depressive symptoms.
In the light of the above review, we hypothesized that the association of maternal depressive symptoms with child externalizing behaviors would be bidirectional. A few previous studies had similar goals (e.g., Choe et al., Reference Choe, Shaw, Brennan, Dishion and Wilson2014; Hails et al., Reference Hails, Reuben, Shaw, Dishion and Wilson2017; Shaw et al., Reference Shaw, Sitnick, Reuben, Dishion and Wilson2016) and examined the transactional associations of maternal depressive symptoms with children's behavioral problems in a single sample of Women, Infants, and Children program participants (except for Shaw et al., Reference Shaw, Sitnick, Reuben, Dishion and Wilson2016, who used data from an additional study of Women, Infants, and Children program participants). Only one of these studies also included the indirect associations of parent–child coercive interactions in their transactional model (Hails et al., Reference Hails, Reuben, Shaw, Dishion and Wilson2017).
All three studies estimated typical transactional path models that were augmented with potential exogenous confounding processes (e.g., neighborhood deprivation) or mediating processes (e.g., inhibitory control or harsh parenting). When typical transactional path models are estimated, the transactional effects between the first two time points must be interpreted cautiously. The effects from the baseline observation to the first follow-up confounds all shared fixed predictors of the two processes that are not included in the model, and therefore may be overestimated. All three studies reviewed here (Choe et al.; Reference Choe, Shaw, Brennan, Dishion and Wilson2014, Hails et al., Reference Hails, Reuben, Shaw, Dishion and Wilson2017; Shaw et al., Reference Shaw, Sitnick, Reuben, Dishion and Wilson2016) found transactional effects during the first two time points. Thereafter, transactional effects were very small or nonsignificant. Instead, there was more empirical evidence supporting child-to-mother effects than mother-to-child effects after age 3. The only exception was the weak bidirectional association for ages 4 to 5. Note that this period probably coincided with the transition to kindergarten, and the maternal depressive affect might have diminished the mother's support for the child during this transition.
We added to this body of research in two ways. First, we examined the transactional associations of maternal depressive symptoms with child externalizing behaviors using annual follow-up data spanning ages 3–7, from a large, nationally representative, non-Western sample. Second, we addressed the question of between-dyad and within-dyad associations of maternal depressive symptoms and child externalizing behaviors. This effort had the potential to inform theoretical questions about the association of the two processes and its implications for policy.
We anticipated that the levels of and changes in both maternal depressive symptoms and child externalizing behaviors would be positively associated. We also expected that the within-person change in maternal depressive symptoms would be positively associated with the within-person change in the child's externalizing behaviors. We controlled for the associations of three factors with maternal depressive symptoms and child's externalizing behaviors: harassment of the mother by her spouse, child gender, and family socioeconomic status (SES) at the time of the baseline interview. Previous research indicated that boys exhibited higher levels of externalizing behaviors than girls (Prinzie et al., Reference Prinzie, Onghena, Hellinckx, Grietens, Ghesquiere and Colpin2004), and SES was associated with severe and chronic depressive symptoms (McLennan, Kotelchuck, & Ch, Reference McLennan, Kotelchuck and Ch2001; Pascoe, Stolfi, & Ormond, Reference Pascoe, Stolfi and Ormond2006; Rehman, Gollan, & Mortimer, Reference Rehman, Gollan and Mortimer2008).
Much research indicated strong associations of maternal depressive symptoms with harsh parenting practices, and harsh parenting practices with children's externalizing behaviors (Lengua, Reference Lengua2006; Maccoby, Reference Maccoby2000; Prinzie et al., Reference Prinzie, Onghena, Hellinckx, Grietens, Ghesquiere and Colpin2004). In order to better understand the transactional process that links maternal depressive symptoms and child externalizing behaviors, we estimated a model where harsh parenting behaviors mediated the lagged mother-to-child and child-to-mother transactional associations of maternal depressive symptoms and child externalizing behaviors. This model represented the following two mediational transactional hypotheses: (a) an increase in maternal depressive symptoms could lead to harsh parenting, which, in turn, could result in an increase in child externalizing behaviors; and (b) an increase in child externalizing behaviors could lead to negative responses of the mother to the child (i.e., harsh parenting), which, in turn, could result in an increase in maternal depressive symptoms. This latter association could result from the deteriorating mother–child relationship and a sense of loss of parenting self-efficacy.
Method
Our data were from a 5-year longitudinal survey that focused on early childhood and its developmental ecology.
Participants
The participants consisted of 1,052 children and their families. They constituted a nationally representative sample from 19 provinces in Turkey. This sample was a multistage geographical cluster sample, with probabilities of selection at each stage proportional to the population size. In order to confirm the representativeness of the sample, characteristics of the families were compared to the national data from the Study of Family Structure, conducted by the Turkish Statistical Institute (2006). Families from both studies were almost identical in terms of rural/urban residence, level of education of the mothers, and the marital status of the parents (for further details, see Baydar & Akcinar, Reference Baydar and Akcinar2015). Children were first assessed when they were between 36 and 47 months of age, and then annually through age 7.
Procedure
Mothers and the focal children were visited in their homes annually. The visits lasted approximately 1 hr and 45 min. During these visits, the mothers and the children were assessed, interviewed, and observed in an alternating sequence. The following measures were used in the current study: maternal depressive symptoms (ages 3–7), children's externalizing behaviors (ages 3–7), indicators of SES (at age 3), children's gender, mothers’ reports on spousal harassment (at age 3), and maternal self-reports and observational data on parenting behaviors (ages 3–4).
Measures
All of the measures that were used in this study were scaled in order to ensure the stability of the numerical procedures that were required for the estimation of the models presented here.
Maternal depressive symptoms scores were based on a subset of items of the Turkish adaptation of the Brief Symptom Inventory (BSI; Sahin & Durak, 1994) that was administered annually. The original BSI (Derogatis, Reference Derogatis1993) was a 53-item self-report measure of psychiatric symptoms, where each item was rated on a 5-point Likert scale. Two items were adapted in Turkish version of the scale due to a lack of Turkish words that corresponded to the original wording of the items. The item “feeling blue” was replaced with 2 items, “feeling tearful” and “feeling sad.” The item “feeling fearful” was deleted because “feeling scared” and “feeling fearful” do not correspond to distinct Turkish words. The remaining items were verbatim translated to Turkish.
