Depression in young children, a previously unrecognized childhood mental health concern, has received increasing attention since Luby and her colleagues’ seminal work demonstrating that depression is a valid diagnosis in preschoolers (Luby, Belden, Pautsch, Si, & Spitznagel, Reference Luby, Belden, Pautsch, Si and Spitznagel2009; Luby et al., Reference Luby, Heffelfinger, Mrakotsky, Hessler, Brown and Hildebrand2002). Since that time, evidence also has accrued that depression in young children is relatively stable (Lavigne et al., Reference Lavigne, Arend, Rosenbaum, Binns, Christoffel and Gibbons1998; Luby, Si, Belden, Tandon, & Spitznagel, Reference Luby, Si, Belden, Tandon and Spitznagel2009), and increases the risk for later symptoms of anxiety (Lavigne, Hopkins, Gouze, & Bryant, Reference Lavigne, Hopkins, Gouze and Bryant2015). Despite these data, relatively little attention has been paid to determining the factors that lead to the development and stability of depression in young children.
Developmental psychopathologists have stressed the importance of using longitudinal models that include multiple domains of risk factors for examining the development of childhood disorders (Masten & Cicchetti, Reference Masten and Cicchetti2010). Researchers studying externalizing disorders have heeded this call, and there is a large body of literature modeling the development of these types of problems in middle childhood and adolescence, including attention-deficit/hyperactivity disorder (Murray-Close et al., Reference Murray-Close, Hoza, Hinshaw, Arnold, Swanson, Jensen and Wells2014), aggression (Lansford et al., Reference Lansford, Sharma, Malone, Woodlief, Dodge, Oburu and Di Giunta2014), and antisocial behavior (Mulvey et al., Reference Mulvey, Steinberg, Fagan, Cauffman, Piquero, Chassin and Losoya2004). However, with the exception of two recent studies (Bufferd et al., Reference Bufferd, Dougherty, Olino, Dyson, Laptook, Carlson and Klein2014; Luby, Gaffrey, Tillman, April, & Belden, Reference Luby, Gaffrey, Tillman, April and Belden2014), less attention has been focused on examining longitudinal, multidomain models of depression in young children. Bufferd et al. assessed variables from a number of domains in 3-year-olds as predictors of depression at age 6, and reported that child psychopathology (anxiety and behavior problems), low inhibitory control, parental psychopathology, and life stress uniquely predicted the onset of age 6 depression. Data from Luby et al. also reveal a number of preschool predictors of depression in young, school-age children, including preschool depression, parental depression, unsupportive parenting, and life stress. While both of these studies made important contributions by identifying early childhood predictors of later depression, neither study examined the pathways through which these multidomain factors may have been associated with the levels of depression at age 6 or later. A clearer understanding of the mechanisms by which these risk factors might affect later depression can contribute to the development of improved prevention and treatment programs for young children.
The aim of this study was to extend the predictive findings of Bufferd et al. (Reference Bufferd, Dougherty, Olino, Dyson, Laptook, Carlson and Klein2014) and Luby et al. (Reference Luby, Gaffrey, Tillman, April and Belden2014) by examining, in a multidomain, longitudinal model of depression symptoms the pathways through which variables are associated with each other across three developmental periods: preschool, kindergarten, and formal school entry (ages 4–6). The theoretical underpinnings of this multidomain model were based on a transactional approach to child depression (Cicchetti & Toth, Reference Cicchetti and Toth1998), which posits that multiple factors occurring at different levels (domains) and at different ages affect the later emergence of depression symptoms. These domains include contextual, parental psychopathology, parenting, and child characteristics. We examined risk factors for childhood depression identified in the extant literature from each of these domains at ages 4 and 5 as predictors of depression at age 6. In the contextual domain we assessed socioeconomic status (SES), stress, and family conflict; in the parental psychopathology domain, parental depression; in the parenting domain, support/engagement, hostility, and scaffolding; and in the child domain, attachment security, temperamental negative affect, effortful control, and sensory regulation.
Contextual Factors
There is extensive evidence that low SES is related to depression in preschoolers, school-age children, and adolescents (Gilman, Kawachi, Fitzmaurice, & Buka, Reference Gilman, Kawachi, Fitzmaurice and Buka2003; Graham & Easterbrooks, Reference Graham and Easterbrooks2000; Wickrama & Vazsonyi, Reference Wickrama and Vazsonyi2011). Recent findings (Whalen et al., Reference Whalen, Luby, Tilman, Mike, Barch and Belden2016) also indicate that social adversity prior to age 5 predicts greater depression severity in both boys and girls.
Stress and family conflict are two other contextual factors shown to predict depression symptoms in young children. Specifically, two longitudinal studies (Bufferd et al., Reference Bufferd, Dougherty, Olino, Dyson, Laptook, Carlson and Klein2014; Luby, Belden, & Spitznagel, Reference Luby, Belden and Spitznagel2006) revealed that life stress at age 3 predicted depression at later ages. Cote et al. (Reference Côté, Boivin, Liu, Nagin, Zoccolillo and Tremblay2009) reported that higher levels of family conflict predicted higher levels of anxiety and depression symptoms between the ages of 1.5 and 5.
Rather than having a direct impact on child symptoms, however, it is likely that these distal, contextual factors have indirect effects on early-appearing depression symptoms via their associations with other factors (e.g., parental depression and parenting) that are more proximal to the child. Thus, our model examined the effect of SES, stress, and conflict at age 4 on parental depression and three aspects of parenting (support, hostility, and scaffolding) at age 5, and then the effects of these age five variables on age 6 depression symptoms.
Parent domain
In the parent psychopathology domain, the association between parental depression and child internalizing disorders, particularly depression, has received a great deal of attention. Studies of children of all ages consistently show a moderate to strong relation between parental depression and child depression (Downey & Coyne, Reference Downey and Coyne1990). There is recent cross-sectional evidence (Hopkins, Lavigne, Gouze, LeBailly, & Bryant, Reference Hopkins, Lavigne, Gouze, LeBailly and Bryant2013) that parental depression is related to preschool depression symptoms. Bufferd et al. (Reference Bufferd, Dougherty, Olino, Dyson, Laptook, Carlson and Klein2014) reported that maternal depression assessed at age 3 years predicted child depression at age 6. Although these associations may reflect genetic influences, it is also well known that parental depression affects parenting. Moreover, the cross-sectional study (Hopkins et al., Reference Hopkins, Lavigne, Gouze, LeBailly and Bryant2013) revealed that, in addition to its direct effect on preschool depression, parental depression also had indirect effects via its association with parenting and child temperament. Thus, longitudinal studies are needed that examine the pathways by which parental depression leads to child depressive symptoms over time via parenting and child characteristics.
Parenting
Unsupportive parenting, control, and hostility have each been associated with child depression symptoms. A meta-analysis (McLeod, Weisz, & Wood, Reference McLeod, Weisz and Wood2007) of studies examining the relation between these dimensions of parenting and child depression indicates that parenting has a small, but statistically significant effect, on child depression. There is also recent evidence that unsupportive parenting (Kok et al., Reference Kok, Linting, Bakermans-Kranenburg, van Ijzendoorn, Jaddoe, Hofman and Tiemeier2013; Luby et al., Reference Luby, Gaffrey, Tillman, April and Belden2014) and parental hostility (Hopkins et al., Reference Hopkins, Lavigne, Gouze, LeBailly and Bryant2013) play a role in depression in preschool-age children. Although it seems clear that parenting is related to early-appearing depression, further research is needed to illuminate these relationships, as well as to examine if parenting effects have indirect effects via their association with child characteristics (i.e., temperament).
