Over a million refugees have arrived by sea in Greece during the last four years, almost half of whom are under 18 years of age (UNHCR, 2018). These children and adolescents report prolonged exposure to violence and lack of a sense of security (Giannakopoulos & Anagnostopoulos, Reference Giannakopoulos and Anagnostopoulos2016; Sleijpen, Mooren, Kleber, & Boeije, Reference Sleijpen, Mooren, Kleber and Boeije2017). Upon arrival in Greece, many are placed in camps with limited access to school and mental health services, and high rates of attempted suicide, panic attacks, anxiety, and aggressive outbursts have been reported (Hermans et al., Reference Hermans, Kooistra, Cannegieter, Rosendaal, Mook-Kanamori and Nemeth2017; Kousiakis, James, & Benasuly, Reference Kousiakis, James and Benasuly2016; Médecins Sans Frontières, 2018). There is an urgent need for scalable interventions that are designed to improve the mental and physical health of these refugee children and adolescents, given research that highlights the importance of targeting protective factors (Fazel & Betancourt, Reference Fazel and Betancourt2018) and resilience-building (Reed, Fazel, Jones, Panter-Brick, & Stein, Reference Reed, Fazel, Jones, Panter-Brick and Stein2012; Werner, Reference Werner2012) in shaping the mental health of child refugees.
Most interventions for refugee children focus on ameliorating negative outcomes that are related to trauma exposure and insecurity, rather than on improving well-being, resilience, or the ability to cope with ongoing challenges (Fazel, Reference Fazel2018; Miller-Graff & Cummings, Reference Miller-Graff and Cummings2017; Tyrer & Fazel, Reference Tyrer and Fazel2014). Randomized controlled trials with child refugees have provided evidence that group-based interventions that target depression, anxiety, and posttraumatic stress disorder may act as potential first-line treatments for improving children's mental health (Fazel & Betancourt, Reference Fazel and Betancourt2018; Hodes & Vostanis, Reference Hodes and Vostanis2018; Newnham, Kashyap, Tearne, & Fazel, Reference Newnham, Kashyap, Tearne, Fazel, Morina and Nickerson2018; Panter-Brick, Dajani, et al., Reference Panter-Brick, Dajani, Eggerman, Hermosilla, Sancilio and Ager2018). However, there is much less evidence about the efficacy of interventions that are intended to promote positive mental health, such as well-being, optimism, and self-esteem. For example, in Tyrer and Fazel's (Reference Tyrer and Fazel2014) review of 21 school- and community-based psychological interventions for refugee children, only one included a positive outcome (well-being; Ager et al., Reference Ager, Akesson, Stark, Flouri, Okot, McCollister and Boothby2011), with all of the others testing for reductions in negative outcomes such as depression, anxiety, posttraumatic stress disorder, and functional impairment. Recently, there has been a greater focus on promoting resilience and positive functioning rather than ameliorating negative functioning (e.g., Masten, Reference Masten2014; Motti-Stefanidi, Asendorpf, & Masten, Reference Motti-Stefanidi, Asendorpf and Masten2012; Panter-Brick, Hadfield, et al., Reference Panter-Brick, Hadfield, Dajani, Eggerman, Ager and Ungar2018; Sleijpen, Mooren, Kleber, & Boeije, Reference Sleijpen, Mooren, Kleber and Boeije2017), but the majority of interventions with refugee children continue to focus on alleviating mental health symptoms—posttraumatic stress disorder in particular (Fazel, Reference Fazel2018). Given the challenges that refugee children continue to face during and after displacement and the importance of individual strengths in buffering against the development of mental health problems, a greater focus on promoting psychological resilience and positive functioning is warranted (Motti-Stefanidi, Reference Motti-Stefanidi2015; Sleijpen et al., Reference Sleijpen, Mooren, Kleber and Boeije2017; Yaylaci, Reference Yaylaci2018).
