Introduction
In recent years, the consumption and abuse of drugs has been identified as one of the most important public health concerns worldwide, mainly due to its health and social consequences, especially in developing countries. In Mexico, for example, the 2016 to 2017 National Addiction Survey reports that the proportion of respondents reporting the consumption of any drug, illegal drugs, and marijuana, at least once in their lifetime, increased significantly from 2011 to 2016; from 7.2% to 7.8%, 6% to 10.3%, and 8.3 to 9.9%, respectively for the population between 12 and 65 years old.Reference Villatoro Velázquez, Resendiz-Escobar and Mujica Salazár1
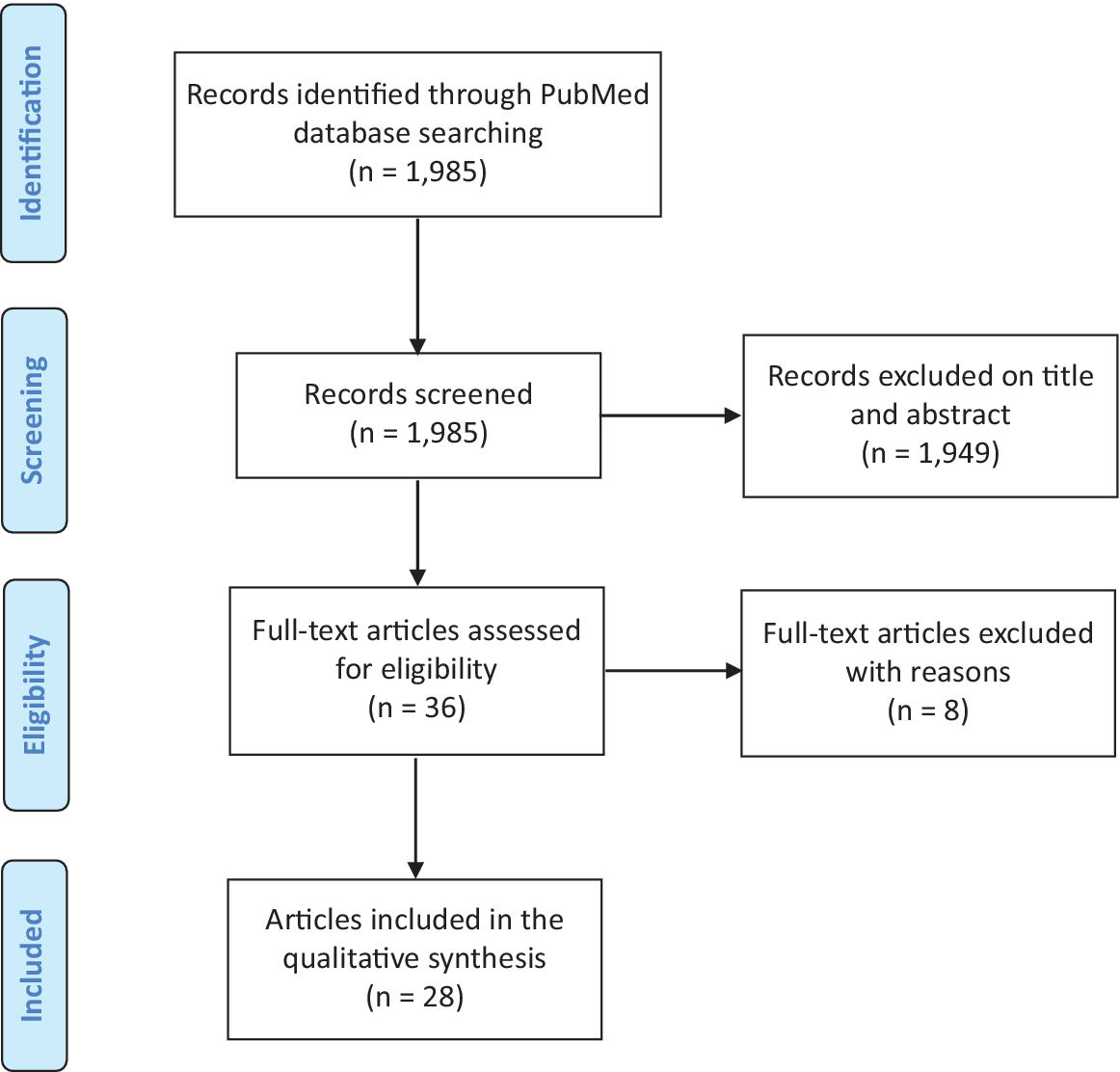
Figure 1. Flow chart of included articles from PubMed and SciELO literature.