Child domain
Temperament
There is extensive evidence that the reactive aspect of temperament, negative affect (NA), is a risk factor for internalizing symptoms in preschool children (Eisenberg et al., Reference Eisenberg, Cumberland, Spinrad, Fabes, Shepard, Reiser and Guthrie2001, Reference Eisenberg, Valiente, Spinrad, Cumberland, Liew, Reiser and Losoya2009; Muris & Ollendick, Reference Muris and Ollendick2005). The regulatory aspect of temperament, effortful control (EC), also has been concurrently and prospectively linked to internalizing disorders in young children (Eisenberg et al., Reference Eisenberg, Valiente, Spinrad, Cumberland, Liew, Reiser and Losoya2009; Muris & Ollendick, Reference Muris and Ollendick2005).
Sensory regulation (SR) has been recognized as a component of temperament that is related to later adjustment since the seminal work of Thomas and Chess (Reference Thomas and Chess1977) in the New York Longitudinal Study. Despite this early recognition, however, recent studies have not assessed or focused on this dimension of temperament independently to determine if it is a risk factor for child disorders. Instead, it has been treated as a component of other temperament variables. For example, Rothbart's widely used temperament questionnaire, the Child Behavior Checklist (Rothbart, Ahadi, Hershy, & Fisher, Reference Rothbart, Ahadi, Hershy and Fisher2001), subsumes sensory items within the NA and EC factors. There is evidence, however, that SR is a dimension of temperament that is distinct from both NA and EC. Specifically, Gouze, Lavigne, Hopkins, Bryant, and LeBailly (Reference Gouze, Lavigne, Hopkins, Bryant and LeBailly2012) reported that a confirmatory factor analysis failed to replicate Rothbart's two-factor model and that a three-factor model that included separate factors of NA, EC, and SR was a better fit. There is also evidence that sensory overresponsivity frequently co-occurs with both externalizing and internalizing problems in school-age children (Ben-Sasson, Carter, & Briggs-Gowan, Reference Ben-Sasson, Carter and Briggs-Gowan2009). Cross-sectional data (Hopkins et al., Reference Hopkins, Lavigne, Gouze, LeBailly and Bryant2013) indicate that SR is related to both depression and anxiety in young children. These findings suggest that SR is a distinct dimension of child temperament that may well be a risk factor for depression in young children, but its significance as a risk factor requires longitudinal data.
Attachment security
A recent meta-analysis of studies of attachment security indicates that insecure attachment in early childhood predicts later internalizing symptoms with a small to medium effect size (Madigan, Atkinson, Laurin, & Benoit, Reference Madigan, Atkinson, Laurin and Benoit2013). Because secure attachment predicts better self-regulation (Sroufe, Reference Sroufe2005), it is likely that more secure preschool attachment would lead to better EC at age 5, which in turn would be related to fewer depression symptoms at age 6. Thus, we examined if attachment at age 4 had indirect effects on age 6 depression symptom levels via its association with age 5 EC.
The Present Study
To summarize, there is consistent evidence that variables from several domains, including contextual factors, parental characteristics (i.e., parental depression), parenting, attachment security, and child temperament, are associated with depression symptoms in young children. To our knowledge, however, only one study (Hopkins et al., Reference Hopkins, Lavigne, Gouze, LeBailly and Bryant2013) has tested a model of risk factors for depression symptoms in young children that included variables from each of these domains. Findings from that study are informative about the factors related to preschool depression symptoms; however, they cannot address causality or shed light on the direction of effects due to the cross-sectional design. The aim of the present study, therefore, was to extend the cross-sectional study (Hopkins et al., Reference Hopkins, Lavigne, Gouze, LeBailly and Bryant2013), and the studies of early childhood predictors of later depression by Bufferd et al. (Reference Bufferd, Dougherty, Olino, Dyson, Laptook, Carlson and Klein2014) and Luby et al. (Reference Luby, Gaffrey, Tillman, April and Belden2014) by examining multidomain risk factors at two developmental periods, and the pathways through which these factors are associated with levels of depression symptoms at age 6. Based on previous empirical findings, we predicted that contextual, parent, parenting, and child factors assessed at age 4 would be related to factors in other domains at age 5 that, in turn, would be associated with age 6 symptom levels. Specifically, we hypothesized that at child age 4: (a) contextual factors of SES, stress, and conflict would be associated with age 6 depression symptoms via pathways through age 5 parental depression and parenting; (b) parental depression would be associated with age 6 child depression via age 5 parenting and age 5 child temperament variables of NA, EC, and SR; (c) parenting factors of hostility, support, and scaffolding would be associated with age 6 child depression via age 5 child NA, EC, SR, and attachment security; and (d) attachment security would be associated with age 6 child depression via age 5 EC. We also hypothesized that age 5 parental depression, parental hostility, support, and scaffolding, and child attachment security, NA, EC, and SR would have direct effects on age 6 depression symptoms.
We further extended the work of Bufferd et al. (Reference Bufferd, Dougherty, Olino, Dyson, Laptook, Carlson and Klein2014) and Luby et al. (Reference Luby, Gaffrey, Tillman, April and Belden2014) by carefully considering the pathways by which multidomain factors at preschool and kindergarten entry are associated with both the levels of depression symptoms between preschool and school entry and increases in depression symptoms across those same developmental periods. That is, we examined two distinctly different models. The first model examined the pathways by which age 4 and 5 multidomain factors are associated with levels of depression symptoms at age 6 regardless of their time of onset. This model answers the question “What are the pathways by which age 4 and age 5 multidomain factors contribute to the levels of depression symptoms at age 6 regardless of the age of onset of the depression symptoms.”
The second model examines the risk factors and pathways that contribute to the change in depressive symptoms between preschool and formal school entry, thus addressing the question “What multidomain factors and pathways between age 4 and age 5 are associated with an increase in depression symptoms between preschool and formal school entry.” Both of these questions are distinct and important in the field of developmental psychopathology: the former to address risk factors for the levels of depression symptoms that could affect children's psychological functioning and academic progress after entering formal schooling; the latter to address risk factors for increases in these symptoms between preschool and formal school entry.
Method
Participants
Participants were initially recruited at age 4 from 13 public schools and 23 pediatric practices in a large urban area for a longitudinal study that would include two follow-up assessments, at ages 5 and 6. The initial sample included 796 preschool children (mean age = 4.44 years) and their primary caregiver, and an approximately equal number of boys and girls (49.1% boys; n = 391). The racial/ethnic composition (parent identified) was 433 White (54.4%), 162 Hispanic (20.4%), 133 African American (16.7%), 19 Asian (2.4%), 35 multiracial or other (4.4%), and 14 not reporting (1.8%). There also was a wide range of SES (Hollingshead, Reference Hollingshead1975): Specifically, 303 Class I (highest; 38.1%), 290 Class II (36.4%), 79 Class III (9.9%), 63 Class IV (7.9%), and 61 Class V (7.7%). The majority of parents, 78.1% (n = 622), were married. Mothers completed 765 evaluations, and primary caretaker fathers completed 31.
Sample retention across all three waves was 78.6% (N = 626). Dropouts included a significantly greater proportion of minorities, χ2 (5, N = (796) = 77.7, p = .001, and a greater proportion of low SES families, χ2 (4, N = (796) = 69.61, p = .001, compared to families who completed all three waves of data collection. Younger child age at Wave 1 also was associated with dropout status, t (773) = 2.41, p = .02. As discussed in the Data Analysis section, missing data were imputed, so the final sample N for this report was 796.