Sin and Lyubomirsky's (Reference Sin and Lyubomirsky2009) meta-analysis suggests that positive psychology interventions can be effective for both enhancing well-being and ameliorating depressive symptoms. Positive psychology interventions that focus on mindfulness (Zenner, Herrnleben-Kurz, & Walach, Reference Zenner, Herrnleben-Kurz and Walach2014), character strengths (e.g., Quinlan, Swain, Cameron, & Vella-Brodrick, Reference Quinlan, Swain, Cameron and Vella-Brodrick2015), hope (e.g., Marques, Lopez, & Pais-Ribeiro, Reference Marques, Lopez and Pais-Ribeiro2011), and psychological resilience (e.g., Pluess, Boniwell, Hefferon, & Tunariu, Reference Pluess, Boniwell, Hefferon and Tunariu2017) have been found to be effective at promoting positive development in children in high-income countries. There is emerging evidence of the success of this approach in high-risk and/or low-income populations as well. For example, a 16-session school-based program that combined stress reduction, perspective-taking, empathy training, mindfulness, and compassion-cultivating practices (Berger, Reference Berger, Mitchel and Karr2014) led to increased prosocial behaviour and academic achievements and reduced anxiety and hyperactivity among Tanzanian children and adolescents (Berger, Benatov, Cuadros, VanNattan, & Gelkopf, Reference Berger, Benatov, Cuadros, VanNattan and Gelkopf2018).
However, there is a need to design positive interventions that integrate the specific profile of children still in transit to target the processes that may be especially affected by displacement and refugee status. Many refugee children will spend a significant amount of time during their displacement living in refugee camps (Tyler & Fazel, Reference Tyrer and Fazel2014). These children have not only experienced considerable trauma but also continue to experience significant challenges such as poverty, malnutrition, limited access to education, insecurity, further violence, abuse, and poor health (Crisp, Reference Crisp2000; Silove, Ventevogel, & Rees, Reference Silove, Ventevogel and Rees2017) as well as increased psychological disturbance (Charlson et al., Reference Charlson, van Ommeren, Flaxman, Cornett, Whiteford and Saxena2019; Reed et al., Reference Reed, Fazel, Jones, Panter-Brick and Stein2012). Importantly, the waiting period before receiving refugee status can also exacerbate stress and uncertainty (Hodes & Vostanis, Reference Hodes and Vostanis2018; Sleijpen et al., Reference Sleijpen, Mooren, Kleber and Boeije2017). There are few evidence-based interventions that have been rigorously evaluated for delivery to children or adolescents in transit, and even fewer that measure or target improvements in positive outcomes (Tyrer & Fazel, Reference Tyrer and Fazel2014). Given the challenges that they will continue to face during displacement and resettlement, promoting the ability to do well despite adversity is particularly critical for these children and adolescents (Miller & Rasmussen, Reference Miller and Rasmussen2017; Silove et al., Reference Silove, Ventevogel and Rees2017).