Table 1. Parasomnias Associated with Addictions in States of Intoxication and Abstinence.
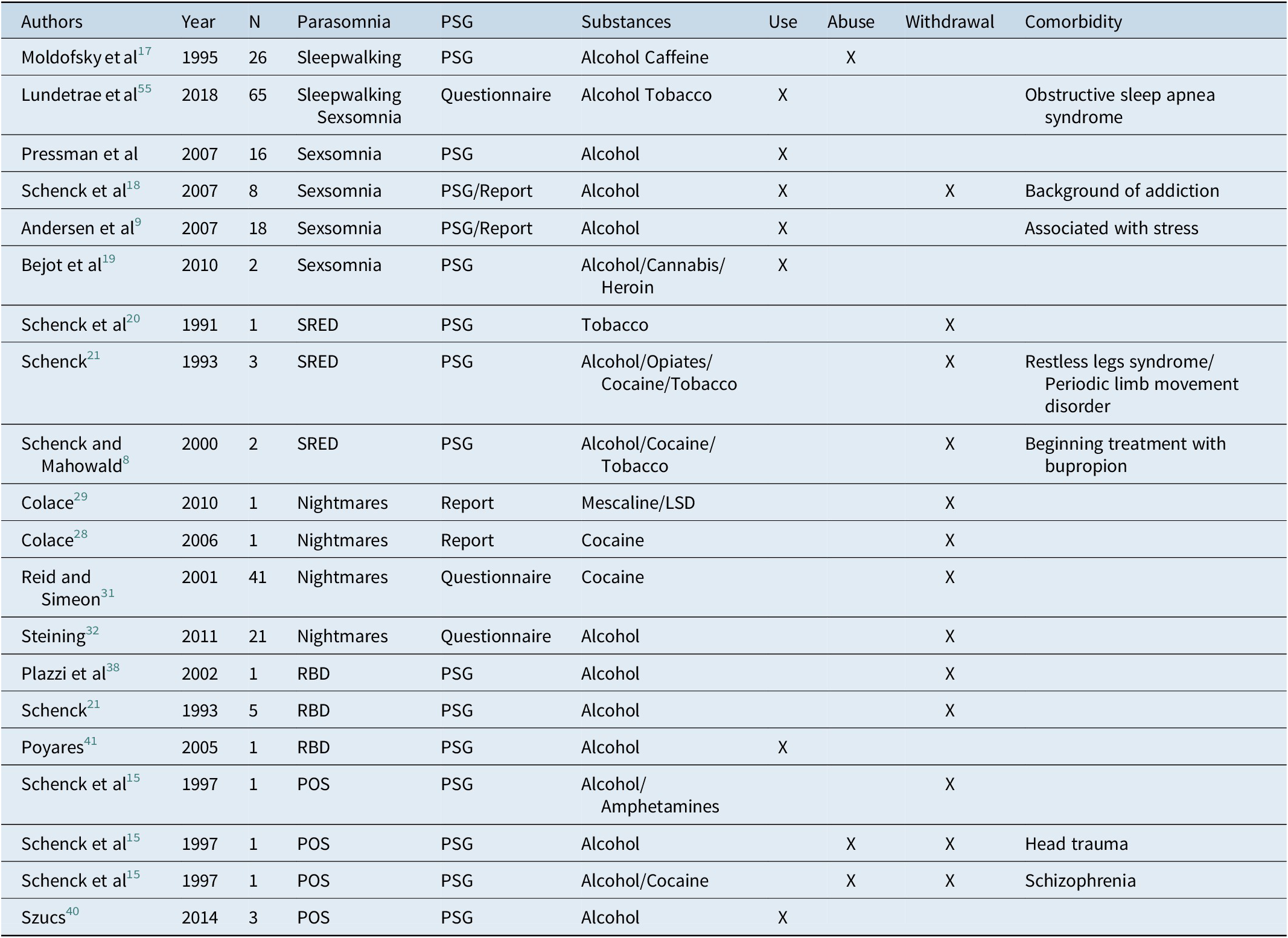
Abbreviations: LSD, lysergic acid diethylamide; POS, parasomnias of superposition; PSG, polysomnography; RBD, rapid eye movements behavior disorder; SRED, sleep-related eating disorder.