Measures
A multi-informant approach was used that included parent reports and interviews to assess outcomes and several risk factors, and observer ratings to assess child attachment and parent scaffolding. Child self-reports could not be used because of the children's ages. We used multiple indicators of a construct to estimate latent factors and reduce measurement error associated with single measures whenever possible. When multiple indicators could not be used, either a single measure or a composite measure was used to assess the particular construct (see Data Analysis section for details). Internal consistencies are reported. When internal consistencies are based on multiple items for a single measure, α coefficients are reported. When internal consistency is reported for latent factors with a few (2–3) indicators, α coefficients are not appropriate and composite reliabilities are reported (Mosier, Reference Mosier1943).
Contextual measures
SES
Demographic information on the child's age, sex, race, and parent's education and employment was obtained by parent report, and social class was calculated using the Hollingshead Four-Factor Index of Social Status (Hollingshead, Reference Hollingshead1975).
Stress
Stress was assessed with three psychometrically sound parent-report questionnaires: the Perceived Stress Scale (Cohen, Kamarck, & Mermelstein, Reference Cohen, Kamarck and Mermelstein1983); (b) the McCubbin Family Changes & Strains Scale (McCubbin & Patterson, Reference McCubbin, Patterson, McCubbin, Thompson and McCubbin1996); and (c) the Parenting Stress Index, Short Form (Abidin, Reference Abidin1995). The stress factor had a composite reliability of .80 at age 4.
Family conflict
Three conflict scales: (a) the McCubbin Family Distress Index (McCubbin, Thompson, & Elver, Reference McCubbin, Thompson, Elver, McCubbin, Thompson and McCubbin1996); (b) the Family Problem Solving/Communication Scale (McCubbin, McCubbin, & Thompson, Reference McCubbin, McCubbin, Thompson, McCubbin, Thompson and McCubbin1996); and (c) the Family Environment Scale conflict scale (Moos & Moos, Reference Moos and Moos1986) were used to derive a composite family conflict measure (composite reliability = .71).
Parent measures
Parental depression
Two widely used self-report measures, the Beck Depression Inventory (Beck, Steer, & Garbin, Reference Beck, Steer and Garbin1988) and the Center for Epidemiologic Studies Depression Scale (Radloff, Reference Radloff1977), were used to assess parental depression at ages 4 and 5. The Beck Depression Inventory is a widely used 21-item self-report inventory; the Center for Epidemiologic Studies Depression Scale, a 20-item, self-report measure, was designed specifically to assess depression symptoms in a community sample. The composite reliability for parental depression was .89 at age 4 and .88 at age 5.
Parenting measures
Parent support and hostility
Support/engagement (hereafter referred to as support) and hostility/coercion (hereafter referred to as hostility) were assessed with the Parent Behavior Inventory (PBI; Lovejoy, Weis, O'Hare, & Rubin, Reference Lovejoy, Weis, O'Hare and Rubin1999). The PBI is a 20-item parent-report measure of parenting behavior, not attitudes. Items from each scale were divided into three parcels to provide three indicators of the latent factors of support/engagement (α = 0.81) and hostility (α = 0.87), as recommended by Brown (Reference Brown2006). The composite reliabilities for support at ages 4 and 5 were .85 and .91, respectively, and for hostility they were .73 and .68.
Parent scaffolding
Scaffolding was assessed at ages 4 and 5 with an observational measure, the 3-Boxes-Task (NICHD Early Childhood Research Network, 1999), which consists of a 15- to 20-min videorecorded, semistructured interaction paradigm in which the parent and child first engage in two tasks (developmentally appropriate tasks are used at each age) that are difficult for the child to accomplish on his/her own, followed by a free-play interaction. Coders rate the parent on 7-point Likert scales for supportive presence, respect for child autonomy, quality of assistance, cognitive stimulation, confidence, and hostility (reverse-scored). Interrater reliabilities in the present study ranged from .80 for quality of assistance to .69 for maternal hostility, with a mean reliability of .74. Factor analysis of the six ratings revealed that a one-factor solution provided the best fit to the data, and we labeled this factor scaffolding. Three parcels were created from the six ratings. Composite reliabilities for scaffolding were .81 at age 4 and .78 at age 5.
Child measures
NA
NA was assessed at ages 4 and 5 with the Children's Behavior Questionnaire (CBQ; Rothbart et al., Reference Rothbart, Ahadi, Hershy and Fisher2001). Following Lengua, West, and Sandler (Reference Lengua, West and Sandler1998) procedures were used to reduce item contamination with measures of child psychopathology (see Data Analysis section). A single measure of NA was used (α = 0.78 at age 4 and 0.66 at age 5), with items from the CBQ scales for discomfort, sadness, fear, anger/frustration, and soothability (negatively loaded).
EC
EC also was assessed at ages 4 and 5 with the CBQ. After reducing item contamination (see Data Analysis section), the two CBQ indicators of EC were attentional focusing and inhibitory control (composite reliability = .72 at age 4 and .78 at age 5).
SR
SR was assessed at ages 4 and 5 with the Short Sensory Profile (SSP; McIntosh, Miller, Shyu, & Hagerman, Reference McIntosh, Miller, Shyu and Hagerman1999), a 38-item parent-report questionnaire. Some SSP items are similar to items on measures of child psychopathology; thus, we used procedures (described in the Data Analysis section) to reduce item contamination. This yielded three SR indicators measuring the tactile, movement, and low-energy components of SR (composite reliability = .81 at age 4 and .70 at age 5).
Attachment
Attachment was assessed at ages 4 and 5 with the Attachment Q-Sort (AQS; Waters, Reference Waters1987), which provides a continuous measure of attachment security. The AQS is an ecologically valid measure of secure base behavior, and has strong reliability and convergent validity with the Strange Situation (van IJzendoorn, Vereijken, Bakermans-Kranenburg, & Riksen-Walraven, Reference van IJzendoorn, Vereijken, Bakermans-Kranenburg and Riksen-Walraven2004). Graduate student research assistants completed the AQS after a 2- to 3-hr home observation (mean interrater reliability on a 20% random sample of home visits = .77).
IQ estimate
The Peabody Picture Vocabulary Test (α = 0.94), a measure of receptive language (Dunn & Dunn, Reference Dunn and Dunn1997), was administered at age 4 to ensure that children met the inclusion criterion of not being developmentally delayed.
Child depression
Child depression symptoms at each age were assessed by both interview and parent report. A developmentally appropriate interview, the Diagnostic Interview Schedule for Children-Parent Scale—Young child version (DISC-YC; Fisher & Lucas, Reference Fisher and Lucas2004), a fully structured interview, was administered by research assistants trained to a criterion of reliability. The symptoms count measure of the DISC-YC was used in the data analysis, which required the use of continuous measures.
The Child Symptom Inventory (Gadow & Sprafkin, Reference Gadow and Sprafkin2000), which consists of symptom items derived from DSM-IV diagnostic criteria, was used as the parent-report measure of depression. Depression symptoms were assessed with the major depression scale and the dysthymia scale. Composite reliabilities for the child depression composite were .70, .84, and .85 at ages 4, 5, and 6, respectively.