In response to this need, the Strengths for the Journey (SFJ) intervention was developed for a forcibly displaced, late childhood and early adolescent population (Tables 1 and 2). The program was designed specifically for children who are still in transit to address the ongoing challenges that they face in Lesvos, where 80% of refugees live in temporary accommodations in nongovernment organizations (NGOs) or government-run refugee camps while they await relocation to mainland Europe (UNICEF, 2018).
Table 1. The Strengths for the Journey program

Table 2. Content of Strengths for the Journey intervention sessions
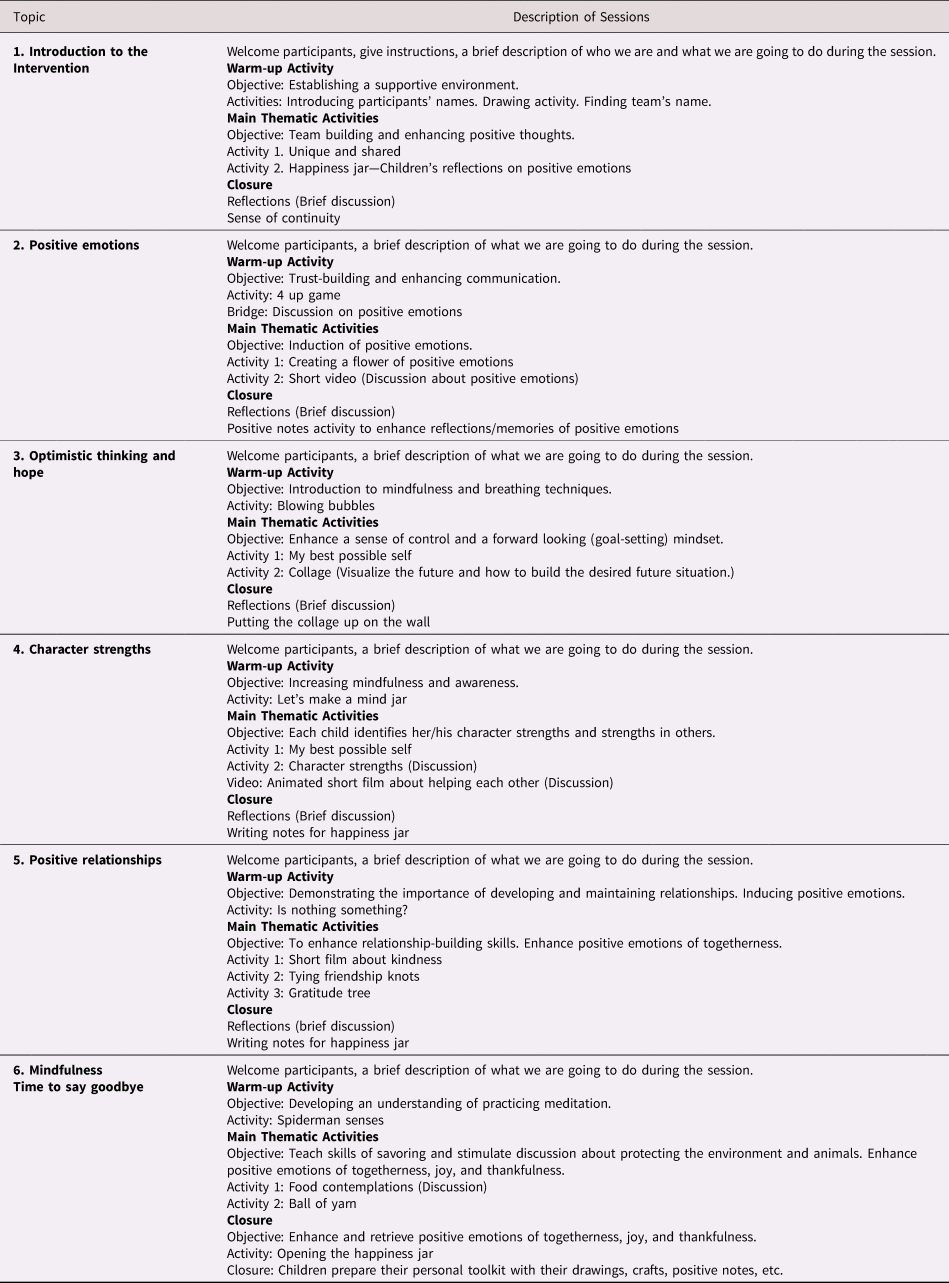
Note: The topics and activities are presented in the order in which they were delivered. In Pikpa only, topics 5 and 6 were covered on the same day.
Strengths for the Journey is a brief, group-based preventive intervention that can be delivered with limited resources by trained nonspecialists and fieldworkers in refugee camps or other humanitarian settings. It was developed for use with child and adolescent refugees in camps in Lesvos over a period of two years by working directly with refugee youth, discussing the needs and characteristics of the children in the camp with service providers and camp managers, and completing an unpublished prepilot test of the intervention with a sample of six children in summer 2015 in collaboration with the NGO, Agkalia. The goal of SFJ is to improve resilience and well-being by cultivating psychological resources, such as optimistic thinking and fostering a sense of togetherness and belonging, to enhance the experience and recall of positive emotions and facilitate future planning, identifying the child's and group's character strengths and increasing self-esteem and mindfulness (Foka & Sergianni, Reference Foka and Sergianni2019). We collaborated with authorities from three refugee camps in Lesvos—two NGOs (Agkalia and Pikpa Solidarity Lesvos) and the Municipality of Lesvos—to implement and conduct a pilot evaluation of SFJ with refugee children and adolescents.
The purpose of our pilot study was to determine whether the SFJ intervention improves positive psychological resources such as well-being, hope and optimistic thinking, and self-esteem and reduces depressive symptoms in child and adolescent refugees that are living in camps in Lesvos. We adopted a quasi-randomized wait-listed trial design over two points (before and immediately after the intervention) to assess the short-term outcomes of the SFJ intervention. This was followed by focus group interviews with the intervention participants to understand their experiences of the intervention, which psychological resources they found to be the most beneficial, and how they felt that it affected them. We hypothesized that the effectiveness of the intervention would be evidenced through improvements in well-being, optimistic thinking, and self-esteem and reductions in depressive symptoms, as indexed both by the participants’ survey responses and the focus group interviews.
