Adolescent mothers and their children frequently suffer from psychological, social, and economic difficulties (Jaffee, Caspi, Moffitt, Belsky, & Silva, Reference Jaffee, Caspi, Moffitt, Belsky and Silva2001). The young mothers have a higher risk for psychiatric disorders, such as postpartum depression, posttraumatic stress syndrome, substance abuse, and personality disorders than adult mothers do (Hodgkinson, Beers, Southammakosane, & Lewin, Reference Hodgkinson, Beers, Southammakosane and Lewin2014). In their own childhood, they have more often experienced adversity in the forms of neglect, physical and sexual abuse, out-of-home placement, and inconsistent parenting than have adult mothers (Garwood, Gerassi, Jonson-Reid, Plax, & Drake, Reference Garwood, Gerassi, Jonson-Reid, Plax and Drake2015). Adolescent pregnancy in industrialized countries is more common among individuals with lower socioeconomic status and poor education (Penman-Aguilar, Carter, Snead, & Kourtis, Reference Penman-Aguilar, Carter, Snead and Kourtis2013). Although adolescent mothers represent a very heterogeneous group with some mothers and their children not being exposed to the mentioned risk factors (Lee et al., Reference Lee, Gilchrist, Beadnell, Lohr, Yuan, Hartigan and Morrison2016), there is a strong association between adverse childhood experiences, adolescent pregnancy, and long-term psychosocial consequences (Hillis et al., Reference Hillis, Anda, Dube, Felitti, Marchbanks and Marks2004). Adolescent pregnancy poses a risk factor for socioeconomic disadvantage for the majority of mothers (Brannstrom, Vinnerljung, & Hjern, Reference Brannstrom, Vinnerljung and Hjern2016; Leftwich & Alves, Reference Leftwich and Alves2017; Otterblad Olausson, Haglund, Ringbäck Weitoft, & Cnattingius, Reference Otterblad Olausson, Haglund, Ringbäck Weitoft and Cnattingius2001). All of these factors contribute to inadequate mother–child interactions and less favorable child development. Previous studies have shown that adolescent mothers show less sensitivity towards the child's needs, have more instrumental and less vocal exchanges, and engage more in harsh parenting behavior than do adult mothers (Krpan, Coombs, Zinga, Steiner, & Fleming, Reference Krpan, Coombs, Zinga, Steiner and Fleming2005; Lee, Reference Lee2009). These factors are also associated with an increased risk of child neglect and maltreatment (Crittenden, Reference Crittenden1985). Maltreatment during early life has devastating long-term effects on the child's later psychosocial and cognitive development (Cicchetti & Lynch, Reference Cicchetti and Lynch1993; Perez & Widom, Reference Perez and Widom1994). Attachment insecurity and attachment disorganization are also highly prevalent among maltreated children (Cyr, Euser, Bakermans-Kranenburg, & van Ijzendoorn, Reference Cyr, Euser, Bakermans-Kranenburg and Van Ijzendoorn2010), which is associated with an increased risk for psychopathology later in life (Widom, DuMont, & Czaja, Reference Widom, DuMont and Czaja2007). Thus, children of adolescent mothers present a high-risk group for child adversity compared with children of adult mothers (D'Onofrio et al., Reference D'Onofrio, Goodnight, Van Hulle, Rodgers, Rathouz, Waldman and Lahey2009; Jaffee et al., Reference Jaffee, Caspi, Moffitt, Belsky and Silva2001). Given the high burden of adolescent parenting, countervailing the transmission of risk across generations is a major challenge for our society. Therefore, to stop this cycle of adversity, a better understanding of the underlying mechanisms of this intergenerational transmission along with effective interventions are urgently needed.
In numerous studies on parent–child interaction, sensitive parental interaction with the child (i.e., identifying the child's needs and responding adequately and promptly to them) has been identified as a protective factor for a child's development (Bakermans-Kranenburg, van IJzendoorn, & Juffer, Reference Bakermans-Kranenburg, van IJzendoorn and Juffer2003; Sroufe, Coffino, & Carlson, Reference Sroufe, Coffino and Carlson2010). Sensitive parental interaction with the infant promotes secure and stable attachment formation to the primary caregivers (De Wolff & van Ijzendoorn, Reference De Wolff and van Ijzendoorn1997; van Ijzendoorn, Juffer, & Duyvesteyn, Reference van Ijzendoorn, Juffer and Duyvesteyn1995), which supports the infant in learning to regulate emotions and behavior (Braungart-Rieker et al., Reference Braungart-Rieker, Zentall, Lickenbrock, Ekas, Oshio and Planalp2014; Mikulincer & Shaver, Reference Mikulincer and Shaver2018). Therefore, low maternal sensitivity, a key factor for the development of insecure attachments, may contribute to the transmission of adversity across generations. Recent neurobiological studies highlight the role of adversity on brain development and the stress system, and such studies also show long-term consequences on the adult's brain (Teicher, Samson, Anderson, & Ohashi, Reference Teicher, Samson, Anderson and Ohashi2016), in particular in prefrontal-limbic and reward pathways that are associated with affect regulation and are critical for parenting (Feldman, Reference Feldman2015; Lupien, McEwen, Gunnar, & Heim, Reference Lupien, McEwen, Gunnar and Heim2009). Thus, neurobiological changes brought about by early-life maltreatment might contribute to dysfunctional parenting behaviors and thus perpetuate the intergenerational cycle of abuse.