Sleep is a physiological process that can be altered by multiple factors including the use, abuse, or withdrawal from addictive substances. Patients suffering from addictions may also have comorbid sleep disorders such as insomnia, obstructive sleep apnea, periodic movements of the extremities, circadian rhythm disturbances, and parasomnias.Reference Chakravorty, Chaudhary and Brower2 It has been reported that sleep disturbance is common among patients in recovery from drug abuse and can precipitate relapses.Reference Berro, Frussa-Filho and Tufik3 It is, therefore, highly important to control disturbances to sleep stemming from addiction and the initiation of the detoxification process.Reference Terán, Majadas and Galan4
Definition of parasomnia
Parasomnias are involuntary problematic behaviors and/or subjective experiences, such as sleepwalking, sleep terrors, dream-enactment, sleep paralysis, nightmares, etc… Parasomnias have been considered to be a state of dissociation between consciousness and behaviorReference Mahowald, Cramer-Bornemann and Schenck5, Reference Mahowald, Cramer-Bornemann and Schenck6
Clinical features
Arousal disorders are parasomnias that occur during slow-wave sleep; with symptoms such as sleepwalking, disorientation, intense fear, eating, or sexual behavior. The prevalence of arousal disorders in the adult population is 4%.Reference Ohayon, Guilleminault and Priest7 They mainly occur during the first part of the night, after the onset of sleep during slow-wave sleep (SWS); this is the reason why there is a high threshold for awakening, and the patient does not have any memory of the behavior. The main clinical features areReference Ohayon, Guilleminault and Priest7:
-
(1) Confusional arousals: Episodes that start with the patient sitting up in bed and looking around in a confused fashion.
-
(2) Sleep terrors: Episodes of pseudo-arousals accompanied by crying, screaming, and other autonomic nervous system and behavioral manifestations of fear.
-
(3) Sleepwalking: May begin as a confusional arousal, followed by walking, leaving bed, sometimes running; agitated violent behavior may also occur.
-
(4) Sleep-related eating disorder (SRED) and sexsomnia have been described more recently:
-
(5) SRED is characterized by episodes in which the patient eats while asleep. This disorder is related to weight gain, gastric discomfort upon awakening, and long-term medical and psychological consequences. SRED can be idiopathic or can be associated with other sleep, medical, and psychiatric disorders and their treatments.Reference Schenck and Mahowald8
-
(6) Sexsomnia is characterized by a repertoire of sexual behavior during sleep that can vary from explicit vocalizations (with sexual content), to violent masturbation and complex sexual activities, including oral sex and vaginal or anal intercourse. In some cases, sexual behavior during sleep can lead to injury of the subject and/or their bed partner, which is considered a special form of violence.Reference Andersen, Poyares and Alves9
In addition to the types mentioned above, there are other parasomnias that are only observed during rapid-eye-movement sleep (REM). These parasomnias manifest during the second half of the night, and the patient has a clear memory of the events and is not difficult to wake.
-
(1) Nightmare Disorder is characterized by recurrent dreams that involve negative and intense emotions, such as fear, anger, disgust, or sadness.Reference Fleetham and Fleming10 Nightmares often provoke awakenings and the patient has very clear dream content memories.