Procedure
Initially, research assistants approached parents at pediatric offices and preschools to provide study information and determine interest. Interested parents were then contacted by phone, and a home visit was scheduled. All measures were completed in the home. Parents were recontacted by phone when the child turned 5 and 6 to schedule the two additional home visits, during which the study questionnaires, observational measures, and DISC-YC were readministered. The institutional review board of each author's institution provided study approval, and written consent to participate was obtained at each visit.
Data analysis
Inspection of the data revealed that less than 5% of the data were missing within each age group. Little's missing completely at random (MCAR) test was significant (6117.246, df 5627, p < .0001). We then imputed missing data using SPSS V15.0 Expectation Maximization methodology using maximum likelihood procedures for multiple imputation because imputation is generally less biased than listwise deletion (Graham, Reference Graham2009).
We used a procedure developed by Lengua et al. (Reference Lengua, West and Sandler1998) to reduce item contamination between scales for behavior problems, temperament (Eisenberg et al., Reference Eisenberg, Valiente, Spinrad, Cumberland, Liew, Reiser and Losoya2009; Lengua et al., Reference Lengua, West and Sandler1998), and SR (Ben-Sasson et al., 2007) that could inflate the relationships between EC, NA, SR, and depression symptoms. This procedure, which combined the use of expert opinion and confirmatory factor analysis, has been described elsewhere (reference withheld) and was used to create the EC, NA, and SR scales used in these analyses.
The hypothesized models were examined using SEM with LISREL 8.8 (Joreskog & Sorbom, Reference Joreskog and Sorbom2006). Using a two-step analytic approach (Anderson & Gerbing, Reference Anderson and Gerbing1988), a confirmatory factor analysis was done first to test the goodness of fit of the measurement models before examining the structural models. We used multiple measures of each construct whenever possible to control for measurement error. When there was only one developmentally appropriate manifest indicator and that measure involved a questionnaire with multiple items, individual items were combined into unidimensional subsets (parcels) to create multiple indicators, a procedure for estimating latent factors that avoids problems of nonnormality sometimes associated with a single indicator (Brown, Reference Brown2006). When the only available manifest indicator of the appropriate construct involved a single item or a good fit for a latent construct could not be achieved using multiple indicators, a composite indicator was created by summing the standardized scores from multiple scales (Nunnally & Bernstein, Reference Nunnally and Bernstein1994).
To correct for multivariate nonnormality, we have reported the Satorra–Bentler scaled chi-square (SB χ2; Satorra & Bentler, Reference Satorra, Bentler, von Eye and Clogg1994), although we did not use it to assess overall model fit because that measure is inflated by large sample sizes (Bollen, Reference Bollen1989; Brown, Reference Brown2006). We followed Bryant and Satorra's (Reference Bryant and Satorra2012) guidelines to obtain scaled maximum-likelihood chi-square values using LISREL 8. Brown (Reference Brown2006) recommends using multiple indices to assess model goodness of fit, including an index of absolute fit (standardized root mean square residual, SRMR), an index adjusting for model parsimony (root mean square error of approximation, RMSEA), and comparative fit indices (nonnormed fit index, NNFI; comparative fit index, CFI). Experts differ on the criteria for establishing acceptable goodness of fit for commonly used indices. For RMSEA, Hu and Bentler (Reference Hu and Bentler1999) consider a reasonably good fit to be close to .06 or below, while Brown (Reference Brown2006) and Cudeck and du Toit (Reference Cudeck, du Toit, Millsap and Maydeu-Olivares2009) describe <.08 as adequate, and MacCallum, Browne, and Sugawara (Reference MacCallum, Browne and Sugawara1996) consider RMSEA values between .08 and .10 to be “mediocre.” For NNFI and CFI, Bentler and Bonett (Reference Bentler and Bonett1980) state that relative fit indices (e.g., NNFI and CFI) >.90 indicate acceptable model fit; Hu and Bentler (Reference Hu and Bentler1999) suggested that only relative fit indices above .95 indicate acceptable model fit. Marsh, Hau, and Wen (Reference Marsh, Hau and Wen2004), however, argue against Hu and Bentler's (Reference Hu and Bentler1999) stringent criteria, and support retaining Bentler and Bonett's (Reference Bentler and Bonett1980) criterion of .90. For SRMR, a value of < .08 is often recommended (Brown, Reference Brown2006). In this study, we describe models with RMSEA < approximately .06, NNFI > .95, CFI > .95, and SRMR of < .08 as good fitting models. If RMSEA is > .06 but < .08, NNFI >. 90 but < .95, CFI >.90 but < .95, and SRMR < .08, the model fit is described as moderately good. Models whose fit indices do not reach these thresholds are described as poor fitting.
Different approaches have been advocated for determining the statistical significance of indirect effects. There is general agreement that the original approach advocated by Baron and Kenny (Reference Baron and Kenny1986), sometimes described as the normal theory approach (Mallinckrodt, Abraham, Wei, & Russell, Reference Mallinckrodt, Abraham, Wei and Russell2006), is problematic (Mallinckrodt et al. Reference Mallinckrodt, Abraham, Wei and Russell2006). Two commonly used approaches advocated by Mallinckrodt et al., bootstrapping and joint significance testing (JST), have both advantages and disadvantages. Bootstrapping procedures involve data resampling procedures and calculation of the magnitude of the indirect effect and 95% confidence intervals (CIs). In JST, an indirect path is considered statistically significant if both path coefficients are significant, and the magnitude of the indirect effect is the product of the two path coefficients. Bootstrapping is often advocated, but may result in elevated levels of Type I error (Mallinckrodt et al., Reference Mallinckrodt, Abraham, Wei and Russell2006; Taylor & MacKinnon, Reference Taylor and MacKinnon2012). In contrast, JST may perform better than bootstrapping with respect to Type I error (Mallinckrodt et al., Reference Mallinckrodt, Abraham, Wei and Russell2006; Taylor & MacKinnon, Reference Taylor and MacKinnon2012). MacKinnon et al. concluded that JST was superior to 14 different approaches (none of which included bootstrapping). With large samples, power is similar for both tests, but slightly better for JST when the magnitude of both paths in the indirect effect is small (Taylor & MacKinnon, Reference Taylor and MacKinnon2012). Because it is not clear which procedure is preferable, we discuss results for indirect effects with regard to both procedures.
Results
Measurement models
The first measurement model for Model 1 showed moderately good fit, SB χ2 (495, N = 796) = 2359.57, RMSEA = .053, NNFI = .94, CFI = .95, SRMR = .06. This model included 13 latent factors with multiple indicators: (a) parental depression at ages 4 and 5, with the original two parent depression scales as manifest indicators for each factor; (b) parental hostility at ages 4 and 5, with three parcels of items from the PBI hostility scale as indicators at both ages; (c) parental support at ages 4 and 5, with three parcels of items from the PBI support scale at each age; (d) parental scaffolding at ages 4 and 5 with three parcels of items from the observational measures; (e) EC at ages 4 and 5, with two scales from the CBQ at each age; (f) SR at ages 4 and 5, with three parcels of expert items from the SSP as indicators; (g) the outcome measure of depression symptoms, with three indicators. The model also included three factors with a single-composite indicator (age 4 conflict, age 4 stress, and ages 4 and 5 NA), as well as three factors with a single-item indicator (age 4 SES and ages 4 and 5 attachment).
The measurement model for Model 2 also showed a good fit overall, SB χ2 (226, N = 796) = 3217.52, RMSEA = .05, NNFI = .95, CFI = .95, SRMR = .07. This model included two additional latent factors: child depression symptoms at ages 4 and 5, with three indicators per variable, with two from the Child Symptom Inventory and one from the DISC-YC. The other factors are the same as in model 1. The table of correlations among the manifest indicators in both models is available online.