In this research, we created a measure of depressive symptoms that could include the atypical symptoms of maternal depression that were likely to be reported in a collectivistic culture, in addition to the typical symptoms of depressive symptoms. Several previous studies examining self-reported maternal depressive symptoms in Western cultures also considered symptoms of anxiety alongside the typical symptoms of depression. Azak and Raeder (Reference Azak and Raeder2013), Piche et al. (Reference Piche, Bergeron, Cyr and Berthiaume2011), and Skipstein, Janson, Kjeldsen, Nilsen, and Mathiesen (Reference Skipstein, Janson, Kjeldsen, Nilsen and Mathiesen2012) all investigated maternal depressive and anxiety symptoms together. In a large cross-cultural study of depression, 95% of patients diagnosed with depression in Turkey presented with somatic symptoms, although few (5%) denied typical psychological symptoms (Simon et al., Reference Simon, VonKorff, Piccinelli, Fullerton and Ormel1999).
Our analyses showed that the depression subscale was highly correlated with the anxiety (r = .82, p < .001) and somatization (r = .59, p < .001) subscales of the BSI. The somatization and anxiety subscales were also highly correlated (r = .66, p < .001). Factor analyses of the combined items of the three subscales identified a single factor for the items from each wave of data, and the percentage of total variance accounted for by that factor ranged from 38.9%–43.9%. Therefore, items from the depression (e.g., “Feeling lonely even with others”), anxiety (e.g., “Feeling so restless can't sit still”), and somatization (e.g., “Feeling weak”) subscales were combined to create a 17-item combined scale (range 0–4). While this combined measure assessed generalized internalizing symptoms, we referred to it as the depressive symptoms scale in order to preserve the comparability of this label to the previous studies that also used combined scales. Internal reliability of the combined depressive symptoms scale ranged from α = 0.90 to 0.92 for ages 3–7.
Our data partially supported our premise that collectivistic and traditional attitudes might be associated with the reporting of psychological symptoms as somatic symptoms. For example, the symptoms of depression were lower among the rural than the urban mothers (M = 0.54 vs. M = 0.64, respectively), F (1, 1,052) = 5.18, p = .023. Somatic symptoms were also higher among the mothers who were living in households of five or more than the mothers who were living in smaller households (M = 0.69 vs. M = 0.53, respectively), F (1, 1,052) = 16.57, p < .001. However, the reports of somatic symptoms did not differ significantly by rural/urban status (M = 0.61 vs. M = 0.59), F (1, 1,052) = 0.24, p = .626, and the reports of depressive symptoms did not differ significantly by the household size (M = 0.57 vs. M = 0.63), F (1, 1,052) = 1.76, p = .186.
Child externalizing behaviors were assessed annually with the Eyberg Child Behavior Inventory (ECBI; Eyberg & Robinson, Reference Eyberg and Robinson1983). The original ECBI was a 36-item parent-report rating scale, assessing both the type and the intensity of behavior problems in children between the ages of 2 and 16. The ECBI was adapted to Turkish by Batum and Yağmurlu (Reference Batum and Yağmurlu2007). The Turkish adaptation used here had a 5-point Likert scale in order to make it easy to respond for the mothers who had a very low level of education (69.0% of the mothers had 5 or fewer years of education). The scale was adapted to Turkish through a translation and back-translation procedure. The item “steals” was adapted to “takes other people's belongings without permission,” because of the stigma associated with reporting that one's child may be a “thief” (Batum & Yağmurlu, Reference Batum and Yağmurlu2007). Slight adaptations were made to 2 items in order to render them culturally appropriate (e.g., “physically/verbally fights with sisters, brothers and other children in the extended family” instead of “physically/verbally fights with sisters and brothers”). We used all 36 items (e.g., “Fights with peers,” “whines,” and “has temper tantrums”). High scores indicated diverse types of and/or frequent occurrence of behavior problems (range 0–4, α = 0.93 to α = 0.94 for ages 3–7).
Harsh parenting behaviors at ages 3 and 4 were used in this study. We constructed a measure of harsh parenting by combining the self-report punishment subscale scores from the Parenting Questionnaire (PQ; Paterson & Sanson, Reference Paterson and Sanson1999), and observer reports on harsh behaviors of the mother from the Home Observation for the Measurement of the Environment (HOME-TR; Bradley, Corwyn, Burchinal, McAdoo, & Garcia-Coll, Reference Bradley, Corwyn, Burchinal, McAdoo and Garcia- Coll2001).
The PQ is a 30-item inventory, where the mothers reported the frequency of specific parenting behaviors (expectations of obedience, punishment, warmth, and inductive reasoning). The original scale was adapted to Turkish by Yağmurlu and Sanson (Reference Yağmurlu and Sanson2009), and it was rated on a 5-point Likert scale. The early childhood version (ages 3–5) of the HOME was adapted to Turkish for this longitudinal study (Baydar & Bekar, Reference Baydar and Bekar2007). The factor analysis of the 6 items from the PQ (e.g., “When my child seriously misbehaves, I punish him/her physically, for example I slap him/her”) and 6 items from the HOME (e.g., “The mother talked to the child in a harsh manner, yelled at him/her or insulted him/her at least once during the home visit”) identified a single factor. The percentage of total variance accounted by that factor were 37.0% and 38.8%, respectively, for ages 3 and 4. The internal reliability of the combined harsh parenting measure was α = 0.83 and 0.84 for ages 3 and 4, respectively (range 0–4).
The SES measure combined the measures of maternal education, paternal education, and a composite measure of family economic well-being (including the material possessions of the family and monthly per person expenditures of the household; Baydar et al., Reference Baydar, Küntay, Yagmurlu, Aydemir, Cankaya, Göksen and Cemalcilar2014). This measure is a factor score (M = 0.00, SD = 1.00). The data for the SES indicators came from the age 3 interviews.
Spousal harassment was based on 10 mother-report items that were developed for the current study (Baydar & Yumbul, Reference Baydar and Yumbul2004; range 0–4, α = 0.89). These items ranged from milder forms of abuse, such as verbal abuse (e.g., “Sometimes during our arguments, my husband uses insulting language towards me”), to more destructive forms, such as sexual abuse (e.g., “my spouse forces me to have sexual intercourse with him”).