Method
Participants
A total of 72 children that were living in three refugee camps in Lesvos (Kara Tepe n = 54, Caritas n = 11, and Pikpa n = 7) took part in this intervention study either in August or November 2017 (see Table 3 for sample characteristics, Supplemental Table 1 for demographics by study site, and Supplemental Figure 1 for the study timeline). The children were a nonclinical sample who ranged in age from 7 to 14 years (M = 10.76, SD = 1.96; 64.8% female). Forty-one were displaced from Syria, 13 were from Iraq, 13 were from Afghanistan, 1 was from Lebanon, and 1 identified as being from Kurdistan. One participant identified as stateless, and two did not indicate their country of origin. All of the children were living with at least one close relative in the camp.
Table 3. Sample characteristics before and after the intervention or wait-list experience

Note: All of the values are means with standard deviations in parentheses, unless otherwise specified.
The focus groups were held with 31 of the participants from Kara Tepe either immediately following the intervention or three months after their participation in the intervention (M = 11.32 years old, SD = 1.72; 67.74% female). Fourteen of the focus group participants were displaced from Afghanistan, 12 from Syria, and 5 from Iraq. The subgroup of survey participants who took part in the focus groups was comparable to the larger group with respect to their age and gender, but relatively fewer of the focus group participants were from Syria.
The three camps from which we sampled participants are similar in their living conditions. They all provide basic services, such as school, health services, legal assistance, and language classes as well as accommodation for families and vulnerable adults. However, there are a few pertinent differences between Pikpa, Kara Tepe, and Caritas. First, Kara Tepe is much larger than Caritas or Pikpa, with approximately 1,250 refugees living in Kara Tepe and just 100–150 in the other two camps. Second, Caritas is a disused hotel complex, so all of the families had bathroom facilities in their rooms, whereas in Pikpa the refugees lived in wooden houses and in Kara Tepe they lived in containers. Finally, in Kara Tepe, ready-made meals are distributed to the residents, whereas in Pikpa and Caritas, residents are given a small allowance to buy their own food.
Procedure
We applied a quasi-randomised, wait-listed design to evaluate the SFJ program with children who were living in three camps in Lesvos between July and November 2017. All children aged 7–14 who had not been identified by the camp administrator as having a mental health disorder or intellectual disability were eligible to participate. In Pikpa and Caritas, all of the children who met the inclusion criteria were invited to take part in this research. Due to the larger numbers in Kara Tepe, only children who spoke Arabic or Farsi were offered the intervention. All of the children who were asked whether they would like to participate in the intervention said that they wanted to and ultimately took part.
Participating children were allocated to either the SFJ intervention—which consisted of daily 2-hr group sessions across six days with a trained, female facilitator and a local refugee interpreter—or a wait-list control condition (details of the intervention can be found in Tables 1 and 2). There were 33 participants in the treatment group and 39 in the wait-listed group. Given that there were two predominant languages of origin in the camps and the age range of the children, the participants were grouped based on language and age into mixed-gender groups varying in size from 6 to 17 participants, resulting in six groups of Arabic-speaking children and two groups of Farsi-speaking children. Children in the treatment group (n = 33, 7 in Pikpa, 20 in Kara Tepe, and 6 in Caritas) immediately took part in the 6-day intervention, whereas those in the wait-list group (n = 39, 34 in Kara Tepe, and 5 in Caritas) were offered the chance to participate in sports activities during the same period before taking part in the intervention. Control participants that were not interested in taking part in the physical activities were offered the chance to take part in group discussions about activities that they enjoy doing at home instead (e.g., drawing, painting, sewing their own clothing) or in school (e.g., learning a foreign language, art-based activities), or shared in story telling with the facilitator. These activities were run for the control groups concurrently with the intervention for the treatment group, after which the control group was offered the chance to take part in the intervention. Which groups were allocated to the different conditions was determined by the first author based on the availability of space, translators, and facilitators in each camp. One Arabic-speaking group in Pikpa and three Arabic-speaking groups in Kara Tepe were assigned to the treatment condition, whereas two Farsi-speaking and one Arabic-speaking group in Kara Tepe and one Arabic-speaking group in Caritas were assigned to the wait-list condition.