Model 1: Depression level at age 6
The initial longitudinal model showed moderately good fit, SB χ2 (721, N = 796) = 2359.76, RMSEA = .053, NNFI = .94, CFI = .95, SRMR = .06. Figure 1 shows all the paths examined and Figure 2 shows the significant paths in Model 1, with all of the path coefficients (PC) presented in Table 1. Before examining cross-domain pathways, we examined whether there were stable, persistent effects from the parent, parenting, and child factors over time (ages 4–5) on child depression symptoms at age 6. Model 1 showed that parent depression was highly stable from age 4 to age 5 (PC = .62, p < .001). In addition, age 5 parent depression was significantly associated with age 6 child depression (PC = .17, p < .001). Thus, there was a persistent effect of age 4 parent depression on the level of child depression symptoms at age 6 via its stable effects on age 5 parent depression (indirect effect from JST = .10; from bootstrapping, PC = .10, 95% CI [.05, .2]). The indirect effect assessed with JST and bootstrapping were both significant.

Figure 1. Schematic representation of all paths examined in Model 1 of factors at age 4 and 5 associated with levels of symptoms of depression at age 6 without autoregressive effects for depression at ages 4 and 5. SES, socioeconomic status. EC, effortful control. NA, negative affect. SR, sensory regulation.

Figure 2. Significant pathways in multidomain Model 1 of factors at age 4 and 5 associated with levels of symptoms of depression at age 6 without autoregressive effects for depression at ages 4 and 5. SES, socioeconomic status. EC, effortful control. NA, negative affect. SR, sensory regulation. *p < .05. **p < .01. ***p < .001.
Table 1. Path coefficients for depression Model 1 including age 6 child depression only (i.e., level of depression at age 6)

Note: SES, socioeconomic status. EC, effortful control. NA, negative affect. SR, sensory regulation. *p < .05. **p < .01. ***p < .001.
There were also persistent effects of two age 4 child factors, EC and SR, on age 6 child depression. Child EC was highly stable from age 4 to age 5 (PC = 1.36, p < .001), and age 5 child EC was associated with age 6 child depression (PC = –.18, p < .001). The indirect effect from age 4 EC to age 6 child depression via age 5 EC was significant (indirect effect from JST = –.24; indirect PC = –25; 95% CI [–1.0, –0.15]).
Child SR was also highly stable from age 4 to age 5 (PC = .89, p < .001), and age 5 child SR was associated with age 6 child depression (PC = –.25, p < .001). The indirect effect from age 4 SR to age 6 child depression via age 5 SR was significant (indirect PC from JST = –.22; indirect PC from bootstrapping = –.22; 95% CI [–.64, –.22]).
For child NA, stability of NA between age 4 NA and age 5 NA was moderately strong (PC = .43, p < .001). In addition, age 5 child NA was associated with age 6 child depression (PC = .09, p < .001). The significance of the indirect effect differed by method used to calculate its significance: for JST, the overall indirect effect was statistically significant (indirect PC = .04), while the indirect path using bootstrapping was not significant (indirect PC = –.04; 95% CI [–.05, 0]).
The stability of attachment security from age 4 to age 5 was statistically significant but low (PC = .21, p < .001). Age 5 attachment security was not associated with age 6 child depression.
There were no statistically significant, persistent effects of age 4 parenting on age 6 child depression symptoms. Parenting was stable from age 4 to age 5 for hostility (PC = .74, p < .001), support (PC = .59, p < .001), and scaffolding (PC = .40, p < .001), but the paths from age 5 parenting to age 6 child depression were not significant for any of the parent variables (hostility PC = .07, ns; support PC = –.04, ns; scaffolding PC = .00, ns).
Indirect effects
We then examined indirect effects across domains. The contextual factors of SES, stress, and conflict were assessed only at age 4. The other risk factors, including parental depression, parenting variables of parental support, hostility and scaffolding, and child NA, EC, SR, and attachment security, were assessed at both ages 4 and 5. In discussing these effects, it is important to note that the paths to age 5 variables all represent associations between the age 4 effect and changes in the effect measured at age 5, because each of the age 5 parent, parenting, and child variables were also assessed at age 4; thus, the age 5 assessment of that variable measures change from age 4 to 5.
Results based on JST are reported first, followed by those found with bootstrapping. There were six significant indirect effects based on JST. First, SES had a significant indirect effect on age 6 depression symptom levels via its negative effect on parent depression at age 5 (indirect PC = –.03; i.e., lower SES predicted increases in parental depression at age 5, which in turn were associated with higher levels of age 6 child depression). Second, higher levels of age 4 parental depression had an indirect effect on age 6 depression symptom levels via its association with increases in child NA from age 4 to 5 (indirect PC = .01). Third, higher levels of age 4 child EC were associated with a decrease in child NA from ages 4 to 5. This decrease, in turn, was associated with lower age 6 child depression symptom levels (indirect PC = –.02). Fourth, higher levels of age 4 NA were associated with higher levels of age 5 child EC. The increase in EC, in turn, was associated with decreases in child depression symptom levels at age 6 (indirect PC = –.04).
Fifth, there was an indirect effect of age 4 attachment via age 5 EC (indirect PC = .03) on age 6 child depression. In this path, the sign of the PC from age 4 attachment to age 5 EC was negative, which is the opposite of the expected direction, indicating that more secure attachment at age 4 was associated with a decrease in child EC from ages 4 to 5. Because this finding was theoretically implausible and inconsistent with that of prior studies, we sought to determine if a suppression effect was occurring by examining the correlation between age 4 attachment and age 5 EC. The Pearson correlation between age 4 attachment and age 5 EC was positive (r = .33) and had a sign in the opposite direction of the path coefficient (PC = –.19), a pattern that is consistent with negative suppression (Gaylord-Harden, Cunningham, Grant, & Holmbeck, Reference Gaylord-Harden, Cunningham, Grant and Holmbeck2010; Kline, Reference Kline2011). Negative suppression occurs when two predictor variables (A and B) are both significantly related to an outcome variable (C) in independent regression analyses. When both are entered simultaneously as predictors, the sign of one of the path coefficients changes direction. This occurs because the shared variance between A and B is “removed” when both are entered as predictors and the direction of that portion of the variance that is not shared by A and B has a relationship to C that is the opposite direction for the variable when both shared and unshared variance contribute to its effect.
Because negative suppression was present, the indirect path between age 4 attachment and age 6 child depression via age 5 EC was examined in a model that did not include other variables. The paths from age 4 attachment to age 5 EC (PC = .33, p < .001) and from age 5 EC to age 6 child depression (PC = –.41, p < .001) were significant and in the expected directions. The indirect path was significant via JST (PC for the indirect path = .14).
Sixth, there was an indirect path from caregiver support at age 4 via age 5 child NA. In this path, the sign of the PC from age 4 caregiver support to age 5 NA was negative, which is the opposite of the expected direction, indicating that more supportive parenting at age 4 was associated with an increase in child NA from ages 4 to 5. Again, this finding was theoretically implausible and inconsistent with that of prior studies, and so we determined if a suppression effect was occurring by examining the correlation between age 4 support and age 5 NA. The Pearson correlation between age 4 support and age 5 NA was negative (r = –.11) and had a sign in the opposite direction of the path coefficient (PC = .09), which indicates that a suppression effect was likely to be present. The path from age 4 support to age 5 NA (PC = –.11, p < .01) and from age 5 NA to age 6 child depression (PC = .28, p < .001) were significant and in the expected directions. The indirect path was significant via JST (PC for the indirect path = .03).
