Introduction
Schizophrenia is still too often a highly disabling condition, often requiring intense treatment and employment of a broad range of pharmacological treatment options, due to the heterogeneous clinical manifestations of the disorder.Reference Miyamoto, Miyake and Jarskog1, Reference Kahn, Sommer and Murray2
Despite multiple treatment trials and the availability of clozapine,Reference Breier, Buchanan and Kirkpatrick3 a considerable percentage of patients will have an unsatisfactory outcome,Reference Carbon and Correll4 especially when residual cognitive and/or negative symptoms persist.Reference Buckley, Miller and Olsen5, Reference Carbon and Correll6 Thus, there is a need to diversify the pharmacological approach even before treatment resistance to clozapine and/or chronicity of schizophrenia occurs.Reference Meltzer7
Although clozapine still has the best evidence for efficacy in treatment-resistant schizophrenia,Reference Samara, Dold and Gianatsi8–Reference Kane and Correll10 multiple pharmacologic augmentation and combination therapies have been tried with varying degrees of success. While some of these strategies seemed to be superior to placebo according to a recent review of the meta-analytic evidence, none had sufficient high-quality evidence in the studies analyzed to warrant clinical recommendation for unselected schizophrenia patients.Reference Correll, Rubio and Inczedy-Farkas11
The potential efficacy of dopamine agonist medications, such as atomoxetine or psychostimulants, has been postulated, especially for negative symptoms and cognitive dysfunctionReference Lindenmayer, Nasrallah and Pucci12 or for countering antipsychotic-related lassitude and fatigue.Reference Sommer, Begemann, Temmerman and Leucht13 Moreover studies of adjunctive treatment of lisdexamfetamine—an amphetamine product that recently received US Food and Drug Administration approval for treatment of moderate-to-severe binge-eating disorder in addition to attention-deficit/hyperactivity disorder (ADHD) in adultsReference Fornaro, Solmi and Perna14—documented significant improvement in all assessed negative symptoms and attention in schizophrenia outpatients.Reference Lasser, Dirks and Nasrallah15 However, fear of potential harms due to exacerbation of positive symptoms or relapse also exist, and the “sensitization/kindling” theory has called for caution even against low-dose and short-term use of psychostimulants in individuals at risk for or with manifest psychosis.Reference Curran, Byrappa and McBride16
Unsurprisingly, controlled studies primarily assessing the efficacy of atomoxetine or psychostimulants in the treatment of schizophrenia with prominent positive symptoms are virtually absent, as tolerability issues pose major concerns, limiting the practical and ethical feasibility of such investigations, except for challenge tests to experimentally induce psychosis in imaging paradigms.Reference Strakowski, Sax and Setters17, Reference O’Daly, Joyce and Stephan18 Whenever available, data about the effects of adjunctive atomoxetine or psychostimulants for schizophrenia on positive symptoms essentially represent secondary outcome measures from studies focusing on negative or cognitive symptom management.
In two reviews of old and heterogeneous studies of psychostimulant provocation studies in schizophrenia patients, “overall response” patterns after psychostimulant challenge were summarized. In one review of 11 provocation studies, 37.2% of patients improved and 62.8% showed no change or worsening. In the second review of 36 provocation studies, 17.5% improved, 41.5% showed no change, and 41.1% worsened.Reference Lieberman, Kane and Sarantakos19 However, “response” was not assessed in a detailed way, and almost all of the studies were open-label trials, limiting the value of these observations. Referring to these two reviews, a systematic review published in 2013 examined more recent data regarding the effects of methylphenidate, amphetamines, modafininil, and armodafinil in challenge test designs or in treatment studies for negative symptoms or cognition in patients with schizophrenia. In that more recent, narrative review, data from only one treatment study with methylphenidate and from six treatment studies with amphetamines were summarized. Again, data were difficult to interpret, as only four of the seven studies were randomized and placebo controlled, and outcomes varied.Reference Lindenmayer, Nasrallah and Pucci12
Further issues that are relevant in the consideration of long-term psychostimulant exposure are the potential for development of tolerance, as well as the chance of rebound following abrupt discontinuation, and supersensitivity psychosis, though the corresponding literature in schizophrenia cases is scarce and inconclusive compared with non-schizophrenia samples.Reference Fallon, Dursun and Deakin20–Reference Leduc and Mittleman22 In this context, potentially relevant moderators of safety during the use of psychostimulants in schizophrenia include clinical stability of non–acute phase patients reliably receiving antipsychotic medications and presenting with minimal psychotic symptoms, as well as absent history of stimulant (ab)use, including cocaine and other illicit drugs, or no history of cardiovascular disease.Reference Lindenmayer, Nasrallah and Pucci12
Due to the scarcity of data and conflicting results of individual studies, the primary aim of this systematic review was to provide an updated synthesis of randomized, placebo-controlled, double-blind evidence regarding the efficacy and safety of psychostimulants or atomoxetine, an ADHD treatment that also increases dopaminergic transmission,Reference Koda, Ago and Cong23 in patients with schizophrenia or schizoaffective disorder. As a secondary aim, we systematically summarized results from studies that administered stimulants in a provocation or challenge design in order to test their immediate effects on positive symptoms and potential roles as predictors of psychotic symptom exacerbation/relapses in the longer term.
Methods
The present systematic review adhered to the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) statement,Reference Moher, Liberati and Tetzlaff24 following a predetermined, unpublished protocol.