Statistical methods
The aim of this paper was to understand the associations of maternal depressive symptoms with child externalizing behaviors, exploiting longitudinal data. All analyses were conducted with MPLUS version 7.31 (Muthén & Muthén, Reference Muthén and Muthén1998–2017). All participants who had data at the baseline assessment were included in the longitudinal analyses, even if they attrited from the study subsequently. Maximum likelihood estimation was used, which handled missing data under the assumption of missingness at random.
We first estimated the trajectories of maternal depressive symptoms and children's externalizing behaviors. After identifying the parametric structure of the trajectories of both processes, a bivariate transactional autoregressive latent trajectory (ALT) model was estimated. We then estimated a model exploring the indirect association of maternal depressive symptoms with child externalizing behaviors through maternal harsh parenting behaviors.
The models of the trajectories were developed in three steps. Because the home visits were not exactly 12 months apart, the trajectories could most appropriately be modeled by individually varying time points of observation. However, this approach had several disadvantages, such as being numerically difficult to estimate, not yielding standardized coefficients, and not allowing the estimates of indirect effects. In the current study, the length of the intersurvey interval varied due to scheduling of the field work, and was not endogenous to the family characteristics. Models using individually varying time points and fixed time points were compared. After confirming that the fit of these models or their estimated parameters did not differ substantially, we proceeded with the models with fixed time points.
A number of different models were estimated to determine the shapes of the maternal depressive symptom trajectories and children's externalizing behavior trajectories. These models were compared in terms of model fit and parameter estimates. Although quadratic models fit both maternal depressive symptoms and child externalizing behaviors better than the linear models, their fits were still not satisfactory. Furthermore, nonmonotonous trends were detected in ages 5–7. Both depressive symptom and externalizing behavior trajectories steadily declined at ages 3–5, but they both rose at age 6, and declined again at age 7. Piecewise linear models (latent growth models with free time scores) were used as flexible alternatives to represent nonlinear trends (Curran, Obeidat, & Losardo, Reference Curran, Obeidat and Losardo2010; Diallo & Morin, Reference Diallo and Morin2015; Muthén & Muthén, Reference Muthén and Muthén1998–2017). The models presented here had five time points representing ages 3, 4, 5, 6, and 7, where the time scores for ages 6 and 7 were freely estimated.
Our analyses also indicated that earlier measurements of both maternal depressive symptoms and children's externalizing behaviors had strong positive effects on their subsequent measurements, beyond what the classical latent trajectory model could take into account. An ALT model allowed the association of the lagged values of the observed measures with the later values, while simultaneously estimating the latent trajectories (Bollen & Curran, Reference Bollen and Curran2004). The ALT models were compared to the traditional latent trajectory models. The ALT models had significantly better fit, and therefore they were used to build the multivariate models.
We modeled both inter- and intraindividual differences in the association of maternal depressive symptoms with child externalizing behaviors, and their transactional associations with one another. A bivariate transactional ALT model accomplished the disaggregation of inter- and intraindividual differences in each trajectory, and the associations of these two components of variance in the mother and child trajectories (Berry & Willoughby, Reference Berry and Willoughby2017).
In latent trajectory models, the differences between individual trajectories were quantified with a latent “level” and a latent “change,” which, in the current study, was represented with a piecewise linear function. In the bivariate transactional ALT model, the following quantities estimated the associations of between-mother differences with between-child differences: (a) the covariance of the latent level of maternal depressive symptoms with the latent level of child externalizing behaviors; (b) the covariance of the latent change in maternal depressive symptoms with the latent change in child externalizing behaviors; and (c) the association of the latent level of each process with the latent change of the other process.
The autoregressive and cross-lagged paths represented the within-person and within-dyad associations, respectively. The autoregressive process and the cross-lagged process decomposed the intraindividual and intradyad differences into the following components: (a) continuity of the deviations of the observations for each mother and each child from their own latent trajectory (i.e., intraindividual change) and (b) the association of the deviations of one process from its latent trajectory with the subsequent deviations of the other process from its latent trajectory (intradyad change; Berry & Willoughby, Reference Berry and Willoughby2017).
Results
The original sample consisted of 1,052 children and their families, and 789 (75%) completed all five waves of the study. Of the 1,052 children and their families, 262 (25%) missed at least one wave of the study. At the final (fifth) wave of the study, the sample consisted of 792 families. We compared the sample that was lost from follow-up to the sample that was retained on the following baseline (Wave 1) characteristics: gender, age of the child, maternal age, urban versus rural background, maternal marital status, the number of children of the mother, SES, years of completed education of the mother, maternal employment status, household size, maternal depressive symptoms, child externalizing behaviors, harsh parenting of the mother, and mother reports of spousal harassment. Those families who attrited had higher SES, t (1,050) = 2.48, p = .013, than those who were retained, owing to the high geographical mobility of urban families. Similarly, the families who were lost to follow-up were more likely to be living in urban settings, χ2 (1, N = 1,052) = 12.32, p < .001, had smaller households, t (1,050) = 5.42, p < .001, and had younger focal children, t (1,050) = 2.66, p = .008, than the families who remained in the study. The mothers who were lost to follow-up had fewer children, t (1,050) = 5.84, p < .001, and more years of education, t (1,047) = 2.14, p = .033, than the mothers who remained in the study. However, the two groups did not significantly differ in terms of the child's gender, maternal age, maternal marital status, maternal employment, baseline child externalizing behaviors, combined maternal depressive symptoms, harsh parenting, and spousal harassment. Table 1 provides the characteristics of the sample at baseline. Many characteristics that indicated SES of the mothers varied widely, more so than a typical sample from the United States or Western Europe.
Table 1. Characteristics of the sample at age 3 interview

Table 2 provides the means, standard deviations, and correlations of the combined maternal depressive symptoms scores (from all 5 years), child externalizing behaviors scores (from all 5 years), and the covariates used in the analyses. Autocorrelations between maternal depressive symptoms that were observed 1 year apart were .45 on average, and ranged from .34 to .54. The autocorrelations between child externalizing behaviors observed 1 year apart were .44 on average, and ranged from .34 to .55. The cross sectional correlation of maternal depressive symptoms with child externalizing behaviors (range = .15–.38 for ages 3–7) was significantly higher at age 4 than at age 3 (z = 5.14, p < .001), and higher at age 7 than at age 6 (z = 2.31, p = .017).