The surveys were completed individually with the help of a facilitator and local translator through interviews in private spaces. Translators read questions aloud to the children, in Arabic or Farsi, and the facilitator noted their responses. No facilitator delivered questionnaires to children from their own intervention group. For the treatment group, data were collected immediately before (T1) and immediately after the intervention (T2) and for the wait-listed group prior to the start of their wait-list session (T1) and at the end of it (T2).
We then asked the participants whether they would be willing to take part in a focus group session. Two of the focus groups were conducted immediately following the intervention (n =13 children) and the other two were conducted three months after completion of the program (n = 18 children; Supplemental Figure 1). The focus group participants were an average of 11.32 years old (SD = 1.72), and 67.7% were female, 45.2% were displaced from Afghanistan, 38.7% were displaced from Syria, and 16.1% were displaced from Iraq. We conducted the different focus groups either immediately after or three months after the intervention to capture both immediate and longer-term views on the effects of the intervention. This allowed us to understand what components of the intervention were useful and what should be changed to improve the intervention for both short-term and long-term effects. All four focus groups were held in November 2017 in Kara Tepe. The 13 children who took part immediately after the intervention were those in the final two intervention groups, which were held in November (Supplemental Figure 1). Because Greece transfers refugees to the mainland after processing on the islands, there were only 18 participants from Kara Tepe who had taken part in the intervention in August who were still living in the camps at the time when the focus groups were conducted in November. As a consequence, we had different children take part in the immediate and longer-term focus groups. All of the children who were asked to take part in focus groups agreed to do so.
Ethical Considerations
The research received ethical approval from the Queen Mary University of London research ethics board (QMERC2017); Lesvos Municipality; and from the management at Kara Tepe, Archipelagos-Caritas, and Pikpa Lesvos Solidarity. Access was approved from The NGO Coordination Committee Support Office for Lesvos Island (General Secretariat for the Aegean and Island Policy—Greek Ministry of Maritime Affairs). Signed parental or guardian consent was obtained prior to data collection. Participating children received no remuneration, but they were allowed to keep the intervention materials that they created and a small booklet for writing.
Measures
All of the measures were translated into Arabic and Farsi with the help of a back-translation protocol. All of the measures were developed for or have been used effectively with similarly aged children and adolescents in other studies (Allgaier et al., Reference Allgaier, Pietsch, Frühe, Prast, Sigl-Glöckner and Schulte-Körne2012; Harris, Donnellan, & Trzesniewski, Reference Harris, Donnellan and Trzesniewski2018; Moghames, McEwen, & Pluess, Reference Moghames, McEwen and Pluess2018; Veronese, Castiglioni, Tombolani, & Said, Reference Veronese, Castiglioni, Tombolani and Said2012). Child participants completed these measures at T1 and T2.
Well-being
We assessed well-being by using the World Health Organisation—Well-Being Index (WHO-5; Bech, Reference Bech2004), which is a widely used five-item measure of subjective well-being (M = 41.16; SD = 19.24, α = .93). Higher scores indicate greater well-being. The WHO-5 is sensitive to changes in response to intervention (Topp, Østergaard, Søndergaard, & Bech, Reference Topp, Østergaard, Søndergaard and Bech2015).
Optimism
Optimism was assessed by using four items from the Youth Life Orientation Test (Ey et al., Reference Ey, Hadley, Allen, Palmer, Klosky, Deptula and Cohen2005; M = 4.79; SD = 2.82, α = .82). Higher scores indicate greater optimism.
Self-esteem
Self-esteem was measured by using one item from the Lifespan Self-Esteem Scale (Harris et al., Reference Harris, Donnellan and Trzesniewski2018), which asked, “How do you feel about the kind of person you are?” Responses ranged from 1 = really sad to 5 = really happy (M = 2.92; SD = 1.22).
Depressive symptoms
We used a 10-item version of the Center for Epidemiological Studies Depression Scale for Children (CES-DC; Roberts, Andrews, Lewinsohn, & Hops, Reference Roberts, Andrews, Lewinsohn and Hops1990) to assess participants’ depressive symptoms. This shortened version was used for its reliability and validity in refugee children (Moghames et al., Reference Moghames, McEwen and Pluess2018). Higher scores indicate more depressive symptoms (M = 17.11; SD = 6.88, α = .92).