Because the model examined specific effects for each of a large number of risk factors, thereby estimating specific effects rather than variance attributable to a factor related to a large number of omitted variables, effect sizes and indirect effects were often small. There were no significant indirect effects for the two contextual risk factors of conflict and stress, for parenting domain factors of hostility and scaffolding skills, or for the child domain factor of temperamental SR.
In contrast to the rich set of indirect effects identified using the JST approach, the bootstrapping approach identified only one statistically significant effect: SES had an indirect effect on child depression symptoms at age 6. That is, the indirect effect of age 4 SES on age 6 child depression via parental depression was significant (PC = –.02, 95% CI [–.05, –.01]).
Model 2: Changes in depression from ages 4 to 6
It is useful to know how indirect effects are associated both with the level of child depression at age 6 and with the change in child depressive symptoms over time. Model 1 provides information about the relative contribution of the various multidomain factors to the absolute level of depression symptoms at age 6. To examine the contribution of other risk factors to changes in depression symptoms between ages 4 and 6, we examined a second model. Model 2 included the initial levels of depression symptoms at ages 4 and 5. Thus, Model 2 includes a latent depression factor at ages 4 and 5, as well as at age 6, and also includes paths for the autoregressions of depression between those ages. Figure 3 shows the paths examined and Figure 4 shows the significant paths, with all of the path coefficients presented in Table 2. This model showed a good fit overall, SB χ2 (969, N = 796) = 3217.52, RMSEA =.054, NNFI = .95, CFI = .95, SRMR = .07.
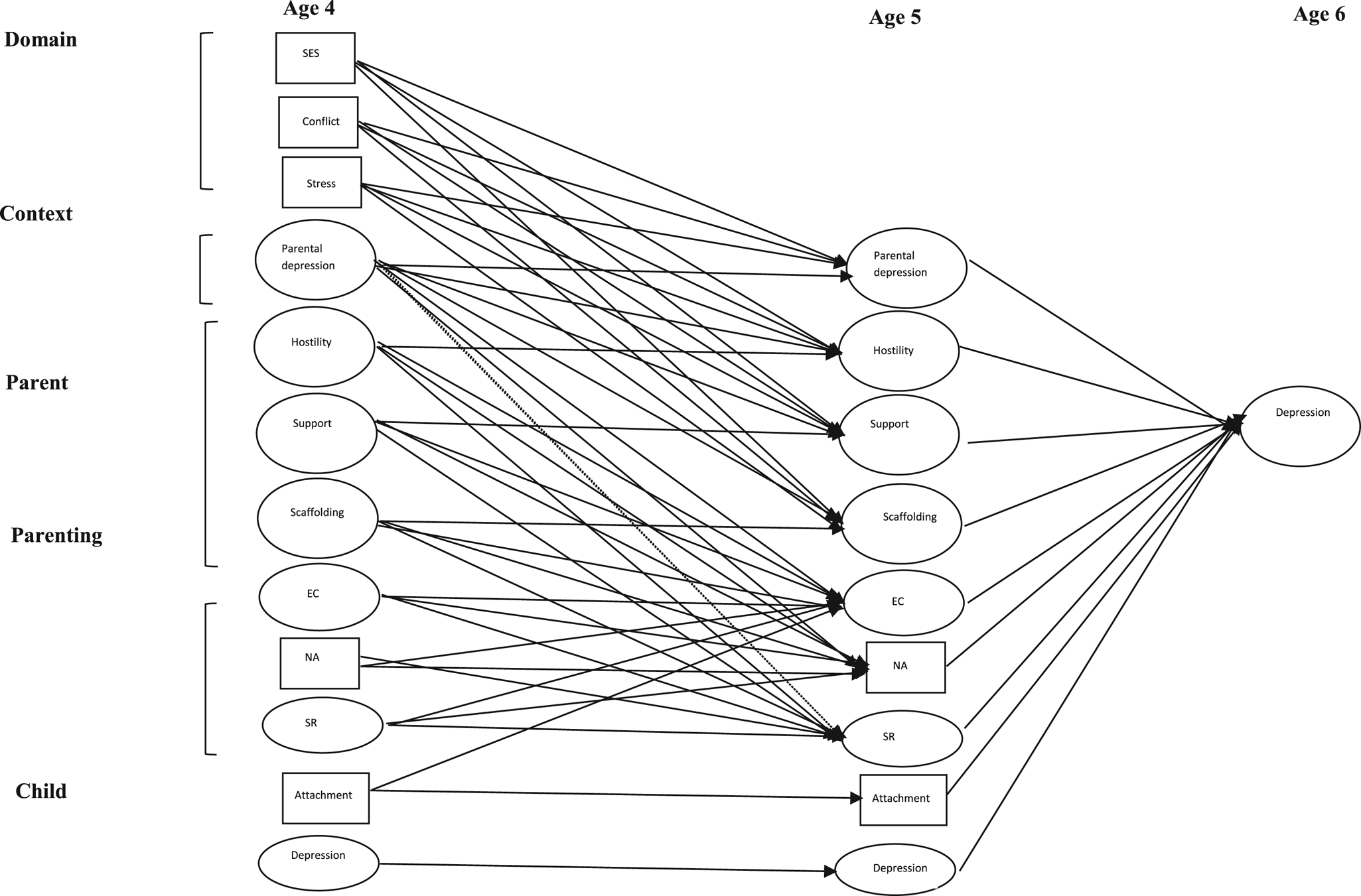
Figure 3. Schematic representation of all paths examined in multidomain Model 2 of factors at age 4 and 5 associated with levels of symptoms of depression at age 6 including autroregressive effects for depression at ages 4 and 5. SES, socioeconomic status. EC, effortful control. NA, negative affect. SR, sensory regulation.

Figure 4. Significant pathways in multidomain Model 2 of factors at age 4 and 5 associated with levels of symptoms of depression at age 6 including autroregressive effects for depression at ages 4 & 5. SES, socioeconomic status. EC, effortful control. NA, negative affect. SR, sensory regulation.
Table 2. Path coefficient for depression Model 2 including child depression at ages 4, 5, and 6 (i.e., model of changes in depression)

Note: SES, socioeconomic status. EC, effortful control. NA, negative affect. SR, sensory regulation. *p < .05. **p < .01. ***p < .001.
The paths from child depression symptoms at age 4 to age 5 symptoms (PC = .53, p < .001) and from age 5 symptoms to age 6 symptoms (PC = .36, p < .001) were both significant. Both paths also were moderate in size. The indirect effect of age 4 child depression symptoms on changes in these symptoms at age 6 via changes in child depression symptoms at age 5 also was significant by JST (indirect path PC = .19; PC = .19, 95% CI [.13, .24]). EC and SR were the only age 5 variables that had a significant, direct effect on changes in depression symptoms between ages 5 and 6. That is, higher levels of age 5 child EC predicted a decrease in child depression symptoms between the ages of 5 and 6 (PC = –.15, p < .01). Higher levels of age 5 SR also predicted a decrease in child depression symptoms between the ages of 5 and 6 (PC = –.16, p < .01).