-
(2) REM behavior disorder (RBD) consists of vigorous and apparently “intentional” behaviors that correspond to the content of dreams, mainly nightmares.Reference Schenck, Bundlie and Ettinger11, Reference Schenck, Bundlie and Patterson12 There is high risk of injury to the patient or their bed partner, since the patient frequently makes movements related to defending or attacking.13
-
(3) Sleep paralysis consists of the sensation of awakening and being unable to move; it has been described as an emotionally unpleasant experience, as it is often associated with paranormal phenomena, such as ghosts or the devil. Sleep paralysis occurs in the transition from REM sleep to wakefulness.Reference Malhotra and Avidan14
Parasomnias of superposition (POS) are defined as when the same patient suffers from REM and non-REM parasomnias.Reference Schenck, Boyd and Mahowald15
The following key questions have been proposed for the clinical evaluation of patients with parasomniasReference Postuma, Arnulf and Hogl16:
-
(1) REM Sleep Behavior Disorder
“Have you ever been told, or suspected yourself, that you seem to ‘act out your dreams’ while asleep (eg, punching, flailing your arms in the air, making running movements, etc.)?”
-
(2) Non-REM Parasomnias (arousal disorders)
“Have you ever sleep-walked or had night terrors where you screamed in your sleep?”
-
(3) Sleep-Related Eating Disorder
“Have you ever eaten food without full awareness (or without any awareness) while asleep?”
-
(4) Sexsomnia
“Have you ever been told by a bed partner that you engage in sexual behaviors while asleep, either with yourself or with your bed partner?”
-
(5) Sleep Paralysis
“Have you ever felt paralyzed or unable to move when falling asleep or as you are waking up?”
-
(6) Nightmares
“Do you have unpleasant or frightening dreams or nightmares?”
Objective
The aim of this article is to review the information about the presence of parasomnias in patients with addictions, mainly those related with REM or non-REM sleep, during substance use, abuse, or withdrawal periods, by means of a systematic review.
Methods
Initially, articles on parasomnias and drugs (or addiction) from peer-reviewed journals were identified by the authors. A systematic review of the literature was carried out in two databases: PubMed and SciELO. The screening of the studies was carried out in three phases (by title, abstract, and complete text) independently by two researchers, comparing the results obtained during each screening phase. The discrepancies were discussed until a consensus was reached.
Search strategy
A systematic review was conducted following the PRISMA guidelines. Articles published from 1980 to date were searched in the PubMed database. The search was performed using the following MeSH terms: “parasomnias,” “hallucinations,” “dreams,” “drug utilization,” “substance-related disorders,” “Street drugs, craving,” “anti-anxiety agents,” “hypnotics and sedatives,” and “benzodiazepines.”
Potential articles were identified by title and abstract, using the following eligibility criteria to examine the original research: the studies must be published in English and had to report parasomnias as a consequence of alcohol use or drug abuse. Review articles were excluded. Publications in the reference list of each article were examined to detect any additional papers that could be relevant to this review.
Selection
After possible studies were identified, all retrieved titles and abstracts were reviewed by one investigator (JMMN) to determine their potential relevance. The assessment of the abstracts was carried out independently by the primary investigator (UJC) against the inclusion criteria previously described. Full papers from potential studies were then independently assessed by the two investigators.
Search results
A total of 1985 articles were identified during the title and abstract search. Thirty-six were determined to be relevant for full-text screening, after which 28 articles fulfilled the inclusion criteria. Figure 1 shows the flow chart of the literature included.
Results
Of the 1985 total articles identified in PubMed, 182 papers passed to the abstract phase. Then, 17 papers were chosen for full-text screening. In SciELO, an additional 14 articles were identified, and only one was chosen for full-text screening. Eighteen papers were chosen for full-text analysis from the systematic review, and 10 articles previously identified by the authors were also included (see Table 1).
Arousal disorders in patients with addictions
Sleepwalking and night terrors
Moldofsky et alReference Moldofsky, Russell and Lue17 studied patients with sleepwalking and night terrors, who were classified into three groups according to their clinical history:
-
(1) Patients with violent behavior toward their bed partner or themselves.
-
(2) Patients whose behavior was harmful, but not destructive.
-
(3) Patients who did not show violent behavior.