Search strategy
An electronic literature search was conducted across PubMed, SCOPUS, and Clinicaltrials.gov for results indexed after 1980 until 17 January 2017 by two independent reviewers (MS, KT), using the following search terms: (“schizophrenia”[MeSH Terms] OR “schizophrenia”[All Fields] OR “schizoaffective”[All Fields] OR “schizophreniform”[All Fields]) AND (“stimulant”[All Fields] OR “stimulants”[All Fields] OR “lisdexamfetamine”[All Fields] OR “lisdexamphetamine”[All Fields] OR “atomoxetine”[All Fields] OR “dexamphetamine”[All Fields] OR “methylphenidate”[All Fields] OR “dextroamphetamine”[All Fields] OR “amphetamine”[All Fields] OR “psychostimulant*”[All Fields]) AND (“randomized” OR “RCT” OR “trial” OR “randomized-controlled”) to identify randomized controlled trials (RCTs) investigating the efficacy and safety of stimulants as an augmentation strategy in patients diagnosed with schizophrenia or schizoaffective disorder. References of included or relevant studies were hand-searched for potential additional trials.
Inclusion and exclusion criteria
Studies eligible for the meta-analysis were double-blind, placebo-controlled, randomized trials (DBPCRCTs) that (1) included patients diagnosed with schizophrenia or schizoaffective disorder, defined by standardized criteria; (2) compared atomoxetine, amphetamine derivatives, or methylphenidate with placebo; and (3) reported efficacy, cognition, or safety results using a standardized rating scale or test (allowing for spontaneous reporting for adverse effects); or (4) measured any putative serum or neural mediators of the biological activity of psychostimulants or atomoxetine in patients with schizophrenia.
Studies were excluded if they reported on different medications, did not include a placebo control group, or included patients with a primary diagnosis other than schizophrenia or schizoaffective disorder.
Outcomes
Efficacy and tolerability outcomes were divided into changes in positive symptoms, negative symptoms, mood, or cognitive functions, as well as extrapyramidal side effects, cardiovascular safety, and other tolerability outcomes. Biological mechanism outcomes were divided into relapse prediction and other results of studies with a provocation test design, as well as results describing the role of putative endocrine or neural markers of the effects of psychostimulants or atomoxetine in patients with schizophrenia.
Data extraction
Two reviewers (MS, TK) independently extracted data from the included studies into a standardized Microsoft Excel spreadsheet. Any disagreement was resolved by consensus. The following information was extracted: author(s), year, country, study design, inclusion and exclusion criteria, trial duration, setting, sample size, population demographics, psychostimulant drug/atomoxetine and dosage, other medications and dosages, outcome measurement tools, and results for each a priori determined outcome.
Quality assessment
Additionally, evaluation of methodological study quality was conducted by two independent reviewers (MS, TK) using the Cochrane Collaboration’s tool for assessing risk of bias.Reference Higgins, Altman and Gotzsche25 The tool includes six domains that can indicate low, unclear, or high risk of bias. Considering the six domains, a study is defined as having low risk of bias when all domains indicate low risk of bias, unclear risk of bias when one or more domains indicate unclear risk of bias, high risk of bias when high risk of bias is present for one or more key domains.
Data extraction and exploratory meta-analysis
Data were extracted and entered into a standardized Microsoft Excel spreadsheet by two authors independently (MS, KT). We extracted the following variables: author(s), year, design of the study, aim of the study, sample size, investigated drug, rating scales used, change or endpoint values, and descriptive primary and secondary results of included studies.
A random-effects exploratory meta-analysis was performed with Review Manager, Version 5.2 (RevMan; Nordic Cochrane Centre, Copenhagen) for each psychopathological or cognitive domain for which meta-analyzable data were reported in at least two studies for either methylphenidate, d-amphetamine, or atomoxetine versus placebo. We analyzed change values of symptom rating scales at endpoint, and when change values were not available, we used endpoint values, given that standard deviations was not more than two times the mean. Data were pooled according to drug (amphetamines, atomoxetine, methylphenidate) subgroups.