Table 2. Descriptive statistics and correlations for the study variables

Note: CMDS, combined maternal depressive symptoms. CEB, child externalizing behavior. SES, socioeconomic status. *p < .01. **p < .001.
The trajectories of maternal depressive symptoms
The goodness of fit indices for the different models of depressive symptom trajectories are presented in Table 3. The linear latent growth models with individually varying time points (Model I) and fixed time points of observation (Model II) were similar, as indicated by the Akaike information criterion (AIC) and the Bayesian information criterion (BIC; Table 3). The comparison of the quadratic models with individually varying (Model III) and fixed time points (Model IV) with their linear counterparts showed that the former had slightly better fit indices than the latter. Nevertheless, the fit indices of none of these models were in the desired range, probably because of the slight increase in the mean level of the combined depressive symptom scores when the children were 6, and a sharp decline between the ages of 6 and 7.Footnote 1
Table 3. Comparison of models of intra-individual change in maternal depressive symptoms

Note: aχ2, RMSEA, and CFI are not available for models with individually varying time points. ALT, autoregressive latent trajectory.
We used a piecewise linear model (represented by a latent slope where two of the five time scores were freely estimated) to account for the nonlinearity of the trajectories of depressive symptoms. The piecewise linear model (Model V) of depressive symptoms had substantially improved fit indices compared to Models II and IV. However, the root mean square error of approximation (RMSEA) and the comparative fit index (CFI) were still not in the desirable range. The ALT model (Model VI) resulted in an acceptable fit.
The latent level and its variance in Model VI were significant (level = .64, p < .001; σ2level = .18, p < .001). The latent change was also significant; however, its variance was not (change = –.10, p < .001.; σ2change = .01, p = .198). The latent level of the model was negatively associated with the latent change (r level, change = –.69, p < .001); however, due to the small and nonsignificant variance of the change, this negative correlation should be cautiously interpreted.
The trajectories of children's externalizing behaviors
Table 4 presents the results of the analyses of the child externalizing behavior trajectories. The linear trajectory models with individually varying time points (Model I) and fixed time points of observations (Model II), and the quadratic trajectory models with individually varying (Model III) and fixed time points of observation (Model IV) did not provide satisfactory fit because the age trend of externalizing behaviors was not uniform. Specifically, externalizing behaviors declined between ages 3 and 5, increased at age 6, and decreased again at age 7.
Table 4. Comparison of models of intra-individual change in child externalizing behaviors

Note: aχ2, RMSEA, and CFI are not available for models with individually varying time points. ALT, autoregressive latent trajectory.
A possible reason for this could be the heterogeneity in the trajectories due to child characteristics such as gender, temperament, or the school start age (50.6% of the children started school at age 6). The gender of the children was not associated with the latent change of the externalizing behavior trajectory; however, a high level of externalizing behaviors at age 3 was negatively associated with the latent change (standardized β = –.41, p < .001). In addition, the transition to school was positively associated with age 6 externalizing behaviors (standardized β = .17, p < .001), and might have played a role in the nonlinearity of this trajectory. A piecewise linear model (with freely estimated time scores for ages 6 and 7; Model V) had better goodness of fit indices than the linear model (Model II), but the RMSEA and CFI were still not in the desired range. An ALT model (Model VI) yielded a good fit. We also estimated a parsimonious ALT model (Model VII) with autoregressive effects at ages 5–6 and 6–7 constrained to be equal. The fit of this latter model was not significantly different from that of Model VI, χ2change (1, n = 1,052) = 0.12, p = .751. The multivariate models presented below were built on this parsimonious ALT model. Both the latent level (1.36, p < .001) and the latent change (–0.25, p < .001) were significant, as well as their variances (σ2level = .17, p < .001; σ 2change = .01, p = .022). The latent level and change were not significantly associated (r = –.29, p = .055).
The estimated trajectories of combined maternal depressive symptoms scores and child externalizing behavior scores are presented in Figure 1. Both trajectories clearly show nonlinearity due to an increase at age 6 in the otherwise declining trajectories throughout early childhood. The most likely cause of this temporary increase is the transition to school that was experienced by slightly more than one-half of this sample at age 6.

Figure 1. The predicted trajectories of the combined maternal depressive symptoms and child externalizing behavior: the results of the autoregressive latent trajectory models.
The transactional model of maternal depressive symptoms and child externalizing behaviors
A bivariate transactional ALT model tested the associations of (a) the latent level and change of maternal depressive symptoms trajectory with the latent level and change of children's externalizing behavior trajectory and (b) the transactional associations of maternal depressive symptoms with children's externalizing behaviors at each age. The model also included child gender, family SES, and spousal harassment as covariates associated with the latent level and latent change. Figure 2 presents this model and the estimated standardized coefficients. In order to avoid an underidentification problem, the covariance of the latent change of maternal depressive symptoms with the latent change of child externalizing behaviors was set to zero. The reason for this constraint was the nonsignificant and substantially small residual variance of the latent change in child externalizing trajectories (see the results below). When the variance of a latent variable is very small, an attempt to estimate a covariance of that variable with another leads to model identification problems. The coefficients of the full transactional model are presented in Table 5. This model had a satisfactory overall goodness of fit, χ2 (38) = 104.52, p < .001; RMSEA = .04, 90% confidence interval [.03, .05]; CFI = .98. The average R 2 estimates for the observed maternal depressive symptoms and child externalizing behaviors were .47 and .44, respectively.