Log-linear analysis showed that a history of childhood parasomnia, and/or a family history of parasomnia and a stressor, such as psychologic distress, substance abuse, or sleep schedule disorder predicted sleepwalking, or night terror. Both harmful and seriously violent sleep behaviors occurred with drug abuse. In comparison to all other groups, those who were violent to other people were more likely to be males, who experienced more stressors, drank excessive caffeine beverages, and used drugs.Reference Moldofsky, Russell and Lue17
Sexsomnia
In a review of clinical cases of sexsomnia, Andersen et alReference Andersen, Poyares and Alves9 described that, in addition to family or personal antecedents of parasomnias, in 42.5% of the study subjects, alcohol use or the combination of alcoholic beverages with psychotropic drugs, marijuana, or multiple substances was the triggering factor for episodes of sexsomnia.Reference Andersen, Poyares and Alves9
In a review of clinical cases, Schenck et alReference Schenck, Arnulf and Mahowald18 found that eight subjects took enough alcohol (or abused alcohol) the night they had episodes of sexsomnia, hence alcohol was considered to be a likely contributing factor.Reference Schenck, Arnulf and Mahowald18
Béjot et alReference Béjot, Juenet and Garrouty19 described two cases of sexsomnia. The first was a 36-year-old woman with current alcohol consumption and a history of somnambulism that began in childhood; her husband reported that he woke up when she masturbated or when she initiated sexual activity. A polysomnography record (PSG) showed spontaneous alertness during the N3 phase; however, sexual activity was not observed. The second case was that of a 40-year-old woman with a history of cannabis and heroin use during adolescence, who presented her first episode of sexual behavior during sleep at 35 years old.Reference Béjot, Juenet and Garrouty19
Sleep-related eating disorder (SRED)
There are reports of cases of SRED associated with substance use.Reference Schenck, Hurwitz and Bundlie20 Schenck et alReference Schenck, Hurwitz and Bundlie20 described that, in a series of 19 adult patients, the main causal factors were sleepwalking, periodic limb movement syndrome, and abuse of triazolam; they also mentioned that the episodes of SRED stopped when the drug was discontinued. In a complementary series of cases of patients with SRED, suspension of alcohol abuse was associated with SRED in a 48-year-old man with periodic limb movement syndrome (PLMS). In the second case, a 34-year-old woman with persistent somnambulism, recent abstinence from alcohol, and abuse of opiates and cocaine was observed by her roommate to consume food while asleep. In the third case, a patient with restless leg syndrome and PLMS developed SRED after smoking abstinence.Reference Schenck, Hurwitz and O’Connor21 In another case study, Khazaal et alReference Khazaal, Krenz and Zullino22 reported the case of a patient who presented sleepwalking and SRED during smoking abstinence with pharmacological treatment with bupropion.Reference Khazaal, Krenz and Zullino22
REM sleep parasomnias and addictions
Nightmares
Patients with addictions to substances often have nightmares in which they dream that they crave the substance or that they are consuming it. The issue is so important that Colace even proposed that these nightmares could be a predictor of relapse.Reference Colace23
Related to sleep, it has been described that insomnia and unpleasant dreams could be depressive symptoms during cocaine withdrawal that may be associated with greater severity of cocaine dependence.Reference Sofuoglu, Dudish-Poulsen and Poling24
Christo and Franey studied dream content in 101 poly-drugs users (mainly alcohol, heroin, other opiates, and cocaine) at onset, after 6 weeks of abstinence, and 6 months later, and found that 63 subjects recalled having drug dreams at some time when using drugs, 85 subjects reported at least one drug-related dream since they stopped using drugs, and only 16 subjects had no such dreams while abstinent.Reference Christo and Franey25
In an epidemiological study in a sample of 3516 adults, Wetter and Young reported that smoking was associated with onset insomnia; excessive daytime sleepiness was related to smoking only in women, while nightmares were related to smoking only in men. The authors concluded that sleep disturbance may be more prevalent among smokers due to the stimulant effects of nicotine, nightly withdrawal, an increased prevalence of sleep-disordered breathing relative to nonsmokers, and/or an association with psychological disturbance.Reference Wetter and Young26
Yee et alReference Yee, Perantie and Dhanani-Nafisa27 studied dream content in a sample of bipolar patients with cocaine dependence and found that dreams about using drugs and craving drugs were reported by 75% and 68.8% of the patients, respectively, and the experience was described as unpleasant by patients. The frequency of drug dreams showed an important decrease from 3 to 36 weeks into the study.Reference Yee, Perantie and Dhanani-Nafisa27
