A 2007 report by the World Health Organisation highlighted the changing landscape of pediatric health in which chronic conditions are becoming increasingly prevalent among younger age groups (Michaud, Surís, & Viner, Reference Michaud, Surís and Viner2007). The conditions are defined as conditions that cannot at present be cured but can be controlled by medication and/or other therapies and include asthma, diabetes mellitus, sickle cell disease, and chronic kidney disease (Department of Health England and Wales, 2012). Significantly, from the first recognition of the growth in prevalence of these conditions, it has been hypothesized that they may have a negative psychological impact on children and adolescents. Although chronic conditions among these age groups are generally characterized by quite mild symptomatology and minimal impairment (Newacheck & Taylor, Reference Newacheck and Taylor1992), early theorists in the field, such as Stein and Jessop (Reference Stein and Jessop1982), argued that stressors common to these conditions, such as treatment regimens and medical monitoring, place significant demands on families, increasing stress among parents and leading to overdependence in the parent–child relationship. Moreover, it was hypothesized that these illness-related demands may prevent children from engaging in social activities that would strengthen friendships and guide self-development (Stein & Jessop, Reference Stein and Jessop1982). Yet, recent theoretical articles have highlighted that these illness-related demands may have an even more detrimental impact during the adolescent years (Michaud et al., Reference Michaud, Surís and Viner2007; Sawyer, Drew, Yeo, & Britto, Reference Sawyer, Drew, Yeo and Britto2007). The adolescent period is viewed as a critical period of social development and identity formation (Michaud et al., Reference Michaud, Surís and Viner2007), with the release of pubertal hormones causing widespread changes in brain chemistry (Blakemore, Reference Blakemore2008). These neural changes not only enhance social understanding and self-awareness but also have a significant impact on the systems that control individual reactivity to rewards and danger (Blakemore, Reference Blakemore2008). In addition, increased neural susceptibility to cortisol results in adolescents reporting elevated stress levels (Nelson, Leibenluft, McClure, & Pine, Reference Nelson, Leibenluft, McClure and Pine2005). Existing research would suggest that these biopsychosocial changes may have a substantial impact on the adjustment of adolescents to their chronic illness. Studies would suggest that adolescents living with chronic illness see the demands and restrictions imposed by their treatment regimen as a barrier to this normative adolescent experimentation and separation from parents (Michaud et al., Reference Michaud, Surís and Viner2007). Stam, Hartman, Deurloo, Groothoff, and Grootenhuis (Reference Stam, Hartman, Deurloo, Groothoff and Grootenhuis2006) found delayed attainment of developmental milestones among a Dutch sample of 650 young adults who had grown up with a chronic illness when compared to their peers. Furthermore, it is hypothesized that increased social self-awareness may make adolescents more conscious of how their condition impacts on their functioning relative to their peers with qualitative data suggesting that trying to appear “normal” is a major focus in the lived accounts of children and adolescents with chronic health conditions (Taylor, Gibson, & Franck, Reference Taylor, Gibson and Franck2008). This focus on appearing “normal” may in particular lead to more negative illness cognitions in conditions in which there are physical manifestations of the chronic illness, such as stomas, scars, and insulin pumps (Michaud et al., Reference Michaud, Surís and Viner2007; Sawyer et al., Reference Sawyer, Drew, Yeo and Britto2007), or in conditions that impact on the timing of puberty (Patton & Viner, Reference Patton and Viner2007). Moreover, such aspects of these conditions may make these adolescents more at risk of experiencing victimization during this heightened period of social development. A systematic review indicated that children and adolescents with chronic illness consistently report experiencing increased levels of peer victimization when compared to their healthy peers (Sentenac et al., Reference Sentenac, Arnaud, Gavin, Molcho, Gabhainn and Godeau2012). Consequently, contemporary theories largely view chronic illness as a stressor in early development, and as an additional and acute barrier to self-esteem and social development in adolescence (e.g., Sawyer et al., Reference Sawyer, Drew, Yeo and Britto2007). As a result, given that mental illness in childhood and adolescence has largely been viewed as an outcome of predisposing and precipitating stressors (Henje Blom et al., Reference Henje Blom, Ho, Connolly, LeWinn, Sacchet, Tymofiyeva and Yang2016), the hypothesis of chronic illness as being a risk for psychopathology in young people has a strong theoretical base. However, the supporting evidence from epidemiological data in the intervening years has been somewhat varied.
There is a strong evidence base to suggest a high comorbidity between conditions with a neurological basis and psychiatric illness in youths, with studies suggesting this is largely due to the way in which such conditions impact on neural chemistry and brain structure (Brady, Deighton, & Stansfeld, Reference Brady, Deighton and & Stansfeld2017). For example, longitudinal studies have found that children and adolescents frequently demonstrate marked changes in mood and behavior in the months prior to their first epileptic seizure (Austin et al., Reference Austin, Perkins, Johnson, Fastenau, Byars and Dunn2011). However, the association between other forms of chronic illness and psychiatric illness in younger age groups is more unclear (see Brady et al., Reference Brady, Deighton and & Stansfeld2017). A national study of rates of mental illness in youths in Great Britain in 1999 indicated that children living with a physical health condition aged 5 to 15 were 82% more likely to present with a psychiatric illness when adjusted for biographic, sociodemographic, socioeconomic, and geodemographic factors (Meltzer, Gatward, Goodman, & Ford, Reference Meltzer, Gatward, Goodman and Ford2000). Yet significant variation in rates of mental illness among conditions were seen, with over 30% of children with neurological problems presenting with mental illness as compared to 13% of children with asthma and 12% of children with diabetes mellitus. These rates were just slightly over the 10% rate found for the general population. In addition, although meta-analyses in the field have consistently demonstrated small to moderate associations between chronic conditions and increased scores on psychometric measures of anxiety and depression (Bennett, Reference Bennett1994; Lavigne & Faier-Routman, Reference Lavigne and Faier-Routman1992; Pinquart & Shen, Reference Pinquart and Shen2011a, Reference Pinquart and Shen2011b, Reference Pinquart and Shen2011c), the findings highlight large amounts of variation in outcomes between conditions, and question whether increases seen among many conditions would be clinically significant (e.g., Bennett, Reference Bennett1994; Pinquart & Shen, Reference Pinquart and Shen2011a, Reference Pinquart and Shen2011b, Reference Pinquart and Shen2011c). In addition, the view that chronic conditions present common stressors to child and adolescent development has also been queried. Existing reviews highlight that the research has been mixed in demonstrating an impact of many chronic health conditions on family functioning (McClellan & Cohen, Reference McClellan and Cohen2007) and psychosocial development (Geist, Grdisa, & Otley, Reference Geist, Grdisa and Otley2003). Moreover, although evidence would suggest that, overall, children with chronic illness may be more at risk of experiencing peer victimization, this association varies widely in strength between conditions, with conditions such as asthma showing little or no impact (Sentenac et al., Reference Sentenac, Arnaud, Gavin, Molcho, Gabhainn and Godeau2012).