Previous international studies in high-risk families have shown that early intervention programs focusing on mother–child interaction significantly improve maternal sensitivity (Bakermans-Kranenburg et al., Reference Bakermans-Kranenburg, van IJzendoorn and Juffer2003), enhance attachment security (Letourneau et al., Reference Letourneau, Tryphonopoulos, Giesbrecht, Dennis, Bhogal and Watson2015; Mountain, Cahill, & Thorpe, Reference Mountain, Cahill and Thorpe2017), reduce attachment disorganization (Mountain et al., Reference Mountain, Cahill and Thorpe2017; Wright et al., Reference Wright, Hackney, Hughes, Barry, Glaser, Prior and McMillan2017), and reduce child maltreatment (Thomas & Zimmer-Gembeck, Reference Thomas and Zimmer-Gembeck2011). However, effect sizes are typically small (Bakermans-Kranenburg et al., Reference Bakermans-Kranenburg, van IJzendoorn and Juffer2003), suggesting heterogeneous outcomes. Furthermore, many intervention programs are not suitable for high-risk adolescent parents due to their specific needs, and adolescent mothers frequently refuse to participate in traditional programs or drop out (Chablani & Spinney, Reference Chablani and Spinney2011). Egeland and Erickson (Reference Egeland, Erickson, Kramer and Parens1993) developed a home-visiting program called Step Towards Effective and Enjoyable Parenting (STEEP, Erickson, Egeland, Simon, & Rose, Reference Erickson, Egeland, Simon and Rose2002) based on attachment theory and research from the Minnesota Longitudinal Study (Sroufe, Egeland, Carlson, & Collins, Reference Sroufe, Egeland, Carlson and Collins2005) for young mothers with a focus on maternal sensitivity to enhance attachment security. The STEEP program was evaluated in a randomized controlled trial in 154 high-risk first-time mothers, yielding inconsistent results. Although mothers in the STEEP program arm were more sensitive than were mothers in the control arm after the intervention, children's attachment security was not increased in the STEEP group compared with the control group. This has partly been explained by a ceiling effect due to an inexplicably high rate of attachment security in the control group (Erickson & Egeland, Reference Erickson and Egeland2004). More recently, this program was evaluated in 107 high-risk mother–child dyads in Germany by using a quasiexperimental design (Suess, Bohlen, Carlson, Spangler, & Frumentia Maier, Reference Suess, Bohlen, Carlson, Spangler and Frumentia Maier2016). Suess et al. (Reference Suess, Bohlen, Carlson, Spangler and Frumentia Maier2016) found a higher rate of secure attachment among children in the STEEP group compared with those in the control group when the children were 12 months of age and a lower rate of disorganized attachment in the STEEP group compared with the control group when children were 24 months of age. However, these promising results should be further elucidated in high-quality randomized controlled trials. This is particularly important because a previous systematic review(Taubner, Munder, Unger, & Wolter, Reference Taubner, Munder, Unger and Wolter2013) on the effectiveness of early prevention programs for parents with children until 3 years of age implemented in Germany could not find positive effects on maternal competencies and child development. This included eight studies with a focus on the mother–child relationship, for example, “attachment-based psychotherapeutic intervention for preterm birth” (Brisch, Bechinger, Betzler, & Heinemann, Reference Brisch, Bechinger, Betzler and Heinemann2003) or “nobody slips through the net” (Sidor, Kunz, Eickhorst, & Cierpka, Reference Sidor, Kunz, Eickhorst and Cierpka2013). Nevertheless, due to a current lack of a sufficient amount of high-quality trials in Germany, the results of this review should be verified by further studies. Thus, the objective of the Teenage Mothers–Study (TeeMo) in the framework of the German UBICA-consortium (Understanding and Breaking the Intergenerational Cycle of Abuse) was to evaluate the effects of STEEP-b, an adaptation of the original STEEP program for adolescent mothers (for further details see below), on mother–child interaction. The current study was designed as a randomized-controlled trial (RCT). In the intervention condition, high-risk adolescent mothers received the video-feedback intervention STEEP-b in addition to standard care, i.e., the usually provided health and social support by the German health care and child welfare system. The video-feedback intervention group was compared with a group of high-risk adolescent mothers who only received standard care (SC). A previous meta-analysis of attachment-based interventions (Bakermans-Kranenburg et al., Reference Bakermans-Kranenburg, van IJzendoorn and Juffer2003) revealed that sensitivity-focused interventions with a moderate number of sessions including video feedback were more effective in promoting secure attachment than complex, long-lasting interventions. Therefore, STEEP-b was designed to be relatively brief, completed in 12–18 sessions with video feedback over a 9-month period, with a focus on maternal sensitivity.
Our primary hypothesis was that maternal sensitivity (mother's ability to read and respond to the child's signals) and child responsiveness—a child's eagerness and willingness to respond to the mother (e.g., Biringen, Reference Biringen2000; Biringen, Derscheid, Vliegen, Closson, & Easterbrooks, Reference Biringen, Derscheid, Vliegen, Closson and Easterbrooks2014)—would improve from baseline to postintervention more strongly in the intervention group than in the SC group. Maternal sensitivity and child responsiveness were selected as primary outcome variables because of their specific relevance to the development of secure attachment behaviors. Further, we expected that STEEP-b would have a positive effect on child socioemotional and cognitive development and maternal well-being including maternal mental health and parental stress.
Materials and Method
Study design
The Teemo study was designed as a mono-center, randomized-controlled superiority trial (RCT) with two parallel groups. Primary endpoints were maternal sensitivity and child responsiveness after 9 months of intervention. The trial was located at the Department of Child and Adolescent Psychiatry, Psychosomatics and Psychotherapy, University Hospital RWTH Aachen, Germany. The study procedures were conducted in accordance with the declaration of Helsinki and approved by the ethical committee of the Medical Faculty of RWTH Aachen University (see for the trial protocol Firk et al., Reference Firk, Dahmen, Lehmann, Niessen, Koslowski, Rauch and Herpertz-Dahlmann2015).