In another case report by Colace, he documented the case of an 18-year-old woman who had been using cocaine for 1 year. During the first month of psychological treatment, the patient presented vivid dreams, in which large amounts of cocaine were administered intravenously, which she reported as generating intense feelings of pleasure during the dream, but a strong feeling of sadness upon awaking.Reference Colace28
In another case investigated by Colace, he reported the case of a 23-year-old woman who used mescaline and LSD frequently for 3 years and was then admitted to a psychological treatment program with a diagnosis of dependence. During the first days of treatment, she remembered having a vivid dream, in which she used LSD; days later she had a relapse (benzodiazepine use) and later abandoned treatment.Reference Colace29
In a recent study, it was described that users of cocaine and crack had a higher frequency of dreams than patients consuming other substances (opiates and alcohol), and that this was associated with negative changes in mood.Reference Tanguay, Zadra and Good30
In a sample of patients in rehabilitation for cocaine dependence, during the first month of abstinence, 89.1% of the patients reported having dreams in which they consumed drugs, an average of 2.5 times per week; 60.9% of patients still dreamed that they used cocaine after 6 months of abstinence.Reference Reid and Simeon31
When Steining et alReference Steinig, Foraita and Happe32 evaluated patients with alcohol dependence, 92% of them reported poor sleep quality. They also reported terrifying dreams in which they consumed alcohol, and this was related to more feelings of guilt, fear, and helplessness compared with the controls.Reference Steinig, Foraita and Happe32
In the FINRISK study of more than 13 000 participants, the frequency of alcohol intoxication was associated with a greater number of nightmares in males.Reference Sandman, Valli and Kronholm33
Sleep paralysis
A study conducted in Chinese adolescents found that the risk of presenting sleep paralysis was significantly higher among alcohol users than those who had never consumed alcohol.Reference Ma, Wu and Pi34 Similarly, Munezawa et alReference Munezawa, Kaneita and Osaki35 reported that the prevalence of sleep paralysis was higher in adolescents when they reported the consumption of alcoholic beverages one or more days during the past month.Reference Munezawa, Kaneita and Osaki35
REM behavior disorder (RBD)
Schenck et alReference Schenck, Hurwitz and Mahowald36, Reference Schenck, Hurwitz and Mahowald37 reported the onset of RBD after cessation of use or abuse of REM sleep-suppressing agents (ethanol, amphetamine, cocaine, and imipramine), presumably inducing a persistent and intense disorder due to REM sleep rebound.Reference Schenck, Hurwitz and Mahowald36, Reference Schenck, Hurwitz and Mahowald37
Plazzi et alReference Plazzi, Montagna and Meletti38 documented the case of a 56-year-old patient who presented REM sleep behavior disorder during the period of abstinence from alcohol consumption.Reference Plazzi, Montagna and Meletti38 However, in a review of medical records, the consumption of alcohol, caffeine, and illicit substances was not related to RBD.Reference Teman, Tippmann-Peikert and Silber39
Parasomnias of superposition (POS)
Parasomnias of Superposition affect men more frequently than women, and, in most cases, begin during adolescence.13 In the original report by Schenck et al,Reference Schenck, Boyd and Mahowald15 the following three cases were reportedReference Schenck, Boyd and Mahowald15:
-
1. A 40-year-old man with sleepwalking of childhood onset developed RBD during abstinence following abuse of alcohol and amphetamines.
-
2. A 32-year-old woman who had childhood-onset parasomnia that was aggravated by head trauma (resulting in a coma that lasted for several days), due to alcohol abuse, and the following withdrawal.
-
3. A 32-year-old man who developed schizophrenia and parasomnia during adolescence with exacerbations of both conditions associated with abuse of withdrawal from alcohol and cocaine.
Szucs et alReference Szucs, Kamondi and Zoller40 studied 13 subjects with violent behavior during sleep, which was related to alcohol consumption in three patients.Reference Szucs, Kamondi and Zoller40
Other psychotropic addictive substances, such as hallucinogens, solvents, and other substances, were not found in the search.
Discussion
Main findings
This is the first systematic review of the literature analyzing the relationship between two important issues: addiction and parasomnias. The results will be of interest for sleep disorder medicine and for rehabilitation and addiction medicine. However, other disciplines could also benefit from this review, including neurology, neurosciences, psychiatry, psychology, neuropsychology, occupational therapy, and others. Our review detected events of unwelcome parasomnias in patients with many types of drug addiction during both the consumption and rehabilitation phases.