Overall, existing research could lead to questions about whether the impact of chronic illness on child and adolescent development and subsequent mental health outcomes may be limited to a number of conditions that present with severe, disruptive symptomatology. This is inclusive of both specific conditions with a life limiting prognosis (e.g., cystic fibrosis and epilepsy) and more severe symptom presentations within conditions overall (e.g., asthma, allergic rhinitis, and eczema). However, inconsistencies in existing findings may also be an artifact of current research methods in the field (Brady et al., Reference Brady, Deighton and & Stansfeld2017). A recent systematic review highlighted that the vast majority of research that has looked at the impact of chronic illness conditions in younger age groups has been mainly based on small, cross-sectional samples of varied ages recruited from specialist clinics (Brady et al., Reference Brady, Deighton and & Stansfeld2017). Early meta-analyses in this area warned against this practice, highlighting the large amount of bias it may introduce to assessing outcomes (Lavigne & Faier-Routman, Reference Lavigne and Faier-Routman1992). Moreover, given recent focus on how the period of adolescence may be a time of acute risk, it should be noted that small samples do not provide sufficient power to examine possible age-related variations in mental health outcomes (Williams, Holmbeck, & Greenley, Reference Williams, Holmbeck and Greenley2002). Therefore, issues of reliability and validity could be impacting on the insight currently offered by studies in the field.
Policy makers are becoming increasingly aware of the impact that mental health may have on the capacity of people to adjust to chronic illness conditions and maintain treatment regimens (Naylor et al., Reference Naylor, Parsonage, McDaid, Knapp, Fossey and Galea2012, Reference Naylor, Das, Ross, Honeyman, Thompson and Gilburt2016). However, the paucity and heterogeneity of the current research impacts on our ability to understand the relationship between chronic illness conditions and mental health in young people. Therefore, this study was designed to provide the strongest possible test of the hypothesis that children and adolescents with chronic illness are more likely to develop mental illness due to the way that these conditions disrupt the typical trajectories of development. In order to thoroughly examine the hypothesis that chronic illness is associated with higher levels of mental illness, particularly in the adolescent years, the study looked at the cross-sectional and longitudinal associations with mental illness rates for a sample of children indicated to have chronic health problems in a representative birth cohort sample from the age of 10 to 15 years. Mediation analyses were then conducted in order to isolate if factors previously implicated in theories of the impact of chronic illness on adolescent development were similarly suggested to mediate mental health outcomes in this study. As it has been suggested that chronic illness may pose as a stressor within the family, as well as a barrier to increasing independence from parents in the adolescent years, these factors included measures of family functioning—namely, conflict in the parenting relationship, parental monitoring, child disclosure, parental solicitation, and parental control. Moreover, given that there has been focus on the relationship between social development and chronic illness in the adolescent years, the mediating role of satisfaction with peer relationships was also explored. Relatedly, given that it has been suggested that children with chronic illness are at an increased risk of experiencing peer victimization, the mediating role of this variable in mental health outcomes was also explored. Finally, the mediating role of proxy markers of illness severity, specifically high degrees of absence from school and functional impairment, were also examined. These analyses were used to isolate mediating variables that were included in the creation of a pathway model in order to more rigorously explore the varying contribution of each of these variables to mental illness rates among children with chronic illness together and over time.
In order to estimate the validity and reliability of such patterns to a specific chronic illness, the study also examined how applicable the patterns found for chronic illness in general are to those seen for a subset of children living with asthma. Asthma diagnosis was selected as an exemplar for many reasons. As a reflection of the high prevalence of this condition in the general childhood population (e.g., Department of Health England and Wales, 2012), asthma was the only condition within the data set that ensured adequate analytic power for comparative purposes. Moreover, van Gent et al. (Reference van Gent, van Essen-Zandvliet, Klijn, Brackel, Kimpen and van Der Ent2008) report that the “silent” majority of children with asthma (up to 70%) are affected by mild persistent asthma, a state in which symptomatology is responsive to medical intervention, and contact with healthcare services is minimal, if not comparable to healthy peers. Consequently, comparative analyses would allow for the possibility to identify if, as suggested based on previous studies, children presenting with less impairing forms of chronic health conditions may show comparable rates of mental illness to their healthy peers. In addition, previous systematic reviews have noted that studies suggest that factors, such as socioeconomic deprivation and varied prevalence of behavioral symptomatology, distinguish the mental health outcomes seen in asthma from other chronic illness conditions (Brady et al., Reference Brady, Deighton and & Stansfeld2017). Therefore, it was considered that focusing on asthma as an exemplar would also test the assumption of theorists (e.g., Stein & Jessop, Reference Stein and Jessop1982) that factors common to all chronic health conditions predict the associated mental health impact for children and adolescents. As outlined, based on current theory in the area, it would be hypothesized that the mental health outcomes associated with asthma, and the suggested mediating variables in these outcomes, should approximate those seen for chronic illness in general.
Method
Sample
Data from this study was taken from the Avon Longitudinal Study of Parents and Children (ALSPAC), a longitudinal birth cohort study of children born in Avon county from April 1, 1991 to December 31, 1992. From birth to 18 years, there are 68 identifiable data collection points, inclusive of questionnaires completed by multiple informants, and extensive clinical assessments. A full description of the study recruitment and sample characteristics can be found in official study reports (Boyd et al., Reference Boyd, Golding, Macleod, Lawlor, Fraser, Henderson and Smith2012; Fraser et al., Reference Fraser, Macdonald-Wallis, Tilling, Boyd, Golding, Smith and Ness2013). In brief, the ALSPAC enrolled sample (aged from birth to 18 years) had an overall total of 15,247 pregnancies, 75.3% of the determined eligible sample. These pregnancies resulted in 14,775 live-born children, of which 14,701 were alive at 1 year of age. Comparative analyses of the ALSPAC sample to 1991 census data indicated that the sample had a higher socioeconomic profile than both the British average and the average for Avon County. For example, mothers in the ALSPAC sample were more likely to live in owner-occupied accommodation and have a car available to the household relative to mothers in Avon county overall. Only 2.2% of the mothers in the ALSPAC sample were indicated to be non-White, meaning that this group is highly ethnically homogenous when compared to the general British population from this period. Official attrition rates for the study throughout the childhood and adolescent period are relatively low when compared with other birth cohort studies. For example, 12,776 participants (86.9% of the 14,775 live-born children) remained officially enrolled during the adolescent phase of the study. However, these official enrollment rates mask a selective participation bias. For example, the average engagement with the 12 measures during the adolescent stage of data collection was 6,155 participants, under half (48.2%) of the official enrollment figure. Furthermore, official figures highlight that 9,600 participants (75%) responded at least once during this study phase, suggesting that the samples who engaged across data collection points were somewhat inconsistent. When looking at the age 16 comparisons of the ALSPAC sample to the national (NPD KS4 GME) sample, children who had not recently participated, or have been lost to follow-up through attrition, had a lower educational attainment than both the ALSPAC responders and the national average. Recent participants in ALSPAC at 16 years were also more likely to be female, White, and less likely to be eligible for free school meals.