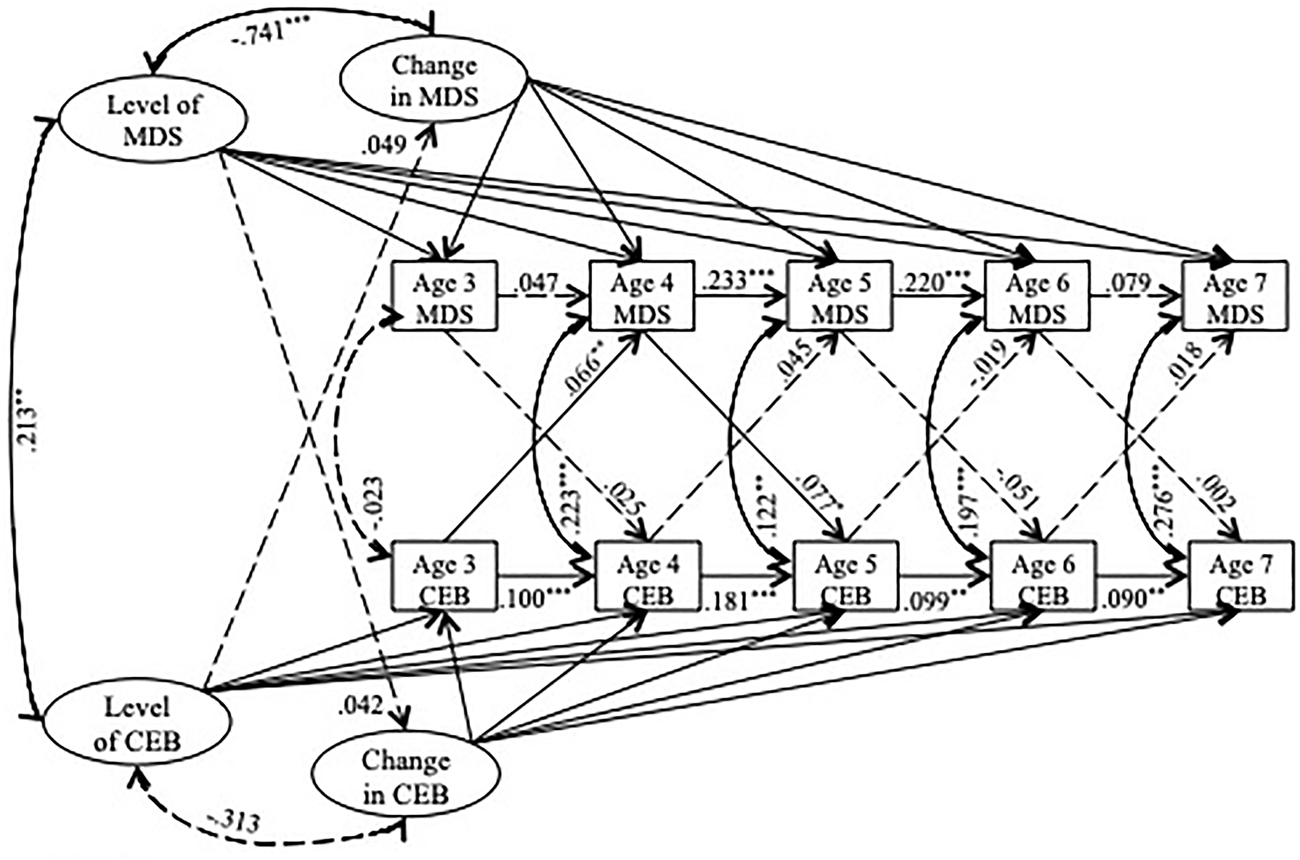
Figure 2. The transactional autoregressive latent trajectory model of combined maternal depressive symptoms and child externalizing behaviors for ages 3–7. The effects of the covariates and the covariances between the covariates are not depicted, but estimated in this model. The numbers indicate standardized coefficients. –– → indicates a nonsignificant path. — → indicates a significant path. MDS, combined maternal depressive symptoms. CEB, child externalizing behaviors. *p < .05. **p < .01. ***p < .001.
Table 5. The estimated unstandardized coefficients of the full transactional autoregressive latent trajectory model for ages 3–7

Note: All models included child gender, socioeconomic status, and harassment of the mother by the father as covariates. The standardized coefficients are provided in Figure 2. *p < .05. **p < .01. ***p < .001.
The estimates for the means of latent level and change of the combined maternal depressive symptom score trajectories were .393 and –.079, respectively, implying an overall decline. The estimates for the latent level and change of child externalizing behaviors were 1.134 and –0.226. Controlling for the covariates, the latent levels of the two processes had significant variances (.15, p < .001 and .14, p < .001 for maternal depressive symptoms and child externalizing behaviors, respectively). The residual variance in latent change in maternal depressive symptoms was significant (σ2change = .02, p = .019), but the residual variance of the latent change in child externalizing behaviors was not significant (σ2change = .01, p = .076), pointing to a better prediction of the variability of child externalizing trajectories than maternal depressive symptom trajectories.
The latent level of the combined maternal depressive symptoms was not significantly associated with the latent decline in child externalizing behaviors (standardized β = .04, p = .857). Similarly, the latent level of externalizing behaviors was not significantly associated with the latent decline in maternal depressive symptoms (standardized β = .05, p = .664). The level and change of maternal depressive symptoms were significantly negatively correlated (r = –.74, p < .001). The level and the change of child externalizing behaviors were not significantly correlated (r = –.31, p = .068).
There were no significant cross-lagged (transactional) associations of prior maternal depressive symptoms with subsequent child externalizing behaviors at ages 3–4 (standardized β = .03, p = .390), at ages 5–6 (standardized β = –.05, p = .128), and at ages 6–7 (standardized β = .002, p = .950). There was a small but significant association of age 4 maternal depressive symptoms with age 5 child externalizing behaviors (standardized β = .08, p = .033). Similarly, there were no significant cross-lagged associations of prior child externalizing behaviors with subsequent maternal depressive symptoms at ages 4–5 (standardized β = .05, p = .159), at ages 5–6 (standardized β = –.02, p = .500), and at ages 6–7 (standardized β = .02, p = .624). Age 3 externalizing behaviors was significantly, but weakly associated with age 4 maternal depressive symptoms (standardized β = .07, p = .002). In sum, the transactional associations of the deviations from the underlying trajectories of maternal depressive symptoms with child externalizing behaviors that were evident in these data were small and limited to ages 3–5.
When the latent trajectories were accounted for, the autoregressive associations of the combined maternal depressive symptoms at ages 3–4 (standardized β = .05, p = .224), and ages 6–7 (standardized β = .08, p = .133) were nonsignificant. The autoregressive associations of depressive symptoms for ages 4–5 (standardized β = .23, p < .001) and 5–6 (standardized β = .22, p < .001) were significant. Similarly, after accounting for the latent trajectories, the autoregressive associations of child externalizing behaviors at all ages were significant (standardized β = .10, .18, .10, and .09, all p < .01, for ages 3–4, 4–5, 5–6, and 6–7, respectively). These findings suggested a stronger continuity of the deviations from the underlying trajectory of child externalizing behaviors than the combined maternal depressive symptoms.