Parasomnias in patients with addictions: comparison with other studies and explanations
It has been previously published that sleep deprivation and comorbid sleep disorders, such as insomnia, sleep apnea, periodic limb movements syndrome, and others, are trigger factors for episodes of parasomnias, and that sleep deprivation and poor sleep quality are frequent symptoms in patients with addictions.13 It would, therefore, be expected that comorbid sleep disorders, sleep deprivation, and poor sleep quality, which are trigger factors for parasomnias, are increased in patients with addictions. This possibility should be explored in future investigations.
It has been reported that patients with alcohol abuse disorder suffer from a multitude of sleep disruptions (profound insomnia, excessive daytime sleepiness, and altered sleep architecture) during both drinking periods and abstinences, caused by a disrupted sleep homeostasis.Reference Thakkar, Sharma and Sahota42 Acute alcohol consumption increases sleep latency, decreases total sleep time, increases non rapid eye movements (NREM) sleep,Reference Brower43 and suppresses REM sleep, after which REM sleep rebounds or returns to baseline levels.Reference Knapp, Ciraulo and Datta44 On the other hand, REM sleep latency decreases during alcohol withdrawal.Reference Brower43 Using a rat model, it was found that intraperitoneal injections of ethanol increase non-REM sleep, but suppresses REM sleep; while nicotine suppresses both non-REM and REM sleep. Combined ethanol and nicotine administration attenuated both substances’ effects on non-REM sleep, but REM sleep remained suppressed.Reference Alam and Sinha45
Interestingly, one of the recommendations for patients with arousal disorders is to get sufficient sleep time to avoid a deep sleep rebound and decrease the frequency of non-REM parasomnias. Possibly, the above-described alteration in sleep homeostasis and increase in non-REM sleep could trigger the sexsomnia episodes related to alcohol consumption described by Andersen,Reference Andersen, Poyares and Alves9 Schenk and Bejot.Reference Béjot, Juenet and Garrouty19
Disinhibition of REM sleep could be one of the provoking factors of nightmares, sleep paralysis, and RBD reported in patients with alcoholism during withdrawal. This has been suggested by many authors46-48 that have proposed that hallucinations in delirium tremens represent an intrusion of REM sleep into the waking state, which is another indication of increased REM sleep pressure during alcohol withdrawal.
Research about smoking and sleep has provided some inconsistent results. Zhang et alReference Zhang, Samet and Caffo47 found that smokers and nonsmokers differ in non-REM sleep but not in REM sleep,Reference Zhang, Samet and Caffo47 while other authors have reported that nicotine suppressed REM sleep.Reference Alam and Sinha45, Reference Jahene, Loessl and Barkai48 Certainly, the stimulating effect of smoking causes insomnia symptoms or insufficient sleep in smokersReference Wetter and Young26, Reference Sabanayagam and Shankar49; however, the increase in REM sleep during tobacco or cocaine withdrawal may be the cause of nightmares,Reference Schierenbeck, Riemann and Berger50, Reference Irwin, Bjurstrom and Olmstead51 as described previously.28-31
Considering the cases discussed above, it is important that guidelines for the clinical practice during rehabilitation include safety measures to protect patients and their bed partners, such as sleeping in separate beds, or bedrooms, or in a large bedroom, sleeping on the ground floor, locking the windows, or covering them with heavy drapes, removing mirrors and furniture from the bedroom, and removing sharp objects and objects with sharp corners. In more severe cases, patients should sleep in a sleeping bag closed with a zipper.Reference Poyares41
Hypothesis of neurobiological substrates of parasomnias
Considering the behavioral manifestation of parasomnias in specific sleep phases, it could be suggested that they each have their own neurochemical substrates. Although there is little information available, coincidentally, it has been reported that parasomnias may often be the expression of increased activity of the reward system during sleep.Reference Perogramvros, Aberg and Gex-Fabry52 After examining two patients with SRED, who exhibited elevated novelty seeking and increased reward sensitivity, one author suggests that an activation of the reward system during sleep may offer a permissive condition for episodes of nocturnal overeating, especially in patients with elevated reward sensitivity and novelty seeking.Reference Perogramvros, Baud and Hasler53
The consumption of alcohol (perhaps due to its depressive central nervous system effects) was related to arousal disorders, such as sexsomnia or SRED; and, as described, REM sleep disinhibition during withdrawal from alcohol or cocaine is associated with REM sleep parasomnias (ie, REM behavior disorder or drug consumption dream content).