Participants
Our sample consisted of adolescent mothers who were between 14 and 21 years old at the time of pregnancy with children between 3 and 6 months old who agreed to participate in the study and met the inclusion and exclusion criteria. The inclusion and exclusion criteria are listed in Table 1. All mother–child dyads received financial compensation for the assessments and travel expenses.
Table 1. Inclusion and exclusion criteria

Procedure
Mother–child dyads were recruited in cooperation with the local youth welfare system, obstetric clinics, midwife practices, and pediatrician practices in the catchment area of Aachen, Germany. Mothers who indicated an interest in participating were contacted for further screening. Those who fulfilled the inclusion criteria were visited at home to present and explain the research procedures. Mothers gave written informed consent. Infants were only included if the adolescent or adult mother and father and—in case of the adolescent mothers—the legal guardian(s) had all given informed consent. Mother–child dyads were invited to the lab to assess primary and secondary outcome measures when their children were between 3 and 6 months old before the start of the intervention (baseline, T1), after the 9-month intervention (postintervention, T2), and 6 months after the end of the intervention (follow-up, T3). Moderators of treatment outcomes and sociodemographic data were assessed at T1. Concomitant care was documented at all measurement points.
Randomization and blinding
After T1, participants were randomly assigned to either group by using a web-based randomization system (http://www.randomizer.at) in a ratio 1:1. The data entry for randomization was done by the STEEP-b trainer. The randomization tool was supervised by the Institute of Medical Biometry and Informatics of the University of Heidelberg, Germany. Block randomization using fixed block lengths was applied, stratified by mother's age (<18 years or ≥18 years). Due to the nature of the intervention neither the participants nor the STEEP-b trainers could be blinded to allocation status. However, all assessments of the outcome measures were performed by members of the research staff that were blinded to group assignment.
Intervention
The intervention (STEEP-b) is an adaptation of the STEEP program (Erickson & Egeland, Reference Erickson and Egeland2006). The STEEP program was one of the first attachment-based early intervention programs for young high-risk mothers. The main goals of STEEP are to promote secure parent–child attachment by enhancing sensitive parental care by using video-feedback techniques to reflect maternal attachment representations and their influence on parenting behavior and to enhance social support (Erickson & Egeland, Reference Erickson and Egeland2006). The STEEP-b program was adapted to be relatively brief, completed in 12–18 sessions over a 9-month period, and focused on parental sensitivity. Briefly, adolescent mothers were visited at home every 2–3 weeks by the same trainer for 9 months depending on clinical appropriateness. Video feedback from free and structured interaction situations was used to enhance maternal sensitivity. The original STEEP program was not manualized; however, as treatment manualization is considered an important factor in treatment integrity and effectiveness (Bakermans-Kranenburg et al., Reference Bakermans-Kranenburg, van IJzendoorn and Juffer2003; Weisz, Jensen-Doss, & Hawley, Reference Weisz, Jensen-Doss and Hawley2006), STEEP-b was modularized, with every session focusing on one of four modules (child development, maternal sensitivity, frightening and intrusive behaviors of the mother, and sensitive parental discipline practices). Every module was worked on twice during the intervention, with the order depending on individual appropriateness.
All of the participants (SC group and STEEP-b group) received publicly funded health care (e.g., infant health checkups, immunization) as usual in Germany and social services (e.g., social support by the German child welfare system) depending on clinical appropriateness. The SC group did not receive any intervention making use of video-feedback methods. All of the STEEP-b trainers were child and adolescent psychiatrists, psychotherapists, or qualified clinical social workers who had prior experience in psychotherapeutic interventions. To ensure that all of the trainers implemented STEEP-b, all of them were educated before the beginning of the study and their use of the modularized sessions was monitored. In addition, the trainers were supervised by an experienced STEEP therapist (G.J. Suess, STEEP training director in Germany). For the assessments of adherence and competence, the sessions were audiotaped. Participants were also asked to rate their satisfaction with the intervention on a 15-item questionnaire (including items on overall satisfaction with STEEP-b training, video-feedback, and participant-therapist alliance) by using a 5-point Likert-type scale ranging from 1 “strongly disagree” to 5 “strongly agree.”
Primary outcome measures
The primary outcome variables were maternal sensitivity and child responsiveness as change from baseline to postintervention. These variables were assessed in a standardized mother–child interaction task consisting of a 12-min free-play period (at all measurement points) and an age-appropriate stress situation (6 min at T1 and 12 min at T2 and T3), which was video-recorded for later coding. For the free-play period mothers were told to interact with their child as they normally would do in a free-play situation. For the age-appropriate stress situation, mother–child dyads participated in the still face procedure (Tronick, Als, Adamson, Wise, & Brazelton, Reference Tronick, Als, Adamson, Wise and Brazelton1978) at T1. At T2 and T3, mother–child dyads were given two boxes and mothers were instructed to have their child spend time with the toys in the boxes.
Mother–child interaction was coded using the fourth edition of the Emotional Availability (EA) Scales (Biringen, Reference Biringen2008) and the Emotional Attachment Zones Evaluation (EA-Z, Wurster, Sarche, Trucksess, Morse, & Biringen, Reference Wurster, Sarche, Trucksess, Morse and Biringen2019). The EA scales assess the emotional quality of dyadic interactions between an adult and a child. Emotional availability has been conceptualized as a research construct that was derived from attachment theory, and it is supported by the empirical literature demonstrating robust links between assessments of attachment and EA in parent–child interactions (Easterbrooks, Bureau, & Lyons-Ruth, Reference Easterbrooks, Bureau and Lyons-Ruth2012; Ziv, Aviezer, Gini, Sagi, & Koren-Karie, Reference Ziv, Aviezer, Gini, Sagi and Koren-Karie2000). For an overview on EA and EA-Z see Biringen et al. (Reference Biringen, Derscheid, Vliegen, Closson and Easterbrooks2014) or Saunders et al. (Reference Saunders, Kraus, Barone and Biringen2015).