As expected, boys had higher initial levels (standardized β = .21, p < .001) and a steeper decline of externalizing behaviors than girls over the study period (standardized β = –.23, p = .023). Family SES was significantly negatively associated with the latent level of the combined maternal depressive symptoms (standardized β = –.16, p < .001), but not with the latent change (standardized β = –.03, p = .587). Family SES was also not significantly associated with the latent level of child externalizing behaviors (standardized β = –.01, p = .744), but it was significantly associated with the change (standardized β = –.26, p = .027). A high level of spousal harassment when the child was 3 years old was associated with a high latent level of combined maternal depressive symptoms (standardized β = .58, p < .001), a high latent level of child externalizing behaviors (standardized β = .36, p < .001), and a steeper decline of the maternal depressive symptoms (standardized β = –.60, p < .001). It was not associated with the latent change in child externalizing behaviors (standardized β = –.19, p = .222).
The mediating role of harsh parenting behaviors in mother-to-child associations
The model described above identified transactional associations only for ages 3–5. We therefore estimated a model focusing on this period, which included age 3 and age 4 harsh parenting as mediators of the mother-to-child and child-to-mother associations. As before, child gender, family SES, and spousal harassment were the covariates of the latent level and latent change constructs. Figure 3 presents this model and its estimated standardized coefficients. This model was identical to the full model (as depicted in Figure 2) in its structure of the concurrent and lagged associations of maternal depressive symptoms and child externalizing behaviors. Table 6 presents the estimated unstandardized coefficients and their standard errors. The residual variances of the latent change of maternal depressive symptoms and the latent change of child externalizing behaviors were constrained to zero for identifiability. This constraint was needed, because only three time points of observation were used in this ALT model, and a substantial proportion of the variance of the latent change was accounted for by the autoregressive components between consecutive observations. This model had a satisfactory overall goodness of fit, χ2 (15) = 53.59, p = .000; RMSEA = .05, 90% confidence interval [.04, .06]; CFI = .98.

Figure 3. The autoregressive latent trajectory model of combined maternal depressive symptoms and child externalizing behaviors for ages 3–5 that included the mediating role of harsh parenting. The effects of the covariates and the covariances between the covariates are not depicted, but estimated in this model. The numbers indicate standardized coefficients. – – → indicates a nonsignificant path. — → indicates a significant path. MDS, combined maternal depressive symptoms. CEB, child externalizing behaviors. HP, harsh parenting. *p < .05. **p < .01. ***p < .001.
Table 6. The estimated unstandardized coefficients of the autoregressive latent trajectory model for ages 3–5, including the mediated effects through harsh parenting

Note: All models included child gender, socioeconomic status, and harassment of the mother by the father as covariates. Only the transactional paths between maternal depressive symptoms and child externalizing that were statistically significant in the full model (Table 5) were included in this model. The standardized coefficients are provided in Figure 3. *p < .05. **p < .001.
We present the results for mother-to-child paths first, and the child-to-mother paths next. Consistent with the full transactional model, the direct and indirect (through harsh parenting) lagged association of age 3 combined maternal depressive symptoms with age 4 child externalizing behaviors was nonsignificant (standardized direct β = .02, p = .565; standardized total indirect β = .00, p = .918). The direct lagged association of age 4 combined maternal depressive symptoms with age 5 child externalizing behaviors (standardized β = .09, p = .025) was significant. The indirect path through harsh parenting, however, was nonsignificant (standardized total indirect β = .00, p = .240) because of the nonsignificant association of age 4 harsh parenting with age 5 child externalizing behaviors (standardized β = .05, p = .176).
The direct child-to-mother associations of externalizing behaviors with combined maternal depressive symptoms were nonsignificant for both ages 3–4 and 4–5 in this model (standardized β = .02, p = .572; and standardized β = .03, p = .383, respectively). There was also no support for the indirect child-to-mother association for ages 3–4, through harsh parenting (standardized total indirect β = .01, p = .213). Nevertheless, the association of age 3 child externalizing behaviors with age 3 harsh parenting was significant (standardized β = .19, p < .001). The total indirect child-to-mother association was significant for ages 4–5. The association of age 4 child externalizing behaviors with age 4 harsh parenting (standardized β = .32, p < .001), and the association of age 4 harsh parenting with age 5 combined maternal depressive symptoms (standardized β = .08, p = .024) were both significant. Consequently, the total indirect child-to-mother association through harsh parenting was small but significant (standardized total indirect β = .03, p = .027). Nevertheless, because of the very small and nonsignificant direct child-to-mother path for ages 4–5, the total effect was nonsignificant (standardized total β = .06, p = .129).
Discussion
In this study, we examined the transactional associations of maternal depressive symptoms with children's externalizing behaviors, at two different levels of inference: the association of the interindividual differences in these processes, and the associations of the intraindividual changes in the two processes. In addition, we investigated the role of harsh parenting as a mediator in the transactional associations.
Our data came from a nationally representative sample of mothers and children in Turkey. The interpretation of the quantitative findings of this study must consider its social and cultural context, characterized by socioeconomic disadvantage, collectivism, and hierarchy based on social class, gender, and age. A concern may pertain to the reporting of depressive symptoms in this cultural context. In this study, we combined depressive, anxiety, and somatization symptoms in order to accommodate the cultural preferences in the reporting of psychological symptoms. There appears to be little reason to suspect the underreporting of these symptoms in this sample, based on the comparisons with previous community samples. It was recommended that a T score of 63 or above in the total psychological distress measure, based on the mean and standard deviation of a relevant population, could be taken as an indicator of an elevated or potentially clinical level of symptoms (Derogatis, Reference Derogatis1993). The current sample was a nationally representative community sample, allowing us to use its estimates as a relevant norm. We estimated that 12.0% of the mothers had elevated levels of symptoms. When norm estimates from the nonclinical sample of the original psychometric study of the BSI were used (Derogatis & Melisaratos, Reference Derogatis and Melisaratos1983), this proportion was estimated to be 21.6%. However, it should be noted that the mean scores of the nonclinical sample in the original psychometric study were substantially lower than those reported by subsequent studies from the United States and Western Europe (e.g., Gasperi, Herbert, Schur, Buchwald, & Afari, Reference Gasperi, Herbert, Schur, Buchwald and Afari2017; Rytilä-Manninen et al., Reference Rytilä-Manninen, Fröjd, Haravuori, Lindberg, Marttunen, Kettunen and Therman2016). The latter estimate of 21.6%, therefore, is likely to be too high.