Results
Search results, studies included, and population
The study-selection flow is described in Figure 1. Out of 1008 initial hits, 922 were excluded through title/abstract reading. Altogether, 86 full texts were reviewed, and 64 were excluded with no DBRT placebo-controlled duplicates, no schizophrenia, and no different drugs. (see Figure 1). A total of 22 studies that reported data on 422 patients randomized to psychostimulants or atomoxetine and 222 randomized to placebo were included in this systematic review (Table 1). Eight studies included patients with schizophrenia only,Reference Swerdlow, Tarasenko and Bhakta26–Reference Martin, Dirks and Gertsik33 and 14 studies included patients with schizophrenia or schizoaffective disorder.Reference Lieberman, Kane and Sarantakos19, Reference Kelly, Buchanan and Boggs34–Reference Barch and Carter46
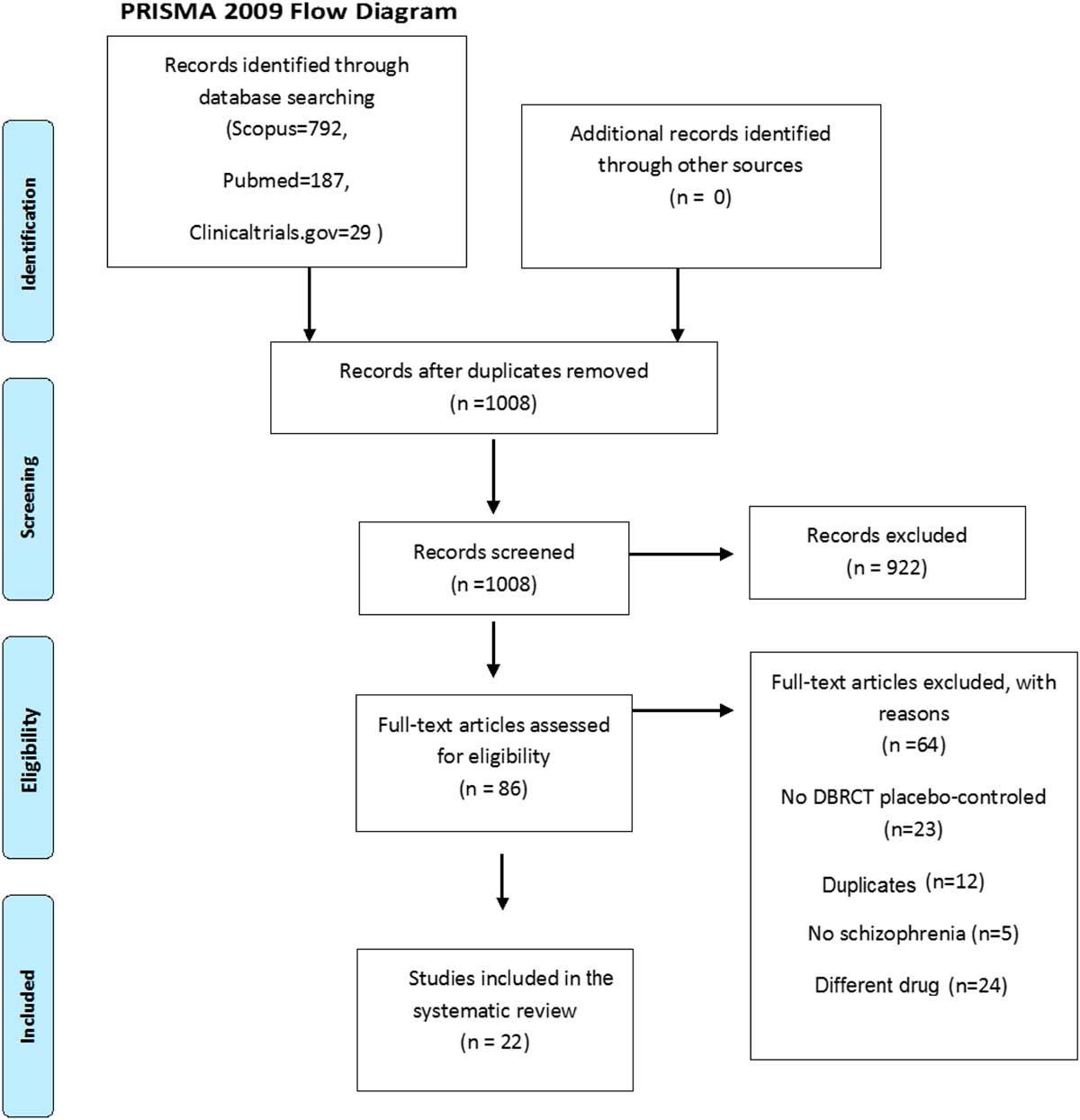
Figure 1 PRISMA study selection flowchart.
Table 1 Descriptive characteristics of included studies

AIMS=Abnormal Involuntary Movement Scale; AIRS=Amphetamine Interview Rating Scale; BACS=Brief Assessment of Cognition in Schizophrenia; BAS=Barnes Akathisia Scale; BPRS=Brief Psychiatric Rating Scale; CDSS=Calgary Depression Scale for Schizophrenia; CGI=Clinical Global Impression; C-SSRS=Columbia-Suicide Severity Rating Scale; COWAT=Controlled Oral Word Association Test; DBRCT=double-blind randomized controlled trial; DSM-III=Diagnostic and Statistical Manual of Mental Disorder, 3rd ed. DSM-IV=Diagnostic and Statistical Manual of Mental Disorders, 4th ed. fMRI=functional magnetic resonance imaging; GH=growth hormone; HVA=homovanillic acid; NA=not available; IP=inpatients; NOSIE=Nurses’ Observation Scale for Inpatient Evaluation; OP=outpatients; PANSS=Positive and Negative Syndrome Scale; POMS=Profile of Mood State; PSAS=Psychiatric Symptom Assessment Scale; RBANS=Repeatable Battery for Assessment of Neuropsychological Status; RDC=Research Diagnostic Criteria; SADS-PD=Schedule for Affective Disorders and Schizophrenia—Psychosis and Disorganization; SANS=Scale for the Assessment of Negative Symptoms; SAS=Simpson Angus Scale; SEC=Side Effect Checklist; SDS=Simpson Dyskinesia Scale; SLOF=Specific Level of Function Scale; TCT=targeted cognitive training; T&A=Taylor and Abrams Scale for Emotional Blunting; WCST=Wisconsin Card Sorting Test.
All but two studies were rated as having a high risk of bias (Table 2); in particular, a high risk of bias was evident from the lack of an adequate random sequence generation method or an adequate allocation concealment procedure.