Measures
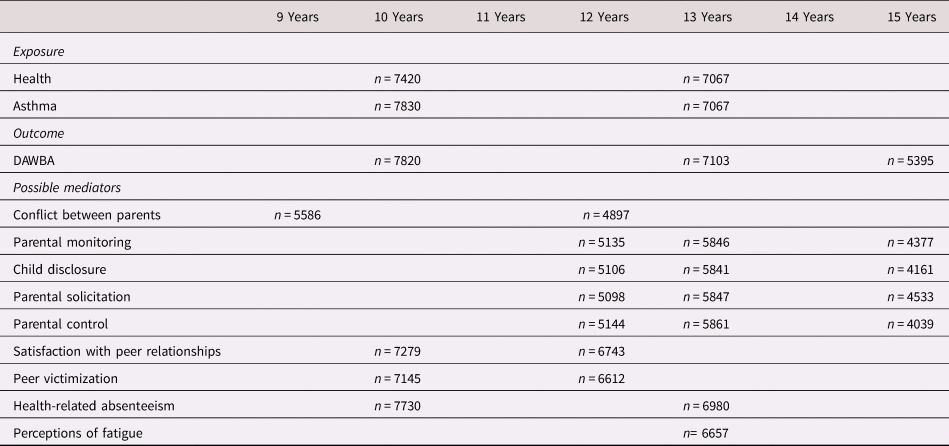
Measures were selected from the ALSPAC data set prior to the analysis. Please note that the study website contains details of all the data that is available through a fully searchable data dictionary (http://www.bris.ac.uk/alspac/researchers/data-access/data-dictionary/). An overview of the administration of all measures can be found in Table 1.
Table 1. Timeline of the administration of the mediating variable measures in relation to the administration of the exposure and outcome measures
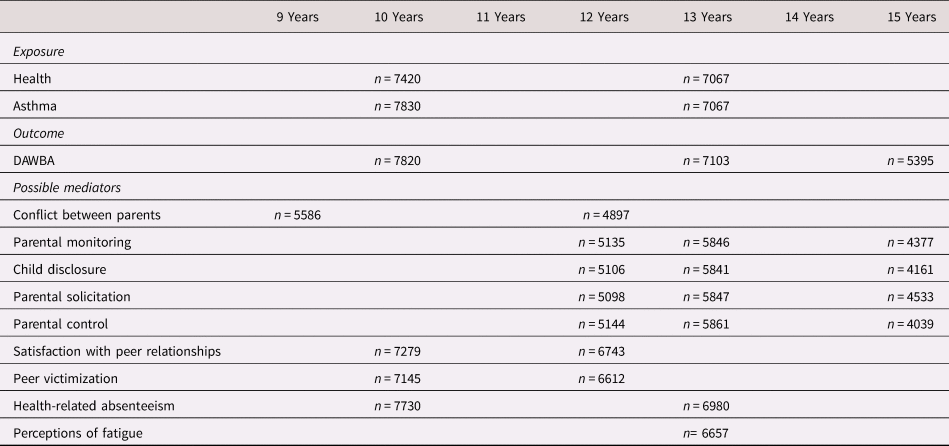
Note: DAWBA, Development and Well-Being Assessment.
Exposure
Chronic illness
The measure of chronic illness was based on maternal ratings of the child's health over the past 12 months on questionnaires administered when the child was approximately 128 months (10.67 years) and 166 months (13.83 years). A total of 7,420 of the 10,441 mothers who received this questionnaire at 128 months (71.06%) and 6,745 of the 10,390 mothers who received the questionnaire at 166 months (64.92%) provided ratings of their child's health. The mother was asked “How would you assess the health of your child within the last 12 months’” and responded, “very healthy, no problems” (128 months n = 4,588 [61.83%]; 166 months n = 4,126 [61.17%]), “healthy but a few minor problems” (128 months n = 2,703 [36.43%]; 166 months n = 2,479 [36.75%]), “sometimes quite ill” (128 months n = 114 [1.54%]; 166 months n = 109 [1.62%]), or “almost always unwell” (128 months n = 15 [0.2%]; 166 months n = 31 [0.36%]). Initial exploratory analyses indicated that these classifications showed strong consistency with other indicators of chronic physical ill health within the ALSPAC data set, such as maternal reports of illness diagnoses.
Asthma
In the 128-month child-based questionnaire, mothers were asked “Has a doctor actually said that your child has asthma or eczema.” Of the 7,810 mothers who responded (74.8% of those sent this questionnaire), 1,124 (14.39%) reported that a doctor had stated that their child has asthma, while a further 574 (7.35%) reported that a doctor had stated that their child had both asthma and eczema. In previous research using ALSPAC data, this measure of asthma was indicated to be both sensitive and specific (Cornish et al., Reference Cornish, Henderson, Boyd, Granell, Van Staa and Macleod2014). Please note this question was asked again in the 166-month questionnaire where, of the 7,067 mothers who responded (68.02% of those who received this questionnaire), 1,129 (15.98%) indicated that the doctor had confirmed that their child had asthma, and 514 (7.29%) that their child had both asthma and eczema. Reported asthma diagnosis in the 128-month questionnaire was a perfect predictor of reported asthma diagnosis in the 166-month questionnaire.
Outcome
Mental illness
The Development and Well-Being Assessment (DAWBA) is a semistructured interview, designed for epidemiological studies, which aims to generate ICD-10 and DSM-IV diagnoses (see Goodman, Ford, Richards, Gatward, & Meltzer, Reference Goodman, Ford, Richards, Gatward and Meltzer2000). The ALSPAC study team administered the DAWBA in the 128-month (10.67 year) and 166-month (13.83 year) child-based questionnaire. At 15 years, this measure was administered to adolescents and their parents in a focused measurement clinic. The prevalence of children presenting with any given psychiatric disorder at each wave were as follows: 468 (5.98% of 7,820 respondents); 393 (5.53% of 7,103 respondents); and 368 (6.82% of 5,395 respondents).
Covariates—Moderating
Gender
The ALSPAC study contains gender coding for all children who took part in the study.
Covariates—Confounding
Socioeconomic status (SES)
Chronic illness and psychiatric illness are found to be disproportionately prevalent in children and adolescents from deprived socioeconomic backgrounds (Department of Health England and Wales, 2012). The measure of SES for this study was based on reports of family income in the mother's questionnaire when the study child was approximately 134 months (11.17 years; n = 5,532). Based on reports of the UK income distribution 2016 (Department for Work and Pensions England, 2016), households where mothers recorded incomes of under £289 per week were coded as “low-income households” (n = 1,004; 19.78% of respondents). Housing tenure was the alternative measure of SES for the cross-sectional analysis of the 10.67-year questionnaire. A total of 6,228 primary caregivers meaningfully indicated their home ownership status at 122 months/10.17 years. Based on previous study classifications (e.g., Marmot, Kogevinas, & Elston, Reference Marmot, Kogevinas and Elston1987), 5,440 (87.35%) were indicated to live in owner-occupied households, 183 (2.94%) were indicated to live in privately rented accommodation, and 605 (9.71%) were indicated to live in local authority housing.