It is possible that the presence of parasomnias during childhood or adolescence could be considered a risk factor for addictions in adulthood. On the other hand, drug consumption in adolescence could be a risk factor for parasomnias in adult life. Both hypotheses deserve more research.
Clinical implications
First, it is important to consider the possibility of parasomnias in patients that face addictions or are in the processes of rehabilitation. To avoid accidents in the bedroom and legal problems, and improve the evolution and prognosis of addicted patients, safety measures must be taken during the sleep period, pharmacological therapies that may trigger parasomnias should be avoided, sleep hygiene should be improved, and comorbid sleep disorders should be treated pharmacologically and behaviorally.
Strengths and limitations
The main strength of the systematic review is the novelty of the topic, addressing the need for identification, diagnosis, therapy, and rehabilitation of parasomnias during the acute and chronic phase of treatment of patients with addiction. Previously, symptoms of parasomnias had been strongly neglected or had not received enough attention.
On the other hand, we can identify two weaknesses in our review. First, the articles included were mostly case reports and case series; this was due to the fact that we found no original articles with systematic observations related to the subject of the review. Secondly, in the reviewed articles, there was little additional information about other pathological conditions, pharmacological treatments, or comorbid sleep disorders (including sleep habits) of the reported patients.
We highlight the need to improve the methodology to increase knowledge about the occurrence of parasomnias in patients suffering from addiction. In another sense, obtaining clinical data (such as sleep habits, comorbidities, and pharmacological treatments) would be very useful in determining the possible weight of other confounding factors. For example, it has been described that pharmacological therapies with antidepressants are a trigger factor of RBD symptoms in patients with depression.Reference Postuma, Gagnon and Tuineaig54 According to our observation in this review, in the clinical evaluation of patients with addictions, it is important to ask about parasomnias and other sleep disorders beyond insomnia, apnea, or periodic limb movements, which cause sleep deprivation and are also triggering factors of parasomnias.
Despite these limitations, the literature reviewed showed that parasomnias (REM or non-REM) are found in patients that consume or are going through withdrawal from several different drugs. However, our study design did not allow us to conclude whether parasomnias are more frequent in patients with addiction due to the lack of a population-based sample. This suggests that the interrelationship between different factors, such as changes in neural system functioning, comorbid sleep disorders, pharmacological treatment, stress, and antecedents of parasomnias in childhood or adolescence, are essential to understanding the existence of parasomnias in adult patients with addictions.
Conclusion
Several types of parasomnias have been described in patients with addictions and withdrawal. These parasomnias may occur as arousal disorders, REM-sleep association, and parasomnias of superposition.
Acknowledgments
The authors thank Mr. Horacio Balam for his help in manuscript preparation.
Funding details
There is no funding to declare.
Disclosures
U. Jiménez-Correa, R. Santana-Miranda, A. Barrera-Medina, J.M. Martínez-Nuñez, H.A. Marín-Agudelo, A. Poblano, and I. Hernández-Berber declare no conflicts of interest.
C.H. Schenck is a consultant for Sunovion Pharmaceuticals, Inc., but the industry had no role in the study design, the collection, and interpretation of data, the writing of the manuscript, or the decision of submission.
Authors’ contribution
UJC, conception and design of the study, acquisition and analysis of data, drafting the manuscript; RSM, acquisition and analysis of data, drafting the manuscript; ABM, acquisition and analysis of data, drafting the manuscript; JMMN, acquisition and analysis of data, drafting the manuscript; HAMA, acquisition and analysis of data, drafting the manuscript; AP, acquisition and analysis of data, drafting the manuscript; CHS, acquisition and analysis of data, drafting the manuscript; IHB, acquisition and analysis of data, drafting the manuscript.