Table 2 Narrative review of efficacy, safety and biological effects of atomoxetine, amphetamines, and methylphenidate

AIMS=Abnormal Involuntary Movement Scale; AIRS=Amphetamine Interview Rating Scale; BACS=Brief Assessment of Cognition in Schizophrenia; BAS=Barnes Akathisia Scale; BP=blood pressure; BPRS=Brief Psychiatric Rating Scale; CDSS=Calgary Depression Scale for Schizophrenia; CGI=Clinical Global Impression; C-SSRS=Columbia-Suicide Severity Rating Scale; COWAT=Controlled Oral Word Association Test; DBRCT=double-blind randomized controlled trial; fMRI=functional magnetic resonance imaging; GH=growth hormone; HR=heart rate; HVA=homovanillic acid; NA=not available; NOSIE=Nurses’ Observation Scale for Inpatient Evaluation; PANSS=Positive and Negative Syndrome Scale; POMS=Profile of Mood State; PSAS=Psychiatric Symptom Assessment Scale; RBANS=Repeatable Battery for Assessment of Neuropsychological Status; RDC=Research Diagnostic Criteria; SADS-PD=Schedule for Affective Disorders and Schizophrenia—Psychosis and Disorganization; SANS=Scale for the Assessment of Negative Symptoms; SAS=Simpson Angus Scale; SEC=Side Effect Checklist; SDS=Simpson Dyskinesia Scale; SLOF=Specific Level of Function Scale; TCT=targeted cognitive training; T&A=Taylor and Abrams Scale for Emotional Blunting; WCST=Wisconsin Card Sorting Test.
Therapeutic interventional studies
Studies included, treatments, and participants
Four trials investigated the therapeutic effects of atomoxetine (n=50 received atomoxetine, n=48 control),Reference Friedman, Carpenter and Lu31, Reference Sacco, Creeden and Reutenauer32, Reference Kelly, Buchanan and Boggs34, Reference Ball, Warren and Feldman38 nine of amphetamine, dextroamphetamine, or lisdexamfetamine (n=218 stimulants, n=98 control),Reference Swerdlow, Tarasenko and Bhakta26–Reference Sanfilipo, Wolkin and Angrist30, Reference Martin, Dirks and Gertsik33, Reference Van Kammen, Bunney and Docherty35, Reference Van Kammen and Boronow39, Reference Barch and Carter46 and one of methylphenidate (n=8 received stimulant, n=8 control) (Table 1).Reference Carpenter, Winsberg and Camus36
Efficacy: positive symptoms
Effects on positive symptoms of atomoxetine,Reference Friedman, Carpenter and Lu31, Reference Sacco, Creeden and Reutenauer32, Reference Kelly, Buchanan and Boggs34 d-amphetamine,Reference Goldberg, Bigelow and Weinberger27–Reference Sanfilipo, Wolkin and Angrist30, Reference Martin, Dirks and Gertsik33, Reference Van Kammen, Bunney and Docherty35, Reference Van Kammen and Boronow39, Reference Barch and Carter46 or methylphenidateReference Carpenter, Winsberg and Camus36 were assessed in three, eight, and one studies, respectively (Table 3).
Table 3 Cochrane Collaboration’s tool for assessing risk of bias in included studies

High=high risk of bias; Low=low risk of bias; Unclear=unclear risk of bias.
Narrative review
No study reported significant improvement in positive symptoms with atomoxetine compared with placebo. Mixed evidence included no effect of d-amphetamine on positive symptoms in three studies,Reference Goldberg, Bigelow and Weinberger27, Reference Pietrzak, Snyder and Maruff28, Reference Barch and Carter46 while three other studies suggested worsening of positive symptoms.Reference Sanfilipo, Wolkin and Angrist30, Reference Van Kammen, Bunney and Docherty35, Reference Van Kammen and Boronow39 Two studies did not report the results of comparison between d-amphetamine and placebo, describing small benefits from baseline in oneReference Martin, Dirks and Gertsik33 and improvement of positive symptomatology in roughly one-third of patients in another.Reference Daniel, Weinberger and Jones29 As for methylphenidate, no improvement in positive symptoms was observed in one study.Reference Carpenter, Winsberg and Camus36
Exploratory meta-analysis
Six studies provided meta-analyzable data comparing positive symptoms ratings between atomoxetine (k=2), d-amphetamine (k=3), or methylphenidate (k=1) versus placebo.Reference Pietrzak, Snyder and Maruff28, Reference Sanfilipo, Wolkin and Angrist30, Reference Friedman, Carpenter and Lu31, Reference Martin, Dirks and Gertsik33, Reference Kelly, Buchanan and Boggs34, Reference Carpenter, Winsberg and Camus36 Neither individual stimulant classes nor pooled analyses (SMD=0.16, 95% CI: -0-28-0.61, p=0.47, I2=50%) showed any significant effect compared with placebo.
Efficacy: negative symptoms
Effects on negative symptoms of atomoxetine,Reference Friedman, Carpenter and Lu31, Reference Sacco, Creeden and Reutenauer32, Reference Kelly, Buchanan and Boggs34 d-amphetamine,Reference Pietrzak, Snyder and Maruff28, Reference Sanfilipo, Wolkin and Angrist30, Reference Martin, Dirks and Gertsik33, Reference Van Kammen, Bunney and Docherty35, Reference Van Kammen and Boronow39, Reference Barch and Carter46 and methylphenidateReference Carpenter, Winsberg and Camus36 were assessed in three, six, and one studies, respectively (Table 3).