Focus Groups
The children were asked open-ended questions about their experiences in the intervention, which components they found to be particularly useful or not useful, how the intervention affected them, and what they would change about the intervention (M = 27 min). The focus groups were conducted in and transcribed from Arabic and Farsi and translated back to English for analysis. Children in our focus groups ranged in age from 8 to 14 years old. Rich and varied information can be gathered from children this age and younger, provided that the questions are developmentally appropriate and open-ended (Greene & Hill, Reference Greene, Hill, Greene and Hogan2005).
Data Analysis
We first tested the comparability of the intervention and wait-listed control group at T1 by using independent samples t tests and chi-square statistics. To evaluate the effectiveness of the intervention, we conducted repeated-measures ANOVAs with Greenhouse–Geisser corrections to test whether the intervention group changed more from T1 to T2 than the wait-listed group did on our survey measures. The outcomes of interest were well-being, optimism, self-esteem, and depressive symptoms. This allowed us to look for differences in within-person patterns of change in our outcomes over time (from T1 to T2) that were dependent on whether participants were in the treatment or control group.
The focus group data were subjected to a content analysis by hand (by the first two authors). This involved repeated review of the transcriptions by the first and second authors, a line-by-line coding, followed by a descriptive analysis of the coded data (Hsieh & Shannon, Reference Hsieh and Shannon2005). Specifically, the first and second authors engaged in open coding, compared and contrasted codes and emerging interpretations, solidified the codes, categorized data that were relevant to our research within these codes, and then described the pattern of results. Focus group data were used to identify specific components in the intervention that may explain treatment effects and to identify components of the intervention that should be changed in future treatments. We followed established methods for improving the trustworthiness of the data collection, analysis, and reporting (Elo et al., Reference Elo, Kääriäinen, Kanste, Pölkki, Utriainen and Kyngäs2014).
Results
The intervention and wait-listed groups did not differ at T1 in age, t (68) = 0.52, p = .61, (intervention group: M = 10.63, SD = 2.10, range = 7–14 years old; control group: M = 10.87, SD = 1.85, range = 8–14 years old), well-being scores, t (53) = -0.17, p = .87, optimism scores, t (59) = 0.61, p = .54, or depressive symptoms, t (51) = 0.02, p = .98. They did differ in self-esteem, with the wait-listed group having significantly higher self-esteem at T1 (M = 3.30; SD = 0.92) than the treatment group (M = 2.48; SD = 1.38), t (60) = 2.79, p = .007. There were also gender differences at T1. The wait-list group had a greater proportion of male participants than the treatment group did (47.4% vs. 21.2%, respectively), χ2 (1, 71) = 5.30, p = .021.
Program Effectiveness (Quantitative)
Compared with the wait-listed group, the intervention group reported significant improvements in well-being, F (1, 46) = 42.99, ηp2 = .48, p < .001, optimism, F (1, 53) = 27.16, ηp2 = .34, p < .001, self-esteem, F (1, 56) = 29.11, ηp2 = .40, p < .001, and depressive symptoms, F (1, 31) = 62.14, ηp2 = .67, p < .001 (Table 3, Figure 1). The effect sizes suggest that when participants took part in the intervention, they experienced large increases in positive outcomes (subjective well-being, optimism, and self-esteem) and decreases in depressive symptomatology. We conducted sensitivity analyses to test whether these results held when controlling for baseline differences in gender and self-esteem. Indeed, they did. When controlling for gender and self-esteem, the intervention group reported improved well-being, optimism, and depressive symptoms (Supplemental Table 2). When controlling for gender, the intervention group reported improved self-esteem (Supplemental Table 2).

Figure 1. Intervention effects on (a) well-being, (b) optimism, (c) self-esteem, and (d) depressive symptoms. The significance levels are for differences across time, within the treatment group and within the wait-list group. The error bars for all of the figures are ± 1 SE.