The EA scales consist of six dimensions. The adult dimensions are sensitivity, structuring, nonintrusiveness, and nonhostility. The child dimensions are responsiveness to the adult and involvement with the adult. All of the scales range from 1 “low” to 7 “high.” The EA-Z allows researchers to globally measure the parent–child relationship, focusing on attachment-related behaviors for adult and child. The EA-Z is scored on a 100-point scale that is divided into four categorical zones: “emotionally available,” “complicated,” “detached,” and “problematic/disturbed” (Wurster, Reference Wurster, Sarche, Trucksess, Morse and Biringen2019). The EA-Z maps broadly onto the four attachment styles: secure (emotionally available), insecure-anxious (complicated), insecure-avoidant (detached), and insecure-disorganized (problematic) (Saunders et al., Reference Saunders, Kraus, Barone and Biringen2015; Wurster et al., Reference Wurster, Sarche, Trucksess, Morse and Biringen2019). The EA-Z and the EA Scales, especially maternal sensitivity and child responsiveness, are associated with measures of attachment security (Biringen, Reference Biringen, Derscheid, Vliegen, Closson and Easterbrooks2014) and therefore maternal sensitivity and child responsiveness were chosen as primary outcome variables.
The coding was done by independent raters (CF and RS) who were blinded regarding group status. The coders were trained by the developer of the method for coding EA, and they were certified as reliable on standard cases. Intraclass correlation coefficients were calculated on 37 randomly selected cases throughout the study and indicated very good inter-rater agreement for the EA scales (sensitivity: .963; structuring: .891; nonintrusiveness: .935; nonhostility: .944; child responsiveness: .946; child involvement: .894). For the EA-Z, inter-rater agreement was calculated by using Cohen's kappa (.772).
Secondary outcome measures
Secondary outcome measures for the child were social-emotional, cognitive, motor, and language development. Cognitive and motor development were assessed with the Bayley Scales of Infant and Toddler Development (BSID-III; Bayley, Reference Bayley2005), social-emotional development was assessed with the Brief Infant Toddler Social Emotional Assessment (BITSEA; Briggs-Gowan, Carter, Irwin, Wachtel, & Cicchetti, Reference Briggs-Gowan, Carter, Irwin, Wachtel and Cicchetti2004), child temperament was assessed with the Infant Behavior Questionnaire-Revised (IBQ-R; Gartstein & Rothbarth, Reference Gartstein and Rothbarth2003), and child attachment was assessed with the Strange Situation Procedure (SSP; Ainsworth & Bell, Reference Ainsworth and Bell1970). Secondary outcome measures for the mother were overall psychopathological symptoms, assessed with the Brief Symptom Inventory (BSI-18; Spitzer et al., Reference Spitzer, Hammer, Lowe, Grabe, Barnow, Rose and Franke2011); depressive symptomatology, assessed with the Beck Depression Inventory (BDI-II; Beck, Steer, Ball, & Ranieri, Reference Beck, Steer, Ball and Ranieri1996); parental stress, measured with the Parental Stress Index (PSI; Abidin, Reference Abidin1995); and child abuse potential, measured with the Child Abuse Potential Inventory (CAPI; Milner, Gold, & Wimberley, Reference Milner, Gold and Wimberley1986). Additional secondary outcome measures to assess the emotional quality of the mother–child dyad were the remaining subscales of the EA dimensions: structuring, nonintrusiveness, nonhostility, and child involvement as well as maternal EA-Z.
For a detailed characterization of the sample, at baseline (T1) mothers additionally completed assessments of intellectual functioning (Culture Fair Intelligence Test–Scale 2, Revision [CFT-20R]; Weiß, Reference Weiß2006) and psychiatric health (Mini-International Neuropsychiatric Interview [M.I.N.I]; Sheehan et al., Reference Sheehan, Lecrubier, Sheehan, Amorim, Janavs, Weiller and Dunbar1998). For psychiatric health, they also completed the Structured Clinical Interview for DSM-IV axis II personality disorders including DSM-IV criteria for conduct disorder (SCID-II; Wittchen, Zaudig, & Fydrich, Reference Wittchen, Zaudig and Fydrich1997), the State-Trait Anxiety Inventory (STAI; Spielberger, Gorssuch, Lushene, Vagg, & Jacobs, Reference Spielberger, Gorssuch, Lushene, Vagg and Jacobs1983), Conners Adult ADHD Rating Scale (CAARS; Christiansen et al., Reference Christiansen, Kis, Hirsch, Philipsen, Henneck, Panczuk and Schimmelmann2011), child abuse history (Childhood Experiences of Care Abuse Questionnaire [CECA-Q]; Kaess et al., Reference Kaess, Parzer, Mattern, Resch, Bifulco and Brunner2011), attachment history (Vulnerable Attachment Style Questionnaire [VAS]; Bifulco, Mahon, Kwon, Moran, & Jacobs, Reference Bifulco, Mahon, Kwon, Moran and Jacobs2003), Experiences in Close Relationships Scale–Revised (ECR-R; Ehrenthal, Dinger, Lamla, Funken, & Schauenburg, Reference Ehrenthal, Dinger, Lamla, Funken and Schauenburg2009), perception of parental rearing behaviors, a questionnaire measuring perceptions of parental rearing behaviors (EMBU; Perris, Jacobsson, Lindstrom, von Knorring, & Perris, Reference Perris, Jacobsson, Lindstrom, von Knorring and Perris1980), impulsivity (Barratt Impulsiveness Scale [BIS-15]; Spinella, Reference Spinella2007), emotion regulation skills (Difficulties in Emotion Regulation Scale [DERS]; Gratz & Roemer, Reference Gratz and Roemer2004), and empathic concern (Interpersonal Reactivity Index [IRI]; Paulus, Reference Paulus2009). Furthermore, sociodemographic data was collected, including standard questions on age, marital status, and educational level. Serious adverse events were documented at T2 and T3.