Indirect effects
In Model 2, there was one significant indirect path from age 4 variables to changes in age 6 depression symptoms, from age 4 attachment to changes in child depression from ages 5 to 6 via age 5 EC. As occurred for this path in Model 1, negative suppression was present, with the sign of the path coefficient from age 4 attachment to age 5 EC (–.19) in the opposite direction of the Pearson correlation coefficient for these variables (r = .32). As a result, a structural model was examined that included only the variables for age 4 attachment, age 5 EC, and the autoregressions for child depression (paths from age 4 child depression to age 5 child depression, and from age 5 child depression to age 6 child depression) to allow for the assessment of the relation between age 4 attachment, age 5 EC, and change in child depression from age 5 to 6. In this model, the path from age 4 attachment to age 5 EC (PC = .33, p < .001) and from age 5 EC to age 6 child depression (PC = –.23, p < .001) were significant and in the expected direction. The indirect path was significant via JST (PC for the indirect path = .08).
Discussion
The aim of this study was to examine the effects of risk factors in multiple domains measured in preschool (age 4) and kindergarten (age 5) on age 6 depression symptoms, and on changes in levels of these symptoms between the ages of 4 and 6. To our knowledge, this is the first study to examine the potential effects of a broad range of risk factors, in multiple domains, across two important developmental periods, preschool and kindergarten, on early-appearing depression symptoms during first grade. It is, additionally, the first study to examine the complex, indirect pathways by which these multidomain risk factors are associated with one another and with age 6 child depression symptoms. Understanding the pathways by which these risk factors are associated with early childhood depression has significant public health implications for developing prevention and early intervention programs.
Model 1
The first model, which showed good overall model fit, showed, as predicted, that several age 5 risk factors, specifically, parental depression, child NA, EC, and SR, have significant, direct effects on age 6 depression symptoms. Although there is extensive evidence that each of these variables is related to child depression (Bufferd et al., Reference Bufferd, Dougherty, Olino, Dyson, Laptook, Carlson and Klein2014; Cote et al., Reference Côté, Boivin, Liu, Nagin, Zoccolillo and Tremblay2009; Luby et al., Reference Luby, Gaffrey, Tillman, April and Belden2014; Whalen, Sylvester, & Luby, Reference Whalen, Sylvester and Luby2017), Model 1 also reveals a novel finding regarding the effects of these variables on later child depression. Specifically, this model shows that each of these risk factors has persistent effects, beginning at age 4, on the same factor at age 5, which in turn lead to higher levels of depression symptoms at age 6.
Model 1 also showed that there were several indirect pathways from variables in the contextual, parenting, and child domains at age 4 that had indirect effects on age 6 child depression symptom levels through pathways to age 5 variables in other domains. Specifically, there were indirect pathways from age 4 SES (via age 5 caregiver depression), age 4 parental depression (via age 5 NA), age 4 parent support (via age 5 NA), age 4 EC (via age 5 NA), age 4 NA (via age 5 EC), and age 4 attachment security (via age 5 EC) on age 6 depression levels. Identifying the effects of early-appearing risk factors, and the pathways whereby these risk factors contribute to age 6 depression symptom levels, has important implications for our understanding of developmental psychopathology, as well as for the development of intervention and prevention programs. To fully explicate the theoretical and clinical implications of the findings revealed by Model 1, the direct and indirect effects of each of the risk factors in each domain assessed at age 4 are discussed in turn.
Contextual domain
SES
Both bootstrapping and JST indicated that a variable from the contextual domain, specifically SES at age 4, had an indirect effect on age 6 child depression via its association with increased parental depression at age 5. This is consistent with Bronfenbrenner's ecological theory that more distal, contextual factors may in part exert their effects on child outcome via factors that are more proximal to the child. That is, the present model shows that the more distal, contextual factor of SES at age 4 exerts its effects by a factor that is more proximal (i.e., caregiver depression at age 5) to the child. This is an encouraging finding because, although the structural changes required to increase families’ SES directly to decrease the risk of child depression require large-scale economic change, there are several evidence-based effective treatments for adult depression (Hollon, Reference Hollon2016), which may have a direct impact on preventing or ameliorating child depression. Furthermore, low-income individuals are at increased risk for depression (Lorant et al., Reference Lorant, Deliege, Eaton, Robert, Philippot and Ansseau2003), and these findings suggest the need for targeted programs specifically designed to address the needs of this population as they take on parental roles.
Parent domain
Caregiver depression
A factor from the parent domain, caregiver depression, had persistent effects across the preschool and school entry periods. Specifically, caregiver depression at age 4 predicted increases in age 5 caregiver depression that, in turn, predicted increases in child depression levels at age 6. Moreover, caregiver depression during preschool had an indirect effect on age 6 child depression via its effect on age 5 child NA. While a genetic relation may exist between parental depression and child NA, it is also likely that the parental emotional unavailability associated with parental depression contributes to increases in child NA because children of depressed parents do not receive the emotional validation and mirroring support that lead to feelings of positive self-worth, thereby increasing their negative affect. In addition, these children live in homes in which high levels of negative affect and negative attributions are modeled on a daily basis.
The persistent and indirect effects of caregiver depression at age 4, as well as the fact that SES exerts its effects via caregiver depression, further highlight the importance of early treatment of depressive symptoms in mothers of young children. Of course, a prerequisite for early treatment is early detection, which means that screening for caregiver depression at well-child visits during the preschool years may well be an effective strategy for early detection that also would increase the likelihood of early treatment.
Parenting domain
Contrary to expectation, the parenting factors of support, scaffolding, and hostility at age 5 did not have significant direct effects on age 6 depression symptoms. However, one dimension of parenting at age 4, supportive parenting, did have an indirect effect on age 6 child depression via its effect on age 5 child NA. That is, after correcting for a suppression effect, higher levels of supportive parenting at age 4 led to decreases in age 5 NA, which in turn led to lower levels of age 6 depression symptoms.
The lack of significant findings regarding the direct effect of parenting at age 5 does not negate the importance of the role of parenting. First, as described above, supportive parenting at age 4 did have an indirect effect via its effect on age 5 child NA. Second, the model tested included all three parenting factors simultaneously. This approach resulted in a rigorous assessment of the specific contributions of each parenting variable, reducing the shared variance between these parenting factors and assessing the contribution specific to each parenting factor to child depression. An approach that examined a “total parenting” variable or each parenting factor alone may have yielded different results, but this would capitalize on the effects of omitted variables correlated with those risk factors included in the model. In designing this study, we had hoped that a design examining the independent contributions of these different aspects of parenting might lead to a clearer picture of which aspects of parenting would be the most important to address in future prevention or intervention programs. It is noteworthy that it is difficult from these results to specify which component of parenting should be the focus of intervention. Finally, it is possible that specific aspects of parenting at earlier ages already has had an effect on child temperament at age 4 via child NA and EC. This speculation awaits further research with even younger children.
Child domain
Temperament
The reactive (NA) and regulative (EC) aspects of temperament also had persistent effects and indirect effects (based on JST) across ages 4 and 5 on child depression symptoms at age 6. Specifically, higher levels of NA at age 4 were related to increases in NA at age 5, and this increase in NA predicted higher levels of depression symptoms at age 6. Self-regulation had similar persistent effects across the preschool and kindergarten periods, such that higher levels of EC at age 4 were associated with increases in self-regulation at age 5, and this increase in age 5 self-regulation predicted lower levels of age 6 depression symptoms. This is consistent with the Muris and Ollendick (Reference Muris and Ollendick2005) model of the effects of temperament on the development of child psychopathology in which the reactive and regulatory aspects of temperament each play a role in the development of internalizing disorders.