Parental history of mental illness
There are substantial hereditary factors in psychiatric illness during the childhood and adolescent years, underlined by both genetic influences and the family environment (Jaffee et al., Reference Jaffee, Moffitt, Caspi, Fombonne, Poulton and Martin2002). The measure of paternal history of mental illness was based on either the mother or the father indicating that they ever had bulimia, drug addiction, alcoholism, schizophrenia, anorexia nervosa, severe depression, or any other psychiatric disorder in either the 97-month maternal questionnaire (n = 6,130 mothers) or an early gestation paternal questionnaire (n = 8,641 fathers). The child was coded as having a parental history of mental illness if either the mother or the father indicated that they had one or more of these conditions (n = 1,776 children; 15.66%).
Mediating variables
Conflict in the parental relationship
The measure of conflict in the parental relationship was based on maternal responses in the 110-month and 145-month mother's questionnaire. The mother was provided with five conflict scenarios (mother and partner not speaking for more than an hour, mother or partner walking out of house, mother or partner shouting or calling one another names, mother or partner hitting or slapping one another, and mother or partner throwing or breaking things) and responded “Yes, I did this,” “Yes, he did this,” “Yes, we both did this,” or “No not at all” based on their recollections of the 3 months preceding the questionnaire administration. A total of 5,586 mothers responded to all five questions when the study child was 9 years and 4,897 mothers responded at 12 years. Any positive response to any of these scenarios was marked as 1 and scores across the five items were totalled (9 Years M = 0.93, SD = 1.06); 12 Years M = 0.87, SD = 1.03). Please note scale reliability coefficients were quite low at .55 across the waves.
Parental monitoring/child disclosure/parental solicitation/parental control
These four scales, designed by Stattin and Kerr (Reference Stattin and Kerr2000), were administered to the adolescents at their clinical assessments at age 12.5 years (n = 5,135; n = 5,106; n = 5,098; n = 5,144), 13.5 years (n = 5,846; n = 5,841; n = 5,847; n = 5,861), and 15.5 years (n = 4,377; n = 4,161; n = 4,533; n = 4,039). All scales were coded so that higher scores indicated higher levels of each aspect of behavior. Means and standard deviation scores for the parental monitoring scale were as follows: 12.5 Years M = 38.19, SD = 5.07; 13.5 Years M = 35.97, SD = 5.26; and 15.5 Years M = 37.45, SD = 3.82; for the child disclosure scale: 12.5 Years M = 19, SD = 3.56; 13.5 Years M = 17.87, SD = 3.52; 15.5 Years M = 19.42, SD = 2.94; for the parental solicitation scale: 12.5 Years M = 18.27, SD = 3.39; 13.5 Years M = 18.16, SD = 3.05; 15.5 Years M = 20.12, SD = 2.3; and for the parental control scale: 12.5 Years M = 19.88, SD = 3.9; 13.5 Years M = 18.56, SD = 3.83; 15.5 Years M = 20.39, SD = 3.34. Alpha coefficients mostly indicated adequate internal consistency of the scales across waves.
Satisfaction with peer relationships
ALSPAC administered the Cambridge Hormone and Moods Project Friendship Questionnaire (Singh, Winsper, Wolke, & Bryson, Reference Singh, Winsper, Wolke and Bryson2014) at clinical assessments at 10 years (n = 7,279) and 12.5 years (n = 6,743). Following the procedure of previous ALSPAC studies (e.g., Holme, Blair, & Emond, Reference Holme, Blair and Emond2013), the scale was scored in a fashion that higher scores indicated higher levels of dissatisfaction with peer relationships (Range: 1–15; 10 Years M = 2.78, SD = 1.96; 12.5 Years M = 3.05, SD = 2.06). The Cronbach α coefficient suggested fairly low internal consistency of this scale (10 Year α = .37; 12.5 Year α = .48).
Peer victimization
The ALSPAC administered the Bullying and Friendship Interview Schedule, which has been validated in studies using German and British samples (see Wolke, Woods, Stanford, & Schulz, Reference Wolke, Woods, Stanford and Schulz2001), at clinical assessments at 10 years (n = 7,145) and 12.5 years (n = 6,612). The scale demonstrated adequate levels of internal consistency at both waves. As a three-category system of classification used in previous studies (e.g., Lereya, Copeland, Costello, & Wolke, Reference Lereya, Copeland, Costello and Wolke2015) showed very little sensitivity in this sample, victimization was classified in a binary fashion with children having a score of 4 or more on the scale (range 0–27) being classified as victims of bullying (10 years n = 1,399 [19.58%]); 12.5 years n = 1,162 [17.57%]).
High degrees of school absenteeism
In the follow-up to questions regarding their children's health in the 128-month and 166-month child-based questionnaire, 7,730 mothers and 6,980 mothers, respectively, indicated the specific number of days missed from school over the past 12 months due to infections, hospital investigations, other investigations, asthma, eczema/itchy rash, hay fever/allergic rhinitis, and/or other reasons. Based on analysis of distributions of scores when days of absence were totaled, there was a strong rationale for creating a binary categorization in which a score of 6 days of more indicated a high degree of health-related school absenteeism (range 128 months: 0–79 days; range 166 months: 0–123 days). A total of 1,636 of the 7,730 children who had absenteeism-related data at 10 years (21.16%) fell into this category and 1,867 of 6,980 children (26.75%) fell into this classification at 13 years.
Functional impairment
In the 166-month self-completed questionnaire, children in the ALSPAC (n = 6,647) completed a number of questions regarding their levels of activity and fatigue in the past 3 months on a 5 point-Likert (1 = Exactly like me to 5 = Not at all like me). Interitem correlations indicated strong correlations for two set of questions. The first set of questions could be viewed as a measure of activity: the degree to which the child felt fit, the degree to which the child was very active, the degree to which the child did a lot each day, and the degree to which the child felt physically in excellent condition. The second set of questions, in contrast, could be viewed as a measure of fatigue: the degree to which the child felt in bad condition, the degree to which the child did not get much done, the degree to which the child thought he or she did not do much, and the degree to which the child did not feel like doing anything. The questions were coded so that higher scores indicated higher levels of impairment (range: 5–40; M = 18.59, SD = 5.32). The scale structure was supported by both exploratory factor analyses and principal components analysis, with Cronbach α showing a high level of internal consistency (α = .86).
Ethical approval
Ethical approval for the study was obtained from the ALSPAC Ethics and Law Committee and the Local Research Ethics Committees.