Statistical analysis
The intended sample size (n = 120) could not be achieved within the period of funding, so the trial was terminated before the intended sample was achieved. The current sample size of n = 56 still allows for the detection of a large effect (f = 0.4) with a power of 80% for a two-sided significance level of 5% (G-Power 3.1). All statistical analyses were performed by using IBM SPSS Statistics Version 25.0. (IBM, Armonk, New York, USA). We tested our primary hypotheses by using analysis of covariance (ANCOVA), with the EA scores at postintervention (T2) as dependent variables and the baseline values as covariates. To control for the effect of mother's age (< or ≥ 18 years at child's birth), we stratified the randomization for mother's age (< or ≥ 18 years). Further, we included the dichotomized factor maternal age (< or ≥ 18 years) as a fixed factor in a first step. However, as there was no effect of maternal age (< or ≥ 18 years) on the outcome variables, it was not included as covariate or fixed factor in the final analyses. Similarly, we compared the continuous secondary outcome variables by using ANCOVA with the respective baseline value as covariate. We calculated the p values and 95% confidence intervals (CI) based on these models. Secondary categorical outcome variables (e.g., attachment style) were analyzed by using chi-square or Fisher exact tests. Means and standard deviations or absolute and relative frequencies are reported according to the underlying scale level. The analyses of all primary and secondary endpoints were based on the modified intention-to-treat principle (Polit & Gillespie, Reference Polit and Gillespie2010), assessing each mother–child dyad with available data at T2 or T3 in the group to which they were randomly assigned irrespective of the number of intervention sessions they received. An independent data monitoring committee, reporting to an independent steering committee, oversaw the study. The trial is registered at the German Clinical Trials Register (DRKS0000440).
Results
The flow of participants from recruitment through the end of the study is shown in Figure 1. From October 2012 to December 2014, 122 mother–child dyads were screened for eligibility of whom 93 fulfilled the inclusion and exclusion criteria. Of the total, 37 were not included in the study (for reasons, see Figure 1). A total of 56 mother–child dyads were randomly allocated to treatment groups (n = 29 STEEP-b vs. n = 27 SC). Sample characteristics are presented in Table 2. In the STEEP-b group, three mothers discontinued the intervention and two mothers withdrew consent. The number of sessions of the mother–child dyads who completed the intervention ranged between 8 and 19 (mean: 12.29; SD: 3.2) sessions including 4 to 10 (mean 6.21; SD: 1.7) video-feedback sessions. Of the 29 mothers who were allocated to STEEP-b, 27 completed the postintervention assessment and 24 completed the follow-up assessment. Of the 27 mothers allocated to the control group, 20 completed the postintervention assessment and 21 completed the follow-up assessment.

Figure 1. Study flow chart.
Table 2. Sample characteristics

Note: Data are mean (SD) or n (%). Maternal IQ was measured with the Culture Fair Intelligence Test—Scale 2, Revision (CFT 20-R). Current psychiatric health was assessed with the Mini-International Neuropsychiatric Interview, (M.I.N.I), the Structured Clinical Interview for DSM-IV axis II personality disorders (SCID-II) including DSM-IV criteria for conduct disorder, and the Conners Adult ADHD Rating Scale, (CAARS). The abbreviations are as follows: STAI = The State-Trait Anxiety Inventory; CECA-Q = Childhood Experiences of Care Abuse Questionnaire; VASQ = Vulnerable Attachment Style Questionnaire; ECR-R = Experiences in Close Relationships Scale-Revised; EMBU = a questionnaire measuring perceptions of parental rearing behaviors; BIS-15, Barratt Impulsiveness Scale (2007); DERS = Difficulties in Emotion Regulation Scale; IRI = Interpersonal Reactivity Index.
Details of participants’ baseline characteristics (means and standard deviations for all primary and secondary outcome variables at T1 are presented in Table 3. The mothers had mean sensitivity scores of 3.80 (1.0), STEEP-b: 3.76 (1.0); SC: 3.85 (1.0), and their children had mean responsiveness scores of 3.82 (1.0), STEEP-b: 3.77 (0.9); SC: 3.86 (1.0). The mother–child dyads were dichotomized based on their EA sensitivity and responsiveness scores to further explore the proportion of mothers rated as sensitive, which was defined as a score of at least 5.5 (low end of neutral sensitivity) to 7 (reflecting high sensitivity), and children rated as responsive, defined as a score of at least 5.5 (low end of moderately optimal in responsiveness) to 7 (reflecting optimal in responsiveness). At baseline, only 7.3.% (STEEP-b: 6.9%, SC:7.7%) of the mothers were rated as sensitive and only 7.3% (STEEP-b: 13.8%, SC:0.0%) of the children were rated as responsive towards their mothers. There was a strong positive correlation between maternal sensitivity and child responsiveness (r = .856, p < .001), reflecting that EA dimensions are relationship variables.
Table 3. Baseline characteristics (T1)

Note: Data are mean (SD) or n (%). SC, standard care as usual; STEEP-b, intervention; BDI-II, Beck Depression Inventory; BSI-18, Brief Symptom Inventory-18; PSI, Parental Stress Index; CAPI, Child Abuse Potential Inventory; BSID-III, Bayley Scales of Infant and Toddler Development; BITSEA, Brief Infant-Toddler Social and Emotional Assessment; IBQR, Infant Behavior Questionnaire–Revised.