Narrative review
While atomoxetine and methylphenidate did not change negative symptoms in three and one studies, respectively, mixed evidence was available for d-amphetamine, with three studies suggesting no effectReference Pietrzak, Snyder and Maruff28, Reference Sanfilipo, Wolkin and Angrist30, Reference Barch and Carter46 and three showing several degrees of improvement compared with placebo.Reference Martin, Dirks and Gertsik33, Reference Van Kammen, Bunney and Docherty35, Reference Van Kammen and Boronow39
Exploratory meta-analysis
Seven studies comparing negative symptom ratings after atomoxetine (k=2), d-amphetamine (k=4), and methylphenidate (k=1) versus placebo provided meta-analyzable data.Reference Pietrzak, Snyder and Maruff28, Reference Sanfilipo, Wolkin and Angrist30, Reference Friedman, Carpenter and Lu31, Reference Martin, Dirks and Gertsik33, Reference Kelly, Buchanan and Boggs34, Reference Carpenter, Winsberg and Camus36, Reference Van Kammen and Boronow39 Neither individual stimulant classes nor pooled analyses showed any significant effect compared with placebo (SMD=0.02, 95% CI: -0-25 to 0.30, p=0.86, I2=0%) showed any significant effect compared with placebo (Figure 2).

Figure 2 Forest plot of effect of stimulants on negative symptoms in patients with schizophrenia.
Efficacy: mood
Effects on mood of atomoxetineReference Kelly, Buchanan and Boggs34 and d-amphetamineReference Goldberg, Bigelow and Weinberger27, Reference Van Kammen and Boronow39 were assessed in one and two studies, respectively (Table 3).
Narrative review
Atomoxetine did not seem to change mood in one study,Reference Kelly, Buchanan and Boggs34 and d-amphetamine did not affect mood in one study, while it improved it in another study.Reference Van Kammen and Boronow39
Exploratory meta-analysis
No exploratory meta-analysis was possible due to partial and heterogeneous data reporting.
Efficacy: cognition
Effects on cognition of atomoxetineReference Friedman, Carpenter and Lu31, Reference Sacco, Creeden and Reutenauer32, Reference Kelly, Buchanan and Boggs34 and d-amphetamineReference Swerdlow, Tarasenko and Bhakta26–Reference Daniel, Weinberger and Jones29, Reference Martin, Dirks and Gertsik33, Reference Barch and Carter46 were investigated in three and six studies, respectively (Table 3).
Narrative review
Atomoxetine failed to improve global measures of intelligence, processing speed, motor speed, verbal fluency, problem solving, verbal learning, visual memory, and attention in two studies.Reference Friedman, Carpenter and Lu31, Reference Kelly, Buchanan and Boggs34 One study did not report results of atomoxetine’s effects on cognition compared with placebo, describing, however, that atomoxetine 80 mg/d enhanced visuospatial working memory and verbal fluency test from baseline.Reference Sacco, Creeden and Reutenauer32 d-Amphetamine improved various isolated cognitive functions across several different studies. These functions included processing speed, visual attention and vigilance, reasoning and problem solving, 28 working memory (response time, accuracy), language production (number of words, filled pauses, thought disorder, poverty of speech), Stroop Task performance (response time, not errors),Reference Barch and Carter46 performance on the Wisconsin Card Sorting Test (WCST; number of correct responses and percent conceptual level),Reference Goldberg, Bigelow and Weinberger27, Reference Daniel, Weinberger and Jones29 and auditory-processing speed after a single session of a cognitive intervention.Reference Swerdlow, Tarasenko and Bhakta26 However, no improvement in visual learning,Reference Pietrzak, Snyder and Maruff28 go/no go, designs, and blink rate was observed with d-amphetamine, while motor speed in finger tapping and trail making improved compared with placebo in one study.Reference Goldberg, Bigelow and Weinberger27 One study did not provide data about the comparison with placebo; however, it described no worsening of processing speed, visual attention, vigilance, and recognition memory from baseline.Reference Martin, Dirks and Gertsik33
Exploratory meta-analysis
Consistent data pooling from several studies was precluded by different cognitive domains being investigated or inadequate data reporting. According to an exploratory meta-analysis including data from two studies,Reference Friedman, Carpenter and Lu31, Reference Kelly, Buchanan and Boggs34 atomoxetine improved problem solving (SMD=0.73, 95% CI: 0.10–1.36, p=0.02, I2=0%) (Figure 3). Moreover, a trend toward a significant improvement with amphetamines compared with placebo resulted for executive functions in a meta-analysis of two studies (SMD=0.80, 95% CI: −1.68–0.08, p=0.08, I2=66%) (Figure 4).Reference Pietrzak, Snyder and Maruff28, Reference Martin, Dirks and Gertsik33

Figure 3 Forest plot of effects of atomoxetine on problem solving in patients with schizophrenia.

Figure 4 Forest plot of effects of d-amphetamine on executive function in patients with schizophrenia.