Program Effectiveness (Qualitative)
The focus group data also suggests intervention effectiveness in these areas. Participating children described that they had learned positive things about themselves, learned how to deal with challenges, had developed a more positive worldview, and had increased their social connections in response to the intervention. They felt that, as a result of the intervention, they had learned “a lot of things” including that they “have to be powerful, relying on strengths, and if there is a problem in my life I have to find a solution.” The children explained that before the intervention, “We didn't have hope. Hope, it was gone, but you have to catch your hope. So don't give up.” In line with improvements in their subjective well-being, the children explained that the intervention was “a new and nice experience” that caused them to “smile together and [be] happy together.” Participants repeated again and again that the intervention had led them to feel more optimistic and hopeful about the future, with increased feelings of hope and strength (e.g., “I felt like there is a hope in the life and even though a lot of bad things happened, still there is hope in life. People will be with you, friends will be with you, so the hope, there is a hope in life”). Finally, they described increased self-esteem due to a focus in the SFJ program on character strengths (e.g., “You give us a lot of advice and give us more trust in ourselves and more power, more strength”). No children specifically mentioned reductions in depressive or other mental health symptoms in response to the intervention.
The children identified working as a team, building social connections, and talking about their issues together to be the most effective and enjoyable parts of the intervention. When asked about the best part of the intervention, for instance, one child responded, “To be together, to talk together, to speak together about our stories, to share our stories and experiences. And, to be happy together.” Another said, “It's unusual living here to work as a team, so that this is why it is such a new and nice experience.” They identified a number of specific activities in the intervention as having led to positive changes in themselves, such as painting T-shirts, discussing the movie clip, coming up with plans to achieve their goals for the future, and writing about positive emotions. When asked what they would like to change about the SFJ program or what they did not like, most of the children did not want to make any changes. Those who did have suggestions wanted to lengthen the program, expand the scope of the program to include arts or language skills development, or to focus more on how to use personal strengths to overcome challenges.
Discussion
Given the unprecedented numbers of child refugees worldwide (UNHCR, 2018), the negative effects of war and displacement on children and adolescents (Reed et al., Reference Reed, Fazel, Jones, Panter-Brick and Stein2012), and the continued challenges that refugees face during and after displacement (Miller & Rasmussen, Reference Miller and Rasmussen2017), rigorously evaluated interventions that effectively promote resilience and positive functioning are urgently needed. The SFJ intervention is a structured, 6-day, strengths-based intervention that was developed for use with 7- to 14-year-old refugees that were living in camps. This pilot study was one of the first to prospectively test the immediate effects of a resilience-building, positive psychology intervention on children in a refugee camp setting. We used a quasi-randomized, wait-list design to evaluate whether the SFJ intervention improved positive functioning (well-being, optimism, and self-esteem) and decreased mental health difficulties (depressive symptoms) among refugee children and early adolescents who were living in camps in Lesvos. Our pilot evaluation of SFJ included survey measures before and after the intervention as well as focus groups immediately after and 3 months following the intervention.
Our findings indicate that the intervention led to improvements on all of the tested measures. Relative to the wait-listed controls, refugee children who took part in the intervention had increased well-being, optimism, and self-esteem as well as reduced depressive symptoms. The large effect sizes suggest that the effects of the intervention are substantial. Our focus group findings also point to the effectiveness of the intervention. The children described a number of positive changes in their thinking and in their lives as a result of having taken part in the intervention. The results provide evidence for the efficacy of this new intervention in the challenging context of refugee camps. Although most psychological interventions with refugees have an explicit focus on trauma or mental health (Fazel, Reference Fazel2018; Newnham et al., Reference Newnham, Kashyap, Tearne, Fazel, Morina and Nickerson2018), this pilot study suggests that child refugees can benefit greatly from an intervention that focuses on positive development and that this focus can also lead to reductions in mental health symptomatology.
This pilot evaluation study has a number of strengths, including the wait-listed pre- and post-test design, the measurement of positive mental health, quantitative and qualitative data collection, and a focus on children that live in refugee camps. However, there are a number of limitations. First, due to the complexities that are associated with conducting research inside refugee camps with limited resources and within a humanitarian crisis context, the intervention groups were not fully randomized. These space and staffing constraints also resulted in intervention groups that varied in size and gender distribution. The treatment and control groups differed at baseline in gender makeup and in self-esteem. Including these as covariates in the analyses did not affect the pattern of findings (Supplemental Table 2), but ideally treatment and control groups would be strictly comparable. Second, the sample is relatively small. Third, participants completed the post-test questionnaires immediately following the intervention, so any long-term effects are unclear. Finally, it is possible that the intervention effects may have resulted from group social cohesion or from interactions with a caring adult, rather than from the intervention itself. Although this is possible, we do not think that this is the case because the control children also took part in facilitated group activities and because the children in the focus groups identified specific activities from the intervention that they found to be effective. More rigorous evaluation of this intervention is needed.