Similar to other longitudinal studies, we found that most children's externalizing behaviors steadily declined (Baydar & Akcinar, Reference Baydar and Akcinar2017; Gilliom & Shaw, Reference Gilliom and Shaw2004), with a slight increase as they first started school. Nevertheless, there was a substantial heterogeneity of the trajectories of externalizing behaviors in early childhood. Based on Colvin (Reference Colvin1999)’s clinical cutoff scores, 11.7% of the 7-year-old children in this sample were in the clinical range (Baydar & Akcinar, Reference Baydar and Akcinar2017). Maternal depressive symptoms also slightly declined during the early childhood of the focal children, similar to the patterns reported by the previous studies using data from a socioeconomically disadvantaged sample (Choe et al., Reference Choe, Shaw, Brennan, Dishion and Wilson2014; Hails et al., Reference Hails, Reuben, Shaw, Dishion and Wilson2017; Shaw et al., Reference Shaw, Sitnick, Reuben, Dishion and Wilson2016).
One of the contributions of this study was its approach to the modeling of trajectories. The trajectories of both maternal depressive symptoms and child externalizing behaviors were represented by ALT models that disaggregated the inter- and intraindividual sources of variance. An ALT model may be a good choice when a strong developmental trend is present. In the absence of explicit modeling of that developmental trend, the autoregressive models may require second- and third-order lagged associations (see, e.g., Choe et al., Reference Choe, Shaw, Brennan, Dishion and Wilson2014). In the current study, the ALT models were augmented with cross-lagged associations between maternal depressive symptoms and child externalizing behaviors. The resulting models identified the following six components underlying the observed depressive symptom and externalizing behavior trajectories: (a) interindividual differences in the latent level of and change in maternal depressive symptoms; (b) interindividual differences in the latent level of and change in child externalizing behaviors; (c) the association of the interindividual differences in the maternal trajectories (i.e., level and change) with the child trajectories; (d) the intraindividual association of the deviations from the latent maternal depressive symptom trajectories over time; (e) the intraindividual association of the deviations from the latent child externalizing trajectories over time; and (f) the bidirectional intradyad associations of the deviations of depressive symptoms and externalizing behaviors from their own underlying trajectories.
In this decomposition, the transactional associations of maternal symptoms with child externalizing behaviors were represented by the components (c) and (f). The former was an association that was not dynamic (did not change over early childhood). The latter was an association that could change over time. These two types of transactions had vastly different policy implications. The unique contribution of this study to the extant literature was its ability to identify these two types of transactions quantitatively. Previous studies that addressed the transactional associations between maternal depressive symptoms and child behaviors (Choe et al., Reference Choe, Shaw, Brennan, Dishion and Wilson2014; Hails et al., Reference Hails, Reuben, Shaw, Dishion and Wilson2017; Shaw et al., Reference Shaw, Sitnick, Reuben, Dishion and Wilson2016) adopted conventional transactional models that confounded the association of the interindividual differences in trajectories with the associations of the intraindividual changes in the mother and the child (Berry & Willoughby, Reference Berry and Willoughby2017).
We expected to find relatively strong transactional associations of combined maternal depressive symptoms with child externalizing behaviors in this sample for three reasons. First, owing to the low rates of maternal employment and low rates of preschool attendance, the mothers and their children spent most of their time together at home during the years prior to elementary school, providing ample opportunity to interact. Second, we expected the motherhood role to be salient, because of the lack of roles of the mothers outside the home, suggesting the potential for strong child-to-mother effects. Third, fathers were rarely involved in parenting in the current social context (Mother Child Education Foundation, 2017), rendering the children vulnerable to the negative effects of maladaptive parenting that could stem from maternal depressive symptoms. Previous research indicated that the presence of an involved father could be a protective factor against the maladaptive cycle of escalating maternal depressive symptoms and child externalizing behaviors (Vakrat, Apter-Levy, & Feldman, Reference Vakrat, Apter-Levy and Feldman2018). In the absence of father involvement, parenting stress of the mothers was probably high. In addition to the expectations based on these conceptual arguments, the cross-sectional correlations between maternal depressive symptoms and child externalizing behaviors got stronger over the study period, in a manner that was consistent with the presence of transactional associations.
There was a positive and moderately strong association of the level of combined maternal depressive symptoms with the level of child externalizing behaviors at age 3. The baseline levels of the two trajectories, however, were not associated with the latent change in the other trajectory, failing to support the hypothesis of a transactional association. How high or low a mother's depressive symptoms were when her child was 3 years old was not associated with how fast or slow the child's externalizing behaviors declined over the next 4 years, and vice versa. Furthermore, the cross-lagged within-dyad associations suggested statistically significant but substantially small transactions that were limited to ages 3–5. In other words, an increase from a mother's own typical depressive symptom levels was not substantially associated with a subsequent increase in her child's own typical externalizing behaviors. Neither was an increase in children's externalizing behaviors substantially predictive of increases in their mothers’ depressive symptoms. Because the transactional associations in our model were small, the mediated association of age 4 maternal depressive symptoms with age 5 child externalizing behaviors through harsh parenting practices was significant, but also small.
The small and nonsignificant transactional associations of maternal depressive symptoms with child externalizing behaviors after age 5 raise the question of whether the start of school might have disrupted the association of the two processes. Our data indicated that only 8.8% of the children had started attending school at the age 5 interview. This percentage was still only at 50.6% at the age 6 interview. By age 7, nearly all children were attending school (99.1%). In order to test whether the absence of transactional associations between maternal depressive symptoms and child externalizing behaviors at age 6 is due to school entry, we reestimated a transactional model for the children who did not attend school at age 6. That model also found no significant transactional associations between the two processes after age 5.
Our findings can be compared to three previous studies, all of which used data from the same longitudinal study of low-SES mothers and children, who were selected for high levels of maternal psychopathology, family problems, and/or child behavior problems. Choe et al. (Reference Choe, Shaw, Brennan, Dishion and Wilson2014) and Hails et al. (Reference Hails, Reuben, Shaw, Dishion and Wilson2017) found reciprocal associations of maternal depressive symptoms with child oppositional behaviors between ages 2 and 3, a child-to-mother association between ages 3 and 4, and a mother-to-child association between ages 4 and 5. Similarly, Shaw et al. (Reference Shaw, Sitnick, Reuben, Dishion and Wilson2016), using the same data, found small but consistent bidirectional associations between ages 2 and 5, and a small child-to-mother association between ages 5 and 7.5. Using externalizing data from a different sample of boys that extended from toddler years to adolescence, Shaw et al. (Reference Shaw, Sitnick, Reuben, Dishion and Wilson2016) found small mother-to-child and child-to mother associations limited to early childhood.