Several additional exploratory meta-analyses of studies providing quantitative data yielded the following negative results: two studies administering d-amphetamine versus placebo did not find any significant difference in WCST failures, perseverative errors, categories, conceptual level, correct responses, and total score (SMD=0.78, 95% CI: −1.24–2.8, p=0.21, I2=0%).Reference Goldberg, Bigelow and Weinberger27, Reference Daniel, Weinberger and Jones29 Four pooled studies on attention did not yield any significant result (SMD=−0.03, 95% CI: −0.48–0.41, p=0.89, I2=31%) or any difference between atomoxetine (k=1) and amphetamines (k=3) (p=0.32).Reference Pietrzak, Snyder and Maruff28, Reference Martin, Dirks and Gertsik33, Reference Kelly, Buchanan and Boggs34, Reference Barch and Carter46 Three pooled studies did not show any effect of stimulants compared with placebo on working memory (SMD=−0.11, 95% CI: −0.61–0.39, p=0.67, I2=0%) or between atomoxetine (k=1) and amphetamines (k=2) (p=0.67).Reference Friedman, Carpenter and Lu31, Reference Kelly, Buchanan and Boggs34, Reference Barch and Carter46 Three studies investigating processing speed did not show any significant difference with placebo (SMD=0.21, 95% CI: −0.3–0.71, p=0.42, I2=0%) or any difference between atomoxetine (k=2) and amphetamine (k=1) (p=0.68).Reference Friedman, Carpenter and Lu31, Reference Kelly, Buchanan and Boggs34, Reference Barch and Carter46 Finally, two studies did not show any significant effect of atomoxetine versus placebo on verbal learning (SMD=0.45, 95% CI: −0.17–1.07, p=0.16, I2=0%).Reference Friedman, Carpenter and Lu31, Reference Kelly, Buchanan and Boggs34
Efficacy: weight loss and smoking status
Two studies assessed the role of atomoxetine on weight loss and smoking status (Table 3).Reference Sacco, Creeden and Reutenauer32, Reference Ball, Warren and Feldman38
Narrative review
Atomoxetine did not seem effective for either reducing smokingReference Sacco, Creeden and Reutenauer32 or elevated body weight in patients with schizophrenia on clozapine or olanzapine.Reference Ball, Warren and Feldman38
Exploratory meta-analysis
No exploratory meta-analysis was possible due to single studies investigating single outcomes.
Challenge studies: symptom response and relapse prediction
Studies included, treatments, and participants
One trial evaluated the effects on symptoms or relapse prediction of a challenge with amphetamine derivatives (n=19 received amphetamine, n=19 control),Reference Pandurangi, Goldberg and Brink42 and five with methylphenidate (n=120 received methylphenidate, n=49 control) (Table 1).Reference Lieberman, Kane and Sarantakos19, Reference Lieberman, Kane and Gadaleta37, Reference Robinson, Mayerhoff and Alvir40, Reference Sharma, Javaid and Pandey44, Reference Lieberman, Alvir and Geisler45
Narrative review
While d-amphetamine did not induce any significant reduction in Brief Psychiatric Rating Scale (BPRS) score from baseline in one study (no data for comparison with placebo), the same study suggested that individual patients whose psychotic symptoms worsened after an acute challenge later had a better response to antipsychotics and tended not to have enlarged ventricles (Table 3).Reference Pandurangi, Goldberg and Brink42 With regard to methylphenidate, a worsening of BPRS items compared with placebo was shown,Reference Sharma, Javaid and Pandey44, Reference Lieberman, Alvir and Geisler45 which correlated with growth hormone (GH) levels, but not with homovanillic acid (HVA) levels.Reference Sharma, Javaid and Pandey44 After methylphenidate challenge, the provocation test was positive in up to 40% of patients,Reference Robinson, Mayerhoff and Alvir40, Reference Lieberman, Alvir and Geisler45 and psychotic activation was observed more frequently in younger, female patients; patients with more symptoms at baseline; patients with tardive dyskinesia; patients on neuroleptics; and patients with euphoric or mood alterations after methylphenidate challenge.Reference Lieberman, Kane and Gadaleta37, Reference Robinson, Mayerhoff and Alvir40, Reference Lieberman, Alvir and Geisler45 Moreover, patients with psychotic activation after methylphenidate administration relapsed sooner and more frequently.Reference Lieberman, Kane and Sarantakos19, Reference Lieberman, Kane and Gadaleta37, Reference Lieberman, Alvir and Geisler45
Exploratory meta-analysis
No meta-analysis was possible for relapse prediction outcomes due to partial reporting of quantitative data in included studies.