Despite these limitations, the results of this pilot evaluation tentatively suggest the usefulness of the SFJ intervention for improving well-being and mental health among refugee children and adolescents who are living in precarious and insecure situations. Developing psychological resilience and strengthening protective factors for refugee youth are critical factors in promoting positive mental health and enabling them to cope with adversity (Measham et al., Reference Measham, Guzder, Rousseau, Pacione, Blais-McPherson and Nadeau2014), including the continued adversity of living in a refugee camp or resettlement (Silove et al., Reference Silove, Ventevogel and Rees2017). This pilot study builds on the evidence base for the effectiveness of positive psychology interventions for improving child well-being, which, to date have largely been conducted in high-income contexts (Bolier et al., Reference Bolier, Haverman, Westerhof, Riper, Smit and Bohlmeijer2013; Sin & Lyubomirsky, Reference Sin and Lyubomirsky2009). It also builds on work on well-being and adaptation among migrant children in Greece (e.g., Motti-Stefanidi, Reference Motti-Stefanidi2014; Motti-Stefanidi et al., Reference Motti-Stefanidi, Asendorpf and Masten2012) by evaluating how to improve these outcomes among child refugees.
We faced a number of challenges in conducting this pilot evaluation that should be informative for future work with this population. Negotiating access to refugee camps to deliver interventions or conduct research can be very difficult (Vogler, Reference Vogler2007). We found that it requires strong connections with camp administrators and a shared belief in the importance of the program. In one of the camps, Kara Tepe, translators from outside of the camp were not allowed in, so translators needed to be refugees from within the camp, which created some logistic challenges. These translators were included in the training. An additional challenge was that many organizations operate programs in the Lesvos camps over the summer months, with fewer programs offered at other times of the year. Access to the children may be limited to only a few hours a day in the summer, which could be problematic for some interventions. Developing programs that could be offered outside of the summer months would maximize access to children and camp resources. A further challenge to implementation in low-resource environments can be in the popularity of programs. In Kara Tepe, we were not able to deliver the program to all those who wanted to take part, which led to disappointment among many children and parents. Finally, many participating children spontaneously brought their parents with them at the start of the sessions each day to show them their drawings, positive thought notes, and collages. Interventions for displaced children that involve parents more closely and take a family-centered approach may be particularly beneficial, and they may build resilience at multiple levels (Bonanno, Romero, & Klein, Reference Bonanno, Romero and Klein2015; Denov, Fennig, Rabiau, & Shevell, Reference Denov, Fennig, Rabiau and Shevell2019; Kadir, Battersby, Spencer, & Hjern, Reference Kadir, Battersby, Spencer and Hjern2019).
Conclusions
Although promoting resilience is a key feature of humanitarian interventions in crisis contexts (e.g., United Nations Children's Emergency Fund, 2011), there are few interventions that specifically target positive development and resilience or measure efficacy in improving positive outcomes among refugee youth. This pilot study is the first to evaluate the effectiveness of SFJ, a brief, structured, group-based positive psychology intervention that was specifically designed for refugee children and adolescents. Besides significantly promoting children's well-being, optimism, and self-esteem, SFJ also reduced symptoms of depression. Our findings suggest that it is possible to mitigate some of the negative effects of war and displacement on children with the help of a scalable low-cost intervention that specifically targets children's psychological resilience and well-being.
Supplementary Material
The supplementary material for this article can be found at https://doi.org/10.1017/S0954579419001585.
Acknowledgments
We thank Lesvos Municipality and the NGOs Pikpa Lesvos Solidarity, Agkalia, and Caritas Hellas for mediating access to the participants in the camps. We thank Efi Latsoudi, Stavros Myroyiannis, Dimitris Lambrou, Athina Foka, and Katerina Efstathiou Selacha for their help and support to the project. We thank Christina Sergianni for providing training and assistance. We also thank Daniela Remfeldt, Gemma Fisher, Emily Keel, Joely Fashokun, and Dr Samuel Solomon for assisting the facilitators and Tharshana Selvakumar for data entry. Finally, we thank Saeed Mohammed, Wafa Oso, Jahid, and Moussa for interpreting during the intervention and Hadi Maboudi for the translation of the data collection documents.