Statistical analyses
Associative analyses
The analyses for this study were guided by preliminary power analyses. These analyses aimed to identify the minimum sample sizes needed to identify a 50% increase in mental illness among children with chronic health problems (α level = .05; p = .9). This threshold was selected based on the low prevalence of mental illness indicated among the ALSPAC sample (e.g., 5.98% in the age 10 questionnaire). Given the low prevalence of mental illness among the sample, increases of below 50% would indicate quite small numbers overall, and it was believed that this may have raised concerns about the practical implications of findings. Consequently, it was considered that increases over this 50% minimum threshold would represent a real and unobscured risk to children with chronic illness within the sample. Due to limited power within the sample to examine increases in the rate of specific psychiatric disorders on the DAWBA, even when categorized into broader categories (e.g., any emotional disorder), the binary outcome of “any psychiatric disorder” was used as the primary outcome measure. Analyses of the “sometimes quite unwell” and “almost always unwell” grouping in the cross-sectional analyses were indicated to be substantially underpowered, even when these groupings were collapsed into an accumulated group. However, it was considered important to retain this grouping, given that severity of pediatric chronic illness was hypothesized to be associated with a greater risk of developing mental illness. However, substantial fluctuations in severity ratings over the 128- and 166-month questionnaires meant that it was not possible to retain such categorizations for the longitudinal analyses. The longitudinal analyses focused on children indicated to be ill at 128 months, but excluded those indicated to subsequently be healthy on the 166-month questionnaire (n = 1,303). The comparative group consisted of the 2,681 children indicated to be free from all health problems at both time waves.
Odds ratios (ORs) and 95% confidence intervals (CIs) indicative of the association between chronic illness and prevalence of psychiatric disorders were estimated using binomial logistic regression models in both the cross-sectional and longitudinal analyses. The crude association was first calculated, and adjustments were subsequently made for the covariate of gender. A third pair of models adjusted for the hypothesized impact of all three covariates, inclusive of the hypothesized confounding covariates of SES and parental history of mental illness. Likelihood ratio testing was used to examine the contribution of these adjustments to the fit of the model. Statistical significance levels were set at p < .05.
Due to the amount of missing data on the SES and parental mental health measure, all models using these measures were underpowered. There was also a proportion of missing data on the DAWBA measure of 15 years. Consequently, a final model was calculated for all analyses that adjusted for the effects of all three covariates with imputed data, created based on chained equations (MICE). Three separate imputed data sets were created for each of the cross-sectional samples, and the longitudinal sample. The chained equations contained variables shown in exploratory regression analyses to predict SES, parental mental health, and mental health at 15 years, inclusive of school attendance, and adversity during the early postnatal period. Monte Carlo estimate error terms and convergence graphs were within acceptable guidelines (methodology available on request).
All analyses were repeated for the sample of children indicated to have a doctor's diagnosis of asthma. Cross-sectional analyses were based on answers on the 128-month and 166-month questionnaires, with children indicated to be “healthy, no problems” serving as the comparative group. Longitudinal analyses were based on the answers on the 128-month questionnaire, with children indicated to be free from all health problems on both the 128-month and the 166-month questionnaire serving as the comparative group. Three separate imputed data sets were created for each of the cross-sectional samples, and the longitudinal sample to account for missing data on the measure of SES, parental mental health, and DAWBA at 15 years.
Exploratory mediation analyses
Exploratory mediation analyses were used to identify variables that were supported as mediating the association between chronic illness/asthma and the presence of psychiatric disorder. These functioned only as a guide to identify the variables to be included in the more rigorously tested path models. As these were longitudinal analyses, they were based on the longitudinal samples as described. The mediation analyses were based on the four-step method proposed by Baron and Kenny (Reference Baron and Kenny1986). In brief, this method examined whether chronic illness/asthma was associated with the mediating variable, and whether the inclusion of this variable in the associative model reduced the magnitude of the association between chronic illness/asthma and rates of psychiatric illness. These analyses were conducted in Stata 12© software.
Path models
The subsequent path model was tested for goodness of fit using MPlus© software, using the weighted least squares mean and variance estimator to account for the nonnormal distribution of the categorical variable. As the chi square test for fit of the theoretical model against the data distribution can be imprecise in the case of large samples, two additional measures of fit were also employed: the root mean square error of approximation (RMSEA) and the comparative fit index (CFI). This study used Hu and Bentler's (Reference Hu and Bentler1999) cutoff value of .95 for CFI and .06 for RMSEA for models with nonnormally distributed data. The model was also tested for goodness of fit to children identified as having an asthma diagnosis. Please note that due to the dearth of mediating measures administered in the years between the 166-month and the 15-year DAWBA measurement, the paths models explored paths to poor mental health outcomes at 10 to 13 years only.
Results
A descriptive breakdown of the cross-sectional and longitudinal samples are available in online-only Supplemental Appendix A.1. In brief, there was a small but statistically significant gender difference between the exposed and the comparative chronic illness samples, with females being slightly overrepresented in the exposed samples, and males slightly more prevalent in the comparative samples. Parents of children in the exposed samples were also statistically more likely to have reported a history of mental illness. The asthma samples reflected those of the larger chronic illness grouping, in that parents of children with asthma were statistically more likely to have reported a history of mental illness than the comparative group. However, males were slightly more prevalent among children with asthma than in the comparative group.
Associative analyses: Cross-sectional
The cross-sectional analyses looked at the association of age 128-month physical health ratings with rates of mental illness at age 10, and subsequently examined the association of the age 166-month health ratings with rates of mental illness at age 13. Compared with children who were rated as being “very healthy, no problems,” children who were rated as “very healthy, but a few minor problems” and “sometimes quite ill” or “almost always unwell” had a higher rate of mental illness at both cross-sectional waves (see Table 1). The association was indicated to be substantially stronger in children rated as “sometimes quite ill” or “almost always unwell” (128 months: “Quite healthy, but a few minor problems” OR = 1.65, 95% CI [1.28, 2.13]; “Sometimes quite ill/almost always unwell” OR = 4.32, 95% CI [2.22, 8.38]; 166 months: “Quite healthy, but a few minor problems” OR = 1.51, 95% CI [1.15, 1.99]; “Sometimes quite ill/almost always unwell” OR = 3.14, 95% CI [1.5, 6.38]). The associations strengthened slightly when adjusting for gender, which significantly improved the model fit (128 months n = 5,877; 166 months n = 5,429). However, analyses using likelihood ratio testing indicated that the addition of the confounding covariates in Model 3 (128 months n = 2,039; 166 months n = 1,511) did not significantly improve model fit over the gender-adjusted model at either time wave. This was supported by the imputed models, where ORs and 95% CIs were comparable to the gender-adjusted models.
Compared with children who were rated as being “very healthy, no problems,” children who were indicated to have been diagnosed with asthma by a doctor had a higher rate of mental illness at both cross-sectional waves (see Table 2); however, this association was just above the threshold of statistical significance at the 166-month cross-sectional wave (OR = 1.31, 95% CI [1.0, 1.73], p = .053; 128 months n = 5,546; 166 months n = 5,041). The associations weakened slightly when adjustments were made for gender, which significantly improved the fit of the models. However, analyses using likelihood ratio testing indicated that the addition of the confounding covariates in Model 3 (128 months n = 1,893; 166 months n = 1,409) did not significantly improve model fit over the gender-adjusted model at either time wave. This was supported by the imputed models, where ORs and 95% CIs were comparable to the gender-adjusted models.