To assess the primary endpoints, ANCOVAs were performed with maternal sensitivity or child responsiveness at T2 as outcome variables, treatment group as a fixed factor (STEEP-b vs. SC), and baseline values as covariates. In contrast to our expectation, we did not find an intervention effect for maternal sensitivity, F (1, 44) = 0.001, p = .98, or child responsiveness, F (1, 44) = .04, p = .84, although—because of the small sample size—we only had enough power to detect a large effect. The effect size (ηp2 < .001) shows that the intervention did not result in any meaningful changes. Also, there was no improvement across time in the outcome variables in both groups (all ps > .05, Figure 2). Means, standard deviations, 95% CIs of the difference between groups, and p values are presented in Table 4. Additionally, exploratory per-protocol analyses and intention-to-treat analyses (using multiple imputation for missing data at T2) also showed no intervention effect for maternal sensitivity, per protocol: 95% CI [-0.56–0.69], p = .84; intention to treat: 95% CI [-0.67–0.50], p = .77, and child responsiveness, per protocol: 95% CI [-0.46–0.72], p = .66, intention to treat: 95% CI [-0.67–0.56], p = .85. Further subgroup analyses including only participants who received at least 12 sessions (n = 13) also revealed no intervention effect for maternal sensitivity, 95% CI [-0.17–0.62], p = .25, and child responsiveness, 95% CI [-0.24–0.47], p = .50. Finally, we explored whether the probability of improvement using the dichotomized EA sensitivity and responsiveness measure differed across treatment groups. However, no treatment effect was found for maternal sensitivity (Fisher exact test, p = .57) and child responsiveness (Fisher exact test, p = .57).

Figure 2. Maternal sensitivity and child responsiveness over time in both groups. Data are mean (SE).
Table 4. Primary outcomes: Maternal sensitivity and child responsiveness (T2, postintervention)

Note: SC, standard care as usual; STEEP-b, intervention.
To assess the secondary endpoints, ANCOVAs were performed for continuous outcomes and chi-square tests or a Fisher exact test were used for categorical outcomes. We only found an intervention effect on the parental domain scale of the PSI, 95% CI [-0.63–18.67], p = .04, showing that mothers in the STEEP-b group were less stressed than mothers in the SC group were at postintervention. However, this effect did not survive corrections for multiple comparisons. Although not correcting for multiple comparisons, no intervention effect was found for any other secondary outcome variable. Means, standard deviations, 95% CIs, and p values are presented in Table 5 (postintervention) and Table 6 (follow-up).
Table 5. Secondary outcomes (T2, postintervention)

Note: Data are mean (SD) or n (%). SC, standard care as usual; STEEP-b, intervention; BDI-II, Beck Depression Inventory; BSI-18, Brief Symptom Inventory-18; PSI, Parental Stress Index; CAPI, Child Abuse Potential Inventory; BSID-III, Bayley Scales of Infant and Toddler Development; BITSEA, Brief Infant-Toddler Social and Emotional Assessment; IBQ-R, Infant Behavior Questionnaire–Revised. Linear model adjusted for baseline value if applicable. No significant differences in EA zone distributions (Fisher exact test, p = .62), child attachment (Fisher exact test, p = .68), risk for behavior problems (χ2 = 1.50, p = .22) and risk for emotional delays (χ2 = 1.01, p =. 31) were found between groups.
Table 6. Secondary outcomes (T3, follow-up)
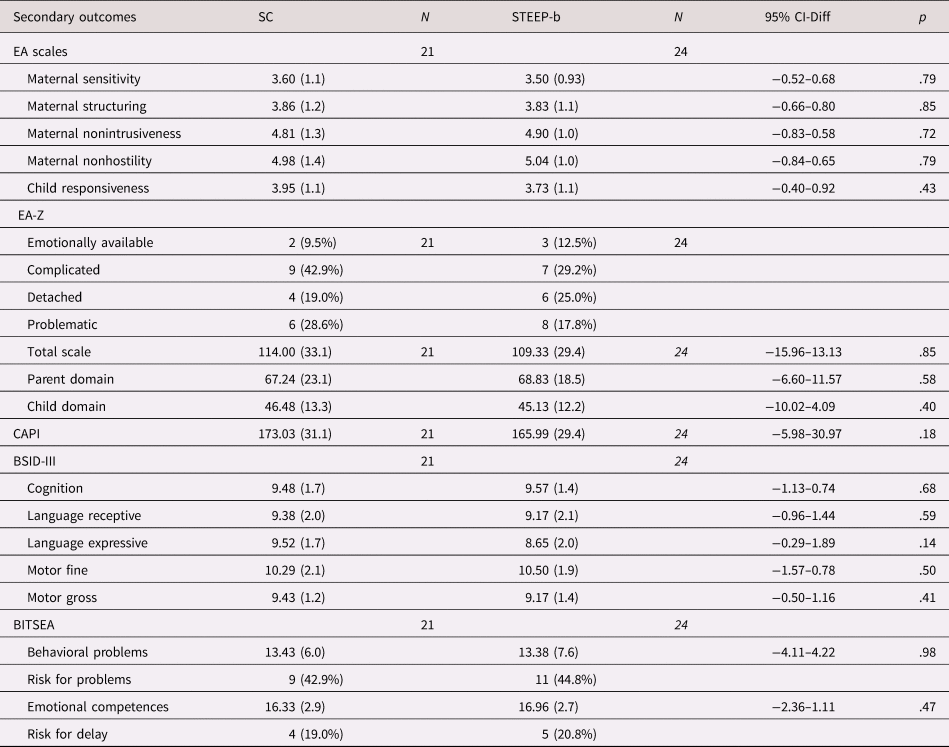
Note: Data are mean (SD) or n (%). SC, standard care as usual; STEEP-b, intervention; BDI-II, Beck Depression Inventory; BSI-18, Brief Symptom Inventory-18; PSI, Parental Stress Index; CAPI, Child Abuse Potential Inventory; BSID-III, Bayley Scales of Infant and Toddler Development; BITSEA, Brief Infant-Toddler Social and Emotional Assessment. Linear model adjusted for baseline value. No significant differences were found in EA-Z distributions between groups (Fisher exact test, p = .86). No significant differences in risk for behavior problems (χ2 = .04, p = .84) and risk for emotional delay (χ2 = 1.01, p = .31) were found between groups.