The findings of these three studies were surprisingly consistent with the current study, in that the estimated transactional associations were small, despite different structures of the models, different sets of covariates, and different mediators that were included in the models. However, none of these previous studies attempted to identify the different sources of associations in dyadic longitudinal data. As such, they are expected to have overestimated the transactional associations of maternal depressive symptoms with child behaviors.Footnote 2
Despite the lack of evidence for strong transactional associations in this sample, the children whose mothers had a high level of combined depressive, anxiety, and somatic symptoms at age 3 tended to have a high level of externalizing behaviors at that age. Two reasons could account for this finding. The first is the possible presence of stronger transactional associations between the two processes prior to age 3 than after that age. The significant transactional associations identified in the toddler years by previous studies supported this hypothesis (Choe et al., Reference Choe, Shaw, Brennan, Dishion and Wilson2014; Hails et al., Reference Hails, Reuben, Shaw, Dishion and Wilson2017; Shaw et al., Reference Shaw, Sitnick, Reuben, Dishion and Wilson2016). The negative repercussions of maternal depressive symptoms for parenting behaviors could lead to insecure attachment during the first few years of life (Campbell et al., Reference Campbell, Brownell, Hungerford, Spieker, Mohan and Blessing2004; Cicchetti, Rogosch, & Toth, Reference Cicchetti, Rogosch and Toth1998). By age 3, the patterns of mother–child interactions may increasingly solidify, and may be robust against temporary changes in the behavior of the mother or the child. An inertia in the patterns of interactions during childhood is predicted by the attachment theory (Bowlby, Reference Bowlby1969) and the systems theory of coercive interactions (Granic & Patterson, Reference Granic and Patterson2006).
Another reason for the lack of strong transactions between the two processes may be the presence of a relatively unchanging common confounding factor (e.g., genetic effects, biological risk factors, stress in the household, or socioeconomic deprivation). In this sample, we considered negative mother–father relationships as a potential confounding factor. There was a strong association of spousal harassment with both maternal depressive symptoms and child externalizing behaviors. The experience of interpersonal conflicts, especially with a family member, may lead to depressive symptoms in women (Artazcoz, Benach, Borrell, & Cortes, Reference Artazcoz, Benach, Borrell and Cortes2004; Kalmijn & Monden, Reference Kalmijn and Monden2006). Interparental conflict is also a risk factor for externalizing behaviors in children (Cummings et al., Reference Cummings, Goeke-Morey and Papp2004; Kouros et al., Reference Kouros, Cummings and Davies2010).
The results of this study have important policy implications, regarding the timing of the interventions aiming to prevent the negative repercussions of maternal depressive symptoms on children's behavioral development. Our results show that when the children are 3 years old, the depressive symptoms of their mothers are strongly associated with their externalizing behaviors. The lack of substantial associations between the subsequent changes in the two processes suggests that the interventions that aim to prevent externalizing behaviors through a reduction in maternal depressive symptoms may be more effective prior to age 3 because maladaptive patterns of interaction may solidify after this age (Shaw, Connell, Dishion, Wilson, & Gardner, Reference Shaw, Connell, Dishion, Wilson and Gardner2009). Nevertheless, in an evaluation of 24 parental interventions, Thomas and Zimmer-Gembeck (Reference Thomas and Zimmer-Gembeck2007) found that most of these interventions not only improved parenting behaviors but also reduced children's behavior problems, even after age 3. However, other research found that when interventions only targeted maternal depressive symptoms, the negative parenting behaviors that were strongly linked to externalizing behaviors did not change (Forman et al., Reference Forman, O'Hara, Stuart, Gorman, Larsen and Coy2007; Foster et al., Reference Foster, Webster, Weissman, Pilowsky, Wickramaratne, Talati and King2008; Nylen, Moran, Franklin, & O'Hara, Reference Nylen, Moran, Franklin and O'hara2006). In their review, Gunlicks and Weissman (Reference Gunlicks and Weissman2008) stated that even though an alleviation of maternal depressive symptoms was associated with some improvements in children's emotional well-being, it did not improve their attachment patterns or behaviors. Considering this body of evidence, further research on the transactional associations of maternal depressive symptoms with child behavioral development during infancy and early toddlerhood may be fruitful, focusing on the mediating role of the attachment processes.
There are some limitations of the current study. First, our study focused on the psychopathology of the mothers, and did not consider the fathers. Our findings on the substantial association of spousal harassment with both maternal symptoms and child externalizing behaviors highlighted the potential importance of the mental and behavioral health of the fathers for the mother–child processes.
Second, apart from the observer-reported harsh parenting, all other data were reported by the mothers. However, mothers who experience depressive symptoms tend to overreport their children's behavior problems (Boyle, & Pickles, Reference Boyle and Pickles1997; Goodman et al., Reference Goodman, Rouse, Connell, Broth, Hall and Heyward2011). Hails et al. (Reference Hails, Reuben, Shaw, Dishion and Wilson2017) had access to reports from a secondary caregiver in addition to the maternal reports on externalizing behaviors, and they found that the estimated transactional association of maternal depressive symptoms with child externalizing behaviors was weaker with those reports than with maternal reports. The implication is that even the meager transactional associations found in the current study may be inflated, and that they may partly be attributed to common method variance.
The current study investigated the longitudinal transactional associations of interindividual differences and intraindividual changes in maternal depressive symptoms and child externalizing behaviors, exploiting the availability of a large, nationally representative, longitudinal study. Rather modest transactional associations were identified, only between ages 3 and 5. The absence of strong and consistent transactional associations between ages 3 and 7 calls for further research on the source of their strong cross-sectional associations during this developmental period.
Author ORCIDs
Begum Dora, 0000-0001-5498-6096
Financial support
This research was funded by Grants 106 K347 and 109 K525 from the Turkish Institute for Scientific and Technological Research and generous support from Koc University.