The findings showing that two indirect paths from age 4 variables to age 6 child depression symptom levels are associated with age 5 EC, plus the fact that the magnitude of the direct effect from age 5 EC to age 6 child depression symptom levels is one of the strongest in the model. This makes it clear that self-regulation is a critically important factor associated with age 6 child depression symptoms. This suggests that interventions targeted directly at improving child EC may be important components of both primary prevention and early intervention. An evidence-based treatment for preschool depression that includes a component focused on helping the parent to support the child's emotion regulation strategies has already been developed (Luby, Lenze, & Tillman, Reference Luby, Lenze and Tillman2012). Nevertheless, further development and refinement of these types of strategies is needed as it is clear that self-regulation plays a critical role in this disorder.
The finding that SR, another aspect of child temperament, has both direct and persistent effects on age 6 child depression (according to both JST and bootstrapping results) makes a novel contribution to the literature. It is also noteworthy that the magnitude of the direct association of age 4 SR with age 5 child depression was greater than that for any other variable. Although there is evidence that SR co-occurs with internalizing disorders (Ben-Sasson et al., Reference Ben-Sasson, Carter and Briggs-Gowan2009; Gouze, Hopkins, LeBailly & Lavigne, Reference Gouze, Hopkins, LeBailly and Lavigne2009), to our knowledge, this is the first study that has examined this component of temperament as a risk factor for depression symptoms in young children. This provides further support to the argument of Gouze et al. (Reference Gouze, Lavigne, Hopkins, Bryant and LeBailly2012) that sensory regulation is a conceptually distinct aspect of temperament that warrants further examination as a risk factor for psychopathology.
In addition to the recognition that increasing attention should be focused on SR as a risk factor, the present findings also suggest that effective interventions to promote better SR might be an important adjunct in the treatment of childhood depression. To date, there are no empirically supported psychological interventions targeted at improving sensory regulation. The present findings indicate that developing such interventions would be an innovative, potentially effective, approach to treating child depression.
Attachment security
Another risk factor from the child domain, attachment security, has a significant indirect effect on age 6 child depression levels via child EC. This finding is consistent with a large body of attachment research (Sroufe, Reference Sroufe2005) showing that by preschool age, the child has developed internal working models of the attachment relationship, and that secure attachment predicts better self-regulation at later ages.
Taken together with the finding that EC at ages 4 and 5 had several direct and indirect effects on age 6 child depression, highlights the importance of this variable and the need to develop effective strategies to enhance self-regulation in young children.
The lack of significant associations between parental support, hostility, or scaffolding with age 5 EC, plus the significant association of age 4 attachment and age 5 EC suggest that critical parenting skills for improving child EC during the preschool years may involve those parenting behaviors that contribute to the development of attachment at an earlier age. These findings suggest that further exploration of the role of parenting skills in the development of child depression symptoms is warranted.
Model 2
Model 2 examined changes in depression symptoms from ages 4 to 6. It is not surprising that the strongest paths in this model are the autoregressive paths from child depression symptoms at age 4 to these symptoms at age 5, and then from child depression symptoms at age 5 to those same symptoms at age 6. When compared to the results of Model 1, the lack of significant effects in the incremental changes in depression symptoms from age 5 to 6 reflects the moderate to high level of stability for these symptoms during this developmental period. This moderate degree of stability in preschool depression is consistent with other findings (Luby, Si, et al., Reference Luby, Belden, Pautsch, Si and Spitznagel2009; Whalen et al., Reference Whalen, Sylvester and Luby2017).
Given this stability in preschool depression, Model 2 further highlights the critical role of EC that was revealed in Model 1. That is, in Model 2, EC is one of only two age 5 variables that have a significant effect on changes in depression levels across the period between preschool and school entry. Other effects on overall level of depression symptoms may have had their effect on depression levels earlier than age 5.
The critical role of EC illuminated in both models suggests that improving self-regulation is likely to be effective not only for intervention but also for primary prevention. Specifically, it suggests that attention should be focused on developing and examining the efficacy/effectiveness of strategies to enhance EC in young children. If shown to be effective, these strategies could be adapted and added to preschool social-emotional learning curricula, thereby providing a major avenue for primary prevention as well as early intervention.
It is also noteworthy that lower levels of SR significantly predicted changes in levels of depression at age 6 after accounting for earlier levels of depression. As previously mentioned, little attention has been paid to SR as a risk factor for internalizing disorders, despite evidence that difficulties in SR frequently co-occur with these disorders. Once again, the strength of these findings suggest that teaching children better sensory regulation might be a fruitful avenue for future prevention and early intervention efforts.
The present findings also suggest that interventions should be multifaceted. That is, although Model 1 revealed several significant paths to levels of child depression at age 6, none of the path coefficients were large. Thus, to be as effective as possible, treatment should include several components, and target both the child and the caregiver. Specifically, treatment components should include decreasing caregiver depression, increasing supportive parenting, and enhancing child self-regulation.
Limitations
This study also has some limitations. First, although the sample size was relatively large, it was not large enough for us to test all of the indirect paths between all of the factors at the different ages. Second, although we used direct observation whenever possible to assess a particular factor, many of the measures relied on maternal report. The young age of children precluded the use of self-report, and, as the children in the study attended over 300 different preschools, it was not feasible to collect teacher data. Third, the reliability for one of the measures, NA at age 5, was low. Nevertheless, it is questionable whether this affected the validity of that measure as multiple path coefficients were associated with NA in a manner that made psychological sense. Fourth, we did not include other types of psychopathology in the model, so it is not clear how specific these pathways are to depression. Further research is needed to determine how specific these pathways are to depression versus an externalizing disorder such as ODD or another internalizing disorder (i.e., anxiety).
Fifth and finally, although we included a wide range of factors in different domains, we also did not include other factors shown to play a role in child depression, such as social skills and peer relationships. These factors become increasingly important in later school age and adolescence, so further research is needed to elucidate the role of these factors.
Conclusions
Despite these limitations, this study contributes to our understanding of influences from variables in different domains and developmental periods that lead to both the levels of and the changes in levels of depression symptoms at early school age. The examination of these two distinct models yields several novel, theoretically important findings, such as the persistent effects of parental depression, child NA, and EC across preschool and kindergarten on age 6 depression symptoms. Second, they reveal that SR plays a role both in levels of these symptoms at age 6 and in the increase in these symptoms across developmental periods. Third, this study identified several pathways through which well-known risk factors exert their effect across these developmental stages, thereby providing information on potential points of entry for early intervention. The importance of developing public health policy targeting early prevention and intervention efforts is highlighted by these results as it is clear that the appearance of symptoms of depression at age 6 is frequently indicative of earlier clinical or subclinical levels of depressive symptoms, and also that preschool depression is the single best predictor of child depression by the time the child begins formal schooling. Fourth and finally, the study findings on EC and SR illuminate the critical importance of developing good self-regulatory abilities during the preschool period as a buffer against later depression symptoms. This suggests a promising, novel avenue for prevention and early intervention, specifically the development of strategies targeted directly at increasing the child's self-regulatory abilities.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/S0954579418001426.
Acknowledgments
This research was supported by National Institute of Mental Health Grant MH 063665, Principal Investigator John V. Lavigne. We thank the Chicago Public Schools Department of Early Childhood Education, along with participating school principals and lead teachers, and the pediatric practices in the Pediatric Practice Research Group who participated in this study.