Table 2. Odds ratios and 95% confidence intervals for the association of chronic illness more generally, and asthma more specifically, to rates of psychiatric illness cross-sectionally at 10 and 13 years in the complete case binomial logistic regression analyses, and model based on imputed data

Associative analyses: Longitudinal
The longitudinal analyses compared the rates of mental illness among children identified as being ill at 128 months at 10, 13, and 15 years with children indicated to be healthy at both waves. The exposed group excluded children who were indicated to have some degree of illness at 128 months, but were later indicated to be “healthy, no problems” on the 166-month questionnaire. Children indicated to be chronically ill had higher odds of presenting with mental illness at baseline (10 years; n = 3,978; OR = 1.99, 95% CI [1.51, 2.62]) and 13 years (n = 3,984; OR = 2.06, 95% CI [1.52, 2.06]; see Table 3). This association was indicated to have a slightly decreased magnitude at 15 years, even in the model based on imputed data (n = 2,643; OR = 1.62, 95% CI [1.17, 2.26]). Adjustments for gender strengthened these associations slightly at 10 and 13 years, and significantly improved the fit of these models. However, analyses using likelihood ratio testing indicated that the addition of the confounding covariates in Model 3 (10 years n = 1,124; 13 years n = 1,127; 15 years n = 765), did not significantly improve model fit over the gender-adjusted model at any time wave. This was supported by the imputed models, where ORs and 95% CIs were comparable to the gender-adjusted model (n = 3,984).
Table 3. Odds ratios and 95% confidence intervals for the association of chronic illness more generally, and asthma more specifically, to rates of psychiatric illness longitudinally at 10, 13, and 15 years in the complete case binomial logistic regression analyses, and model based on imputed data

When controlling for gender and the presence of psychiatric illness at 10 years, chronic health problems continued to be associated with an approximate 70% increased prevalence of psychiatric illness at age 13 (n = 3,978; aO = 1.73, 95% CI [1.25, 2.4]). Although chronic health problems continued to be associated with a slight increase in mental illness at 15 years after controlling for gender and the presence of psychiatric illness at 10 and 13 years, the breadth of the CIs indicated low statistical probability (n = 2,641; aOR = 1.27, 95% CI [0.89, 1.81]).
There was also an increased rate of mental illness detected among children with asthma relative to their healthy peers at baseline (10 years; n = 4,006; OR = 1.46, 95% CI [1.21, 2.12]), with this association increasing slightly at 13 years (n = 3,655; OR = 1.79, 95% CI [1.28, 2.5]) and 15 years (n = 2,505; OR = 1.72, 95% CI [0.91, 3.27]; see Table 3). The association weakened when adjusting for gender of the study child at age 10 and 13 years but strengthened again in the third and more fully adjusted model (10 years n = 1,120; 13 years n = 1,030), although the CIs indicated a lack of precision and the association fell below the level of statistical significance. In contrast, at 15 years adjusting for gender slightly strengthened the association, but this weakened in the third and more fully adjusted model (n = 728). However, analyses using likelihood ratio testing indicated that the addition of the confounding covariates in Model 3 did not significantly improve model fit over the gender-adjusted model at any time wave. In addition, adjustments for gender did not improve the model fit at 15 years. These findings were supported by analyses from imputed data (n = 4,011), where ORs in the fully adjusted model were comparable to outcomes for the gender-adjusted model at 10 and 13 years. ORs for the 15-year fully adjusted model were comparable to the imputed basic model, where ORs were slightly strengthened over the complete case analysis due to increased sample power (OR = 1.33, 95% CI [1.33, 2.59]).
When controlling for gender and the presence of psychiatric illness at previous waves, asthma continued to be associated with an approximate 60% increased prevalence of psychiatric illness at age 13 (n = 3,651; aOR = 1.62, 95% CI [1.13, 2.3]) and age 15 (n = 2,406; aOR = 1.69, 95% CI [1.18, 2.43]).
Exploratory mediation analyses
These exploratory analyses served as a basis for the selection of variables to be included in the more rigorously tested path models. A full overview of these analyses can be found in online-only Supplemental Appendix A.2. Using the Baron and Kenny (Reference Baron and Kenny1986) four-step method, the following were identified as partial mediators of the association between chronic illness and rates of psychiatric illness at 10 years: peer victimization and high school absenteeism. These same two factors were found to partially mediate associations with rates of psychiatric illness at 13 years in addition to scores on the scale measuring perceptions of fitness and fatigue. Chronic illness was also shown to predict lower levels of satisfaction with peer relationships at 12.5 years. However, these low peer satisfaction scores were not associated with mental health outcomes at 13 years. Parental monitoring, child disclosures, and parental solicitations mediated the association between chronic illness and rates of psychiatric illness at age 15 years only. Chronic health problems were associated with a lower prevalence of these aspects of parental monitoring, and these aspects of parental monitoring were, in turn, associated with a lower prevalence of psychiatric illness.
The same factors were indicated to partially mediate the association between asthma and the prevalence of mental illness at 10 and 13 years, with the exception being that, although asthma diagnosis predicted scores on the perceptions of fitness and fatigue scale, these scores did not predict the prevalence of mental illness. Asthma diagnosis also did not predict lower levels of satisfaction with peer relationships at 12.5 years, nor was asthma diagnosis statistically associated with any aspect of parental monitoring at any measurement wave.
Design of the model
The design of the pathway model was created based on a correlation matrix of the exposure, outcome, and suggested mediating variables. This matrix was based on 2,484 complete cases calculated using the nonparametric spearman's rho (see Table 4). These correlation analyses supported the findings of the mediation analysis, as well as suggesting significant associations between the mediating variables at 10 years and psychiatric illness rates at 13 years and additional associations between the mediating variables. However, in this matrix, scores on the perceptions of fitness and fatigue scale were not significantly associated with mental health outcomes at 13 years. As this contrasted with the initial mediation analyses, this mediation pathway was isolated and tested for goodness of fit using MPlus© software. As a poor fit was indicated, this variable was removed from the path model.
Table 4. Correlation matrix

Note: DAWBA, Development and Well-Being Assessment. *p < .05. **p < .01. ***p < .001.