The groups did not differ with respect to the proportion of adverse events (AE, mainly hospitalization associated with infants’ infections, STEEP-b: 11 of 29, SC: 7 of 27, χ2 = .95, p = .32. There were four serious adverse events (SAEs) in the SC group (one child death and three out-of-home placements) and one out-of-home placement in the STEEP group. The difference in SAEs was not statistically significant (Fisher exact test, p = .18). No adverse events were considered related to the intervention.
Participants in the STEEP- b intervention group reported overall satisfaction with the intervention (mean: 4.7, SD: .03), 95% of the mothers would recommend the training to other mothers, and 80% reported that the training was helpful to better understand their infant's needs.
Discussion
Adolescent mother–child dyads are a high-risk population for negative child development. Although adolescent birthrates have declined in high income nations, the negative consequences of adolescent motherhood have intensified over time (Coyne, Langstrom, Lichtenstein, & D'Onofrio, Reference Coyne, Langstrom, Lichtenstein and D'Onofrio2013; Maughan & Lindelow, Reference Maughan and Lindelow1997). On the other hand, serious efforts have been made to develop effective prevention programs. Thus, there is an urgent need to study the effectiveness of these programs to improve parental child-rearing attitudes and practices, particularly in at-risk mothers.
By means of a RCT, the main purpose of the current study was to investigate the effectiveness of a 9-month home-visiting mother–child intervention program (STEEP-b) compared with SC (i.e., standard support from the child welfare system) on maternal sensitivity and child responsiveness in adolescent, high-risk mothers. Regarding demographic risk factors, the current sample of adolescent mother–child dyads is comparable to previously studied high-risk adolescent mother–child dyads (Jaffee et al., Reference Jaffee, Caspi, Moffitt, Belsky and Silva2001; Lounds, Borkowski, & Whitman, Reference Lounds, Borkowski and Whitman2006). With respect to the primary outcomes before the start of the intervention, only 7.3% of the mothers were rated as sensitive while interacting with their child and only 7.3% of their children were rated as responsive towards their mothers, which is comparable to other high-risk groups (Frigerio, Porreca, Simonelli, & Nazzari, Reference Frigerio, Porreca, Simonelli and Nazzari2019). Further, these findings are in line with previous studies showing that adolescent mothers are less sensitive and show more intrusive and hostile interactive behaviors compared with adult mothers (Krpan et al., Reference Krpan, Coombs, Zinga, Steiner and Fleming2005; Lee, Reference Lee2009; Madigan, Moran, & Pederson, Reference Madigan, Moran and Pederson2006). In contrast to our expectation, we did not find a positive effect of the current intervention on maternal sensitivity and child responsiveness, and mother–child interaction did not improve over time in both groups. Maternal sensitivity has previously been shown to be of major significance for children's attachment and social-emotional development (De Wolff & van Ijzendoorn, Reference De Wolff and van Ijzendoorn1997) and has also been associated with children's cognitive development (Mills-Koonce et al., Reference Mills-Koonce, Willoughby, Zvara, Barnett, Gustafsson, Cox and Key2015). Therefore, the reduced quality of maternal parenting behaviors in adolescent compared with adult mothers might also contribute to the influence of adolescent motherhood on offspring's negative developmental outcomes (Firk, Konrad, Herpertz-Dahlmann, Scharke, & Dahmen, Reference Firk, Konrad, Herpertz-Dahlmann, Scharke and Dahmen2018). In the current study, 30% of the children showed a disorganized attachment style in the Strange Situation Procedure at T2 and 44% scored above the cutoff for behavior problems at T2 and T3. These findings underline that there is indeed an urgent need for effective early mother–child intervention programs for high-risk adolescent mothers to enhance socioemotional development in their children.
Although behavior observations of mother–child interaction did not show a positive effect of the intervention, participants’ overall satisfaction with the intervention program was very high. These findings underline the importance of objective measures for evaluating intervention programs. Subjective satisfaction with an intervention may be influenced by dissonance reduction (to justify the personal effort mothers have put into the intervention) (Festinger, Reference Festinger1957) and a positive relationship with the trainer. Interestingly, a significant intervention effect on the parental domain scale of the parenting stress index was found, indicating lower levels of parental stress, which might be driven by an increase in social support through the intervention. Nevertheless, this effect must be interpreted cautiously, as it did not survive correction for multiple comparisons.
Of note there was a statistically nonsignificant but potentially clinically meaningful difference in the prevalence of SAEs, with four SAEs in the standard care condition and only one SAE in the STEEP-b condition. Although we do not have enough evidence to conclude that the lower rate of SAEs in the STEEP-b condition is due to the intervention, it might be driven by different intensity of surveillance of dyads in the treatment groups.