Other biological effects
Studies included, treatments, and participants
All studies discussed here were also listed in the section on interventional therapeutic studies. One study evaluated biological effects of atomoxetine (n=10 atomoxetine, n=10 control),Reference Friedman, Carpenter and Lu31 three studies evaluated the biological effects of amphetamine derivatives (n=8 amphetamines, n=8 control),Reference Schulz, Van Kammen and Pickar43 with two of them (n=39 receiving amphetamines, n=19 control) assessing the effects on symptoms of a challenge with amphetamines (Table 1).Reference Daniel, Weinberger and Jones29, Reference Pandurangi, Goldberg and Brink42 Three studies evaluated the biological effects of methylphenidate (n=19 receiving methylphenidate),Reference Sharma, Javaid and Pandey41 with two of them assessing the effects on symptoms of a challenge with methylphenidate (n=50 receiving methylphenidate, n=49 control).Reference Sharma, Javaid and Pandey44, Reference Lieberman, Alvir and Geisler45
Narrative review
Two studies investigated the effects of atomoxetineReference Friedman, Carpenter and Lu31 and d-amphetamineReference Daniel, Weinberger and Jones29 on brain activation using functional magnetic resonance imaging (fMRI) (Table 3). Compared with placebo, atomoxetine increased activation in the left dorsolateral prefrontal cortex and left posterior cingulate cortex during the N-back test.Reference Friedman, Carpenter and Lu31 Similarly, d-amphetamine increased activation over baseline in the left dorsolateral frontal cortex, right occipital cortex, and right anterior cingulate cortex during WCSTReference Daniel, Weinberger and Jones29; however, no comparison was reported with placebo. One study showed no change in β-endorphin,Reference Schulz, Van Kammen and Pickar43 and one study showed that patients without enlarged ventricles had a better response to antipsychotics after amphetamine challenge.Reference Pandurangi, Goldberg and Brink42 Two studies reported increased GH serum levels after methylphenidate treatment compared with placebo,Reference Sharma, Javaid and Pandey41, Reference Lieberman, Alvir and Geisler45 and one study described a correlation between GH and reduced BPRS positive and mood scores.Reference Sharma, Javaid and Pandey44 A further study described increased prolactin serum levels with methylphenidate compared with placebo,Reference Lieberman, Alvir and Geisler45 while HVA levels seemed unchanged.Reference Sharma, Javaid and Pandey41
Exploratory meta-analysis
No meta-analysis was possible for other biological effects due to partial reporting of quantitative data in included studies.
Safety and tolerability across different designs (therapeutic, challenge, biological effects)
Effects on extrapyramidal symptoms (EPS) of atomoxetine,Reference Sacco, Creeden and Reutenauer32, Reference Kelly, Buchanan and Boggs34, Reference Ball, Warren and Feldman38 d-amphetamine,Reference Sanfilipo, Wolkin and Angrist30, Reference Martin, Dirks and Gertsik33 and methylphenidateReference Lieberman, Alvir and Geisler45 were assessed in three, two, and one studies, respectively.
Narrative review
Atomoxetine did not seem to affect EPS in three trials. While no data were available for a comparison between d-amphetamine and placebo, mixed evidence regarding d-amphetamine indicated reduction of the Abnormal Involuntary Movement Scale score from baseline in one study,Reference Sanfilipo, Wolkin and Angrist30 and no change in Barnes Akathisia Scale and Simpson Angus Scale scores from baselines in another one.Reference Martin, Dirks and Gertsik33 One study using methylphenidate showed reduction of Simpson Dyskinesia Scale score compared with placebo.Reference Lieberman, Alvir and Geisler45 Effects on blood pressure (BP), heart rate (HR), and other safety measures after administration of atomoxetine,Reference Friedman, Carpenter and Lu31, Reference Kelly, Buchanan and Boggs34, Reference Ball, Warren and Feldman38 d-amphetamine,Reference Goldberg, Bigelow and Weinberger27, Reference Daniel, Weinberger and Jones29, Reference Martin, Dirks and Gertsik33 and methylphenidateReference Carpenter, Winsberg and Camus36, Reference Lieberman, Kane and Gadaleta37, Reference Sharma, Javaid and Pandey44, Reference Lieberman, Alvir and Geisler45 were assessed in three, three, and four studies, respectively. Atomoxetine was associated with increased BP compared with placebo one study,Reference Friedman, Carpenter and Lu31 while the other two studies reported no difference from placebo regarding BP, HR, and heart rate–corrected QT (QTc) interval.Reference Friedman, Carpenter and Lu31, Reference Kelly, Buchanan and Boggs34, Reference Ball, Warren and Feldman38 Similarly, d-amphetamine was not associated with any consistent untoward cardiac effects across three studies.Reference Goldberg, Bigelow and Weinberger27, Reference Daniel, Weinberger and Jones29, Reference Martin, Dirks and Gertsik33 Conversely, methylphenidate was associated with an increase in BP and HR in two studies,Reference Carpenter, Winsberg and Camus36, Reference Lieberman, Alvir and Geisler45 while no difference was reported in one study.Reference Lieberman, Kane and Gadaleta37 Clinically relevant HR increase was reported in only one subject among the included studies.Reference Carpenter, Winsberg and Camus36 One study did not provide data about the comparison with placebo and showed minimal HR increase from baseline.Reference Sharma, Javaid and Pandey44
Exploratory meta-analysis
No meta-analysis was possible for tolerability outcomes due to partial reporting of quantitative data in included studies.
Discussion
This systematic review investigating the efficacy, provocation study results, biological effects, and tolerability of amphetamines, methylphenidate, and atomoxetine in people with schizophrenia yielded only 22 studies with a total of 644 patients. Studies were mostly small with high risk of bias and published between 1982 and 2016, with only seven trials published within the last 10 years. Designs and data reporting were mostly limited, allowing only few exploratory meta-analyses of the identified data.