Goodness of fit indices and model results
The path model fitted based on 3,984 observations, 2,842 (71.34%) of whom had complete data across all measures showed good fit to the data (χ2 > 0.05; RMSEA = .00, 90% CI [.00, .025]; CFI = 1.0). However, most of the resulting pathways in the fitted model were statistically nonsignificant (see Figure 1). The pathway from chronic health problems to mental health outcomes at 10 years and 13 years was nonsignificant, suggesting that the associations with psychiatric illness identified at these waves were fully mediated by the model variables. It should be noted that within this model, when controlling for all other variables, chronic illness was no longer associated with the mediating variable of peer victimization at 12.5 years. This model suggests that peer victimization was the strongest mediating factor in the association between chronic illness and mental health outcomes at age 10 years. However, when controlling for this association and its relationship to outcomes at age 13, peer victimization at 12.5 years did not independently predict mental health outcomes at 13 years in and of itself. Instead, high levels of health-related absenteeism were a consistent predictor of mental health outcomes over the two time waves. Not only did high levels of health-related absenteeism predict higher levels of health-related absenteeism within time at both 10 and 13 years, but it appeared that high levels of health-related absenteeism at 10 years were associated with mental health outcomes at 13 years, both indirectly, through the predictive pathway of high levels of health-related absenteeism at 13 years to psychiatric illness at 13 years, and directly, by leading to a slight reduction in rates of psychiatric illness at this wave. Finally, it should be noted that psychiatric illness at 10 years did not predict health-related absenteeism and peer victimization at the subsequent measurement wave.

Figure 1. Pathways predicting mental illness in children with chronic illness. Model Including standardized coefficients. **p < .05. ***p < .001.
The same model was fitted to patterns seen in the association of asthma diagnosis to rates of psychiatric illness. This model was fitted based on 4,010 observations, 2,606 of whom had complete data across all measures. All fit indices were in acceptable ranges, indicating a good fit of the model to the data (χ2 > 0.05; RMSEA = .00, 90% CI [0.00, 0.035]; CFI = 1.0). Moreover, pathways showed strong consistency with the chronic illness model (see Figure 2), with the exception that the path coefficient from school absenteeism at 10 years to psychiatric illness rates at 13 years was not statistically significant.

Figure 2. Pathways predicting mental illness in children with asthma. Model Including standardized coefficients. *p < .05. **p < .01. ***p < .001.
Discussion
This research supported current theories in the field (e.g., Michaud et al., Reference Michaud, Surís and Viner2007) by indicating an increased prevalence of mental illness among children living with mental illness from the ages of 10 to 15 years. Significantly, in spite of the broad view of adolescence as an acute period of risk, children with chronic health problems in this study were already presenting with a high prevalence of mental illness at 10 years. However, chronic health problems continued to predict incidence of mental illness at 13 and 15 years. Although the associations indicated in this study were of a higher magnitude than found in previous meta-analyses (e.g., Pinquart & Shen, Reference Pinquart and Shen2011a, Reference Pinquart and Shen2011b, Reference Pinquart and Shen2011c), they were comparable to rates found in Meltzer et al.'s (Reference Meltzer, Gatward, Goodman and Ford2000) study of children and adolescents living in the United Kingdom. For example, this study indicated that rates of mental illness, as measured by the DAWBA, were about 30% higher among children living with asthma in their cross-sectional sample, as was found in the cross-sectional analyses of this study. However, it must be noted that underlying prevalence rates of mental illness were lower in this study. For example, comparative rates of mental illness in children without any illness were approximately 3%–4% across all waves, much lower than the 10% comparative rate found in Meltzer et al.'s study (Reference Meltzer, Gatward, Goodman and Ford2000), which is in line with national population estimates (e.g., Ford, Goodman, & Melzer, Reference Ford, Goodman and Meltzer2003). This decreased prevalence of mental illness likely reflects an attrition bias in ALSPAC toward children presenting with mental illness symptomatology (Wolke et al., Reference Wolke, Waylen, Samara, Steer, Goodman, Ford and Lamberts2009). In addition, the relatively advantaged profile of the ALSPAC sample suggests a lack of sensitivity to childhood inequalities in mental health (e.g., Wickrama, Noh, & Elder, Reference Wickrama, Noh and Elder2009).
The cross-sectional analyses of this study suggested that although severity of illness symptomatology may be associated with an increased risk of mental illness, it did not wholly predict mental health outcomes. Rather, increased rates of mental illness were also identifiable among children indicated to be “healthy, but a few minor problems” over the past 12 months in both cross-sectional waves. In this sample, peer victimization and school absenteeism emerged as the strongest mediators of the mental health outcomes identified, with school absenteeism identified as the most consistent mediator of these outcomes over time. These findings are consistent with a systematic review by Sentenac et al. (Reference Sentenac, Arnaud, Gavin, Molcho, Gabhainn and Godeau2012), which suggested increased peer victimization rates among young people with chronic illness, although their findings suggested that there was not an increased prevalence of victimization among youths living with asthma. Perhaps the contrasting finding that children with asthma in this sample were also more likely than their healthy peers to be subject to peer victimization reflects the greater statistical power afforded to the mediation analyses of this study by using a larger sample. The finding that adolescents living with chronic illness may be more vulnerable to peer victimization is significant given that peer victimization in the school years has been found to have a negative association with developmental outcomes across the life span (Lereya et al., Reference Lereya, Copeland, Costello and Wolke2015). Such a finding may support a theory in the field that living with a chronic illness makes children noticeably different from peers, making them more vulnerable to teasing and intimidation (Sentanac et al., Reference Sentenac, Arnaud, Gavin, Molcho, Gabhainn and Godeau2012). It is interesting to note that peer victimization rates did not demonstrate a strong relationship with high levels of health-related school absenteeism in this study, suggesting that signifiers of the disease that do not necessarily lead to interrupted school attendance may differentiate these children from their peers.
The pathways by which high levels of health-related school absenteeism were associated with mental illness were notable. High levels of health-related school absenteeism were strongly associated with increased levels of mental illness at both time waves. However, the pathways suggested that children with chronic illness who had a high degree of health-related absenteeism at 10 years, but returned to normative levels of attendance in the following years, had a decreased risk of experiencing mental illness at 13 years. This finding emphasizes school absenteeism as more than a proxy measure of symptom severity, and this is further highlighted by the finding that scores on a scale measuring perceptions of fitness and fatigue did not seem to mediate mental health outcomes. Weitzman (Reference Weitzman1986) previously argued that school absenteeism is a key aspect of the experience of chronic illness but equally acknowledged that, in many ways, it is a very nonspecific factor to examine. For example, school-related absenteeism has been discussed as an indicator of disease activity and symptom control (e.g., Kearney, Reference Kearney2008), meaning that the increased rate of mental illness seen among those experiencing high levels of health-related school absenteeism may be attributed to aspects of the physical illness. However, school absenteeism in the context of chronic illness has also been discussed as a signifier of disruptions to social development and academic attainment (Eiser, Reference Eiser1993), meaning that the increased rate may also be attributable to the ways in which chronic health conditions impact on the normative experience of school and friendships. However, satisfaction with peer relationships did not have a strong relationship with mental health outcomes in this study, suggesting that the impact was also more than just social in nature. In addition, it should be acknowledged that it has been found that mental illness can lead to poorer treatment adherence and symptom exacerbation in chronic health conditions (Department of Health England and Wales, 2012). Consequently, it is possible that the increased levels of health-related school absenteeism observed may be due to the impact of mental illness on the child's physical health. Therefore, although this study suggests that health-related school absenteeism may be a key factor in identifying children with chronic illness who may be at risk of experiencing mental illness, further investigation would be needed to explore the nuances of this relationship.