The implemented intervention (STEEP-b) is an adaptation of the STEEP program (Erickson & Egeland, Reference Erickson and Egeland2006). Recently, Suess et al. (Reference Suess, Bohlen, Carlson, Spangler and Frumentia Maier2016) showed that STEEP has a positive effect on attachment development by using a quasiexperimental design. In contrast to STEEP, which already starts prenatal and lasts up to 2 years, STEEP-b was designed to be relatively brief—based on a previous meta-analysis (Bakermans-Kranenburg et al., Reference Bakermans-Kranenburg, van IJzendoorn and Juffer2003) that concluded “less is more”—to improve compliance with the intervention and treatment effectiveness. Although previous short-term interventions employing video feedback in various populations have shown positive effects on parental sensitivity (Bakermans-Kranenburg et al., Reference Bakermans-Kranenburg, van IJzendoorn and Juffer2003), the current findings suggest that a short-term, narrowly-focused intervention program might not be sufficient to enhance positive parenting behavior and child development in high-risk adolescent mothers. Interestingly, a recent meta-analysis (Wright et al., Reference Wright, Hackney, Hughes, Barry, Glaser, Prior and McMillan2017) including only RCTs indicates that only interventions with more than 16 sessions improve attachment disorganization. This is also supported by a meta-analysis on the effectiveness of home-visiting programs showing that programs with frequent sessions (more than 3 per month) are more effective than programs with less frequent sessions (Nievar, Van Egeren, & Pollard, Reference Nievar, Van Egeren and Pollard2010), although none of these studies were performed in adolescent mother–child dyads only. Therefore, the current intervention might have been too short to change maternal parenting behaviors. Accordingly, the positive effect of another previous short-term attachment-based intervention on maternal sensitivity in families at risk for child abuse in Germany (Pillhofer et al., Reference Pillhofer, Spangler, Bovenschen, Kuenster, Gabler, Fallon and Ziegenhain2015) was no longer seen at follow-up 8–22 months later (Zwönitzer et al., Reference Zwönitzer, Ziegenhain, Bovenschen, Bressem, Pillhofer, Fegert and Künster2015).
The absence of evidence for the effectiveness of the current intervention program in high-risk adolescent mothers in Germany is also in line with recent RCTs (Barnes et al., Reference Barnes, Stuart, Allen, Petrou, Sturgess, Barlow and Elbourne2017; Robling et al., Reference Robling, Bekkers, Bell, Butler, Cannings-John, Channon and Torgerson2016) in other countries. An intervention for adolescent mothers, which has previously shown to be effective in adolescent mothers in the United States to enhance parental care (Olds, Henderson, Chamberlin, & Tatelbaum, Reference Olds, Henderson, Chamberlin and Tatelbaum1986), was not effective in the UK for reducing child maltreatment risk or enhancing parental caregiving behaviors in this high-risk group. These findings suggest that different treatment approaches may have different effects in different populations. It should be noted that in Germany as well as in the UK, adolescent mothers receiving standard care have access to many health and social services per se, which might have diluted the effect of the additional intervention program. Furthermore, a nonrandomized pilot study from Italy (Riva Crugnola, Ierardi, Albizzati, & Downing, Reference Riva Crugnola, Ierardi, Albizzati and Downing2016) with adolescent mothers and their infants suggests that to start an intervention right after the child's birth might be more effective in promoting sensitive parenting behaviors than a program starting later in the child's first year of life. In the current study, based on the results of a previous meta-analysis (Bakermans-Kranenburg et al., Reference Bakermans-Kranenburg, van IJzendoorn and Juffer2003), the intervention for most dyads started when the infants were 3–6 months of age. By this time, problematic interaction patterns may have already emerged and it might be more challenging to change inadequate maternal behaviors.
The current findings should be interpreted in light of the following limitations: First, the planned sample size could not be recruited within the time of funding, so only large treatment effects could have been detected. However, the current effect size (ηp2 < .001) supports our results and suggests that the intervention does not have a clinically relevant effect. Second, three participants who discontinued the intervention were included in the intention-to-treat analyses. However, exploratory per-protocol analyses for the primary outcome measures yielded similar findings as the intention-to-treat analyses did. Third, the coding of the mother–child interactions might not have been sensitive enough to detect subtle changes in the quality of mother–child interactions. However, the null findings are also supported by the secondary measures (e.g., child attachment, child development, maternal mental health) for which also no intervention effect was found.
In conclusion, the current randomized controlled trial does not support a narrowly focused short-term video-feedback intervention program as a means of enhancing mother–child interaction in this high-risk population of adolescent mother–child dyads. Nevertheless, the current findings support the need to develop specific early mother–child dyad interventions for young mothers, particularly given the low rates of sensitive mother–child interactions and high rates of attachment disorganization in this population. By now video-feedback methods are an accepted approach for treatment of families at risk and are increasingly implemented in several countries (Steele et al., Reference Steele, Steele, Bate, Knafo, Kinsey, Bonuck and Murphy2014). However, the idea that “less is more” as stated by Bakermans-Kranenburg and colleagues in their meta-analysis in 2003 might not be appropriate for adolescent populations with diverse psychosocial problems. High-risk adolescent mothers might need longer and more intensive interventions to improve parenting behaviors possibly in combination with more psychosocial support than other populations. Therefore, although narrowly-focused video-feedback interventions have been effective in some populations, clinical practice, theory, and research should take the differential effects of intervention programs across different populations into account.
Acknowledgments
This study was performed within the consortium of UBICA (Understanding and Breaking the Intergenerational Cycle of Abuse), a research association for investigating the influence of maternal early trauma, neglect, and abuse on child development. We acknowledge the advice of our research partners and the support of Romuald Brunner, MD, Department of Child & Adolescent Psychiatry, University of Heidelberg, Germany, who was the speaker of our consortium.
Financial support
This study was funded by the German Ministry for Research and Education (BMBF) under Grant No. 01KR1207B. The funding source (BMBF) had no role in the design of the study, data collection, data analysis, data interpretation, writing of the report, or the decision to submit for publication. The corresponding author had full access to all the data and had final responsibility for the decision to submit for publication.
Conflict of Interest
BH-D received a speaking stipend from Ferring. All other authors declare that they have no conflict of interest.