Regarding efficacy, results were disappointing in the areas of positive, negative, and mood symptoms. However, worsening of positive symptoms was also not generally reported, suggesting that antipsychotic treatment can counter potentially negative effects of dopamine agonism, at least in patients agreeing to be studied in this paradigm. This finding is somewhat supported, albeit in a different population that is admittedly at lower risk for psychosis, by a recent study that did not find any increased risk of psychosis in patients with ADHD.Reference Man, Coghill and Chan47 Moreover, in a recent meta-analysis, stimulant users (without schizophrenia) showed a downregulation of both pre- and postsynaptic aspects of the dopamine system (i.e., dopamine release, transporter activity, and receptor availability).Reference Ashok, Mizuno, Volkow and Howes48
Promising results from the narrative review, which showed a potential benefit for cognitive symptoms in schizophrenia with the use of atomoxetine and amphetamines, were only partially confirmed by the small quantitative meta-analysis. While any agent potentially working to improve cognition in schizophrenia would be highly desired,Reference Carbon and Correll6, Reference Millan, Agid and Brune49 too few subjects across a handful of studies could be analyzed for each outcome, making the present exploratory meta-analysis underpowered, and potentially missing more evident harmful or therapeutic effects of atomoxetine, amphetamines, or methylphenidate. Nevertheless, promising and/or marginally significant results of atomoxetine and/or amphetamines on cognitive domains in particular may be worthy of reinvestigation in larger, well-conducted RCTs, ideally in patients receiving long-acting injectable antipsychotics to ensure antipsychotic coverage during treatment with a dopamine agonist.
Among several mechanisms, amphetamines, methylphenidate, and atomoxetine may improve cognitive domains through a selective increase in dopamine activity at the frontal and prefrontal areas,Reference O’Daly, Joyce and Stephan18 as shown by studies investigating biological signatures of clinical effects of stimulants.Reference Daniel, Weinberger and Jones29, Reference Friedman, Carpenter and Lu31
Regarding challenge or provocation tests, some data seem to suggest that patients with acute worsening in response to dopamine agonist challenge are also those responding to antidopaminergic treatment. This is in line with the hypothesis that increased dopamine transmission is a feature of psychosis and a response to first-line antipsychotic treatment.Reference Howes, Kambeitz and Kim50–Reference Demjaha, Egerton and Murray53
As for safety, both d-amphetamine and atomoxetine proved to be safe across the studied populations, while data about methylphenidate suggested a statistically significant increase in BP and HR. However, whether these data result in any clinically meaningful untoward event due to methylphenidate at therapeutic dosages remains unclear. The most convincing evidence in discouraging methylphenidate prescription in patients with schizophrenia actually comes from concerns surrounding symptom worsening, rather than from its cardiovascular safety profile (although no meta-analysis was possible on such symptoms outcomes at this time due to lack of data).
This study has several limitations. First, the number of studies and patients in each design and medication group was small. Second, study designs and outcomes were very heterogeneous. Many studies only reported partial outcomes or partial or non-overlapping results, including several different measures and heterogeneous effect sizes (change from baseline not compared with placebo, difference in change between mean change values with no mention of standard deviation, endpoint values, percentage of improved/worsened/relapsed patients, etc.), precluding any adequately powered meta-analysis. Finally, similar to a recent meta-analysis of 42 different pharmacologic cotreatment strategies added on to antipsychotics in which the quality of the studies analyzed was insufficient to make firm recommendations,Reference Correll, Rubio and Inczedy-Farkas11 all but two of the studies we included in our review were rated as having a high risk of bias according to the Cochrane Collaboration’s risk of bias assessment tool.
Some points of strength of this systematic review should be mentioned as well, in particular the specific focus on RCTs, providing a state-of-the-art picture of the best level of evidence currently available regarding the efficacy, safety, and biological effects of stimulant and atomoxetine in patients with schizophrenia and schizoaffective disorder. Moreover this systematic review completes and expands evidence from an earlier published review that described the evidence up until 1980, including 285 drug-free patients who were administered amphetamine and showed contrasting and heterogeneous response patternsReference Van Kammen, Bunney and Docherty35 ranging from clinical worsening to clinical improvement through no change at all. This review also expands a former systematic review about amphetamines and methylphenidate, as well as modafinil and armodafinil, in schizophrenia.Reference Lindenmayer, Nasrallah and Pucci12 However, that review excluded atomoxetine, included fewer psychostimulant studies, did not focus just on RCTs, and did not quantitatively pool data.
In conclusion, while some heterogeneous evidence points toward possible efficacy of atomoxetine and amphetamines for cognitive symptoms, clearly more studies are needed to provide more detailed evaluation of amphetamines, methylphenidate, and atomoxetine regarding their efficacy, safety, and potential roles as predictors of relapse or response in patients with schizophrenia or schizoaffective disorder.
Disclosures
Marco Solmi, Michele Fornaro, Kuniyoshi Toyoshima, Andrè F. Carvalho, Cristiano A. Köhler, Nicola Veronese, and Brendon Stubbs have nothing to disclose.
Andrea de Bartolomeis has received research support from Janssen, Lundbeck, and Otsuka and has participated as speaker in educational activities supported by unrestricted grant from Chiesi, Lundbeck, Roche, Sunovion, and Takeda. He has served on advisory boards for Eli Lilly, Jansen, Lundbeck, Otsuka, Roche, and Takeda.
Christoph U. Correll has been a consultant and/or advisor to or has received honoraria from: Alkermes, Allergan, Bristol-Myers Squibb, Gerson Lehrman Group, IntraCellular Therapies, Janssen/J&J, LB Pharma, Lundbeck, Medavante, Medscape, Neurocrine, Otsuka, Pfizer, Sunovion, Takeda, and Teva. He has provided expert testimony for Bristol-Myers Squibb, Janssen, and Otsuka. He served on a data safety monitoring board for Lundbeck and Pfizer. He received grant support from Takeda.
The authors declare no conflict of interest.