There were limitations to the scope of this study that should be noted. Although the measure of chronic illness for this study was selected with the guidelines of international public health bodies in mind, a proportion of children indicated to have chronic illness diagnoses, such as asthma, were not identified. Initial exploratory analyses would suggest that the measure of chronic illness was more sensitive to children experiencing more severe symptoms of illness. Therefore, given the indications of previous studies, and the findings of the comparative analyses of adolescents diagnosed with asthma, it is hypothesized that the associations identified in the study are robust, but that the magnitude may vary depending on illness characteristics. A further artifact of the choice of measure of chronic illness should be noted. As the longitudinal associative analyses excluded children who were ill at 128 months but not in the 166-month questionnaire in order to ensure the measure was reflective of those with chronic health problems, the longitudinal nature of the association of chronic ill health at 10 years to mental health outcomes at 13 years was compromised. Furthermore, it was not possible to maintain this consistency with an exclusion of children indicated to be healthy at 15 years, compromising the reliability of the associative analyses and perhaps underlying the weaker associations found at this later wave.
The study was substantially impacted by characteristics of the ALSPAC data collection. As discussed, the ALSPAC sample, particularly during the years of adolescence, shows a bias to families from higher socioeconomic and White backgrounds. This was likely reflected in the low rates of mental illness in the overall sample, and the lack of mediating role indicated for SES. Consequently, although peer victimization and high levels of health-related absenteeism play the most substantial mediating role in mental health outcomes for the ALSPAC sample, it is possible that different, or additional, outcomes of chronic health problems may be identified as playing a more pivotal mediating role in more heterogeneous population groups. The timeline for the study was determined by a lack of consistency in the ALSPAC measures in middle to late adolescence, as questionnaires were shortened to improve response rates (see Boyd et al., Reference Boyd, Golding, Macleod, Lawlor, Fraser, Henderson and Smith2012). In addition, a lack of consistent measurement of many variables, such as peer victimization and school absenteeism, in the period from 13 to 15 years limited the mediation analyses and constrained the scope of the study. For example, the exploratory mediation analyses, although crude, indicated a role of parental monitoring in mental health outcomes at age 15 years, but not at 10 and 13 years. This provided some suggestion of a changing nature of the factors mediating the association of chronic health problems to mental illness over the adolescent period, but there was limited opportunity to reliably explore this in this sample. In addition, the study was constrained to the measures administered. As a result, a number of the scales used were novel to this study (e.g., the perceptions of fitness and fatigue scale) and a minority indicated weak psychometric properties (e.g., Cambridge Hormone and Moods Project Friendship Questionnaire).
Finally, the low rates of mental illness in the ALSPAC data set meant that it was not possible to use rates of specific psychiatric disorders as the outcome measure. Initial exploratory analyses would suggest that the magnitude of the association may change in middle adolescence, with rates of mental illness becoming increasing characterized by emotional rather than behavioral or anxiety symptomatology (see Appendix S.1). However, using a larger sample with a higher prevalence of such conditions would be required to give a more thorough and reliable picture of relationships in the data.
Yet, there were also notable strengths to this study. A lack of longitudinal research focusing on children and adolescents living with chronic health problems has been repeatedly highlighted in the literature (e.g., Brady et al., Reference Brady, Deighton and & Stansfeld2017; Sawyer et al., Reference Sawyer, Drew, Yeo and Britto2007). This research is bolstered by the use of longitudinal data collected from a large and representative sample of young people and the supportive findings from imputed data. Therefore, the methodology of this study overcomes many of the limitations associated with the small samples of previous investigations. Moreover, this study aimed to support hypotheses made in this field, not only by exploring the nature of the association between chronic illness and mental illness in children as they enter adolescence, but also by exploring the pathways by which chronic illness leads to increased rates of mental illness. The findings of this study were greatly supported by comparative analyses of a subsample of children living with asthma, suggesting that there may be some common mediating risk factors to mental health across chronic illness conditions. Significantly the findings of this study support the positions of many in the field (e.g., Michaud et al., Reference Michaud, Surís and Viner2007; Stein & Jessop, Reference Stein and Jessop1982) by highlighting that the impact of chronic illness goes beyond medical regimens. Rather the findings of this study highlight the impact of chronic illness on development as children enter adolescence, even so far as to impact on children's social relationships and experiences of school.
In the Department of Health England and Wales (2012) report outlining policy planning for the treatment of people with chronic illness, children and adolescents are given relatively limited focus when compared to their adult counterparts. However, in a reflection of international models, it was highlighted that a priority within the health services in the United Kingdom at this time was to ensure a more substantial presence of Child and Adolescent Mental Health Services (CAMHS) in pediatric chronic illness teams. Although this study has supported the view that mental health provisions are needed in the context of children and adolescents with chronic illness, it is still believed that these stated policy plans are short-sighted. The CAMHS service is designed to intervene on cases of moderate to severe psychopathology in children and adolescents, providing intense treatment interventions mostly within healthcare settings (see NHS England, 2014). This study has suggested that the disruptions to daily lifestyles as a consequence of chronic illness, such as higher than normative levels of school absenteeism, may be among the factors leading to mental ill health among these adolescents. Although the findings of this study need further external validation in more heterogeneous samples and older adolescent populations, it is important to highlight that it shows many parallels with qualitative accounts of the lived experience of chronic illness (e.g., Taylor et al., Reference Taylor, Gibson and Franck2008), where being respected and treated like peers within the school context is a highlighted desire of young people living with chronic illness.
In conclusion, this study suggests that chronic illness is associated with an increased rate of mental illness in late childhood and early adolescence and suggests that these increased rates are mediated by school attendance and the child's relationship with peers. The findings suggest that examining school absenteeism rates, as well as rates of peer victimization, may be key to identifying adolescents with chronic illness at risk of developing mental illness. The emergence of these factors as key mediating variables highlights the importance of an age-specific focus when considering the impact of chronic illness on the individual more generally. As Sawyer et al. (Reference Sawyer, Drew, Yeo and Britto2007) argue, longitudinal research is needed to help us to understand the impact of chronic health conditions on developmental outcomes across the childhood and adolescent period and associated mental health. Given the rise in such conditions internationally, it is hoped that this research stands as an insight into the impact of chronic illness in the period of early adolescence in a relatively large population sample.
Supplementary Material
The supplementary material for this article can be found at https://doi.org/10.1017/S0954579420000206.
Acknowledgments
The authors would like to extend their gratitude to all the families who took part in this study, and the whole ALSPAC team.
Financial support
This work was supported by the National Institute of Health Research (NIHR) Collaboration for Leadership in Applied Health Research and Care (CLAHRC) North Thames at Bart's Health NHS Trust. The views expressed are those of the authors and not necessarily those of the NHS, the NIHR, or the Department of Health. The UK Medical Research Council and Wellcome (Grant ref: 102215/2/13/2) and the University of Bristol provide core support for ALSPAC. This publication is the work of the authors, who will serve as guarantors for the contents of this paper.