Overview and Introduction
The diagnostic system for the neurodevelopmental disorders, specifically autism spectrum disorder (ASD) and attention-deficit/hyperactivity disorder (ADHD), has evolved over the past decade. In the United States, the current system in place is the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5). Outside of the U.S., and for the purposes of insurance and other coding procedures, the internationally recognized medical system is the International Statistical Classification of Diseases and Related Health Problems, Tenth Revision, Tenth Revision (ICD-10). This review will first highlight the important changes that the DSM-5 has undergone since the previous version, Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision (DSM-IV-TR). Next, we will cover similarities and differences in the classification of neurodevelopmental disorders between the DSM-5 and the ICD-10, focusing on ASD and ADHD. By examining some of the important revisions made recently for the DSM-IV-TR to the DSM-5, and by comparing the purpose and function of the two distinct diagnostic systems (DSM-5 versus ICD-10), we can help to anticipate changes in the upcoming ICD-11. The DSM-5 and the ICD-10 reflect differences in the tradition and purpose of diagnostic systems, and this review will examine how these different systems stem from having different goals. The primary goal of the DSM-5 is to enhance clinical utility, and a secondary goal is research purposes. The ICD-10, in contrast, has 4 purposes: clinical utility and common diagnostic language, insurance purposes, legal issues, and research longevity. Overall, this review will highlight the importance of progress toward complementary and consistent diagnostic classification systems, keeping in mind that these systems are dynamic and changing as we learn more about mental disorders and their underlying etiology. Finally, this review will touch on alternative diagnostic approaches to mental illness, such as the Research Domain Criteria (RDoC), which attempts to link symptom domains to underlying biological and brain circuitry mechanisms. This new direction may eventually affect diagnostics, treatment development, and insurance coverage in the United States and worldwide.
DSM-IV-TR to DSM-5: Neurodevelopmental Disorders
In order to accurately assess and compare the current DSM and ICD diagnostic systems, it is helpful to examine the revisions made to the DSM-5 from the DSM-IV-TR regarding neurodevelopmental disorders. A major change overall for the DSM-5 was the elimination of the mulitaxial system of classification used in all previous versions of the manual.Reference Harris 1 Arguably the most significant change for child and adolescent psychiatric disorders in the DSM-5 was the deletion of the chapter entitled “Disorders Usually First Diagnosed in Infancy, Childhood, or Adolescence” and the creation of the new chapter entitled “Neurodevelopmental Disorders,” which reflects a general approach in the DSM-5 to be representative over the lifespan.Reference Eapen and Crncec 2 The term “neurodevelopment” encompasses an important component: that individuals exhibit difficulties from birth onward, and that the cause is often situated neurologically, in gestation or birth.Reference Van Herwegen and Riby 3 Attention deficit/hyperactivity disorder was included in this new category of Neurodevelopmental Disorders, and some major changes were made in regard to autism diagnosis.
Autism spectrum disorder
Autism was one of the disorders that received the most public attention in response to changes in the DSM-5 back in May 2013. Notable changes included removal of the 5 separate pervasive developmental disorders (PDDs), creation of the “spectrum” diagnosis, and the reducing the 3 core domains of autism down to 2. Regarding the first major revision, the separate PDDs (autistic disorder, Asperger’s disorder, Rett’s disorder, childhood disintegrative disorder, and PDD-not otherwise specified, or NOS) had been criticized for a pseudo-specificity that impacted treatment research, insurance coverage, and general classification and diagnosis of developmental disorders.Reference King, Navot, Bernier and Webb 4 The separate diagnoses of the PDDs led to a deficit in reliability, particularly regarding the “not-otherwise-specified” (NOS) category. Under the classification of the DSM-IV-TR, a majority of individuals with autism, almost 5-fold, were diagnosed into the PDD-NOS category.Reference Volkmar, State and Klin 5 This NOS category was unspecific and oftentimes ambiguous for diagnostic purposes, and yet became the most commonly given diagnostic category for persons with communication disorders.Reference Eapen and Crncec 2 Despite these obvious limitations of the separate PDD diagnoses in the DSM-IV-TR, there was considerable controversy over the removal of this system and the creation of the single autism spectrum disorder diagnosis, with particular resistance regarding the removal of the Asperger’s syndrome.Reference King, Navot, Bernier and Webb 4 Overall, the removal of these separate diagnoses was made to improve specificity and sensitivity regarding autism diagnosis, to create more accurate description and communication regarding developmental disorders, and to serve as a more useful and productive backdrop for treatment planning.Reference Eapen and Crncec 2 The creation of the autism spectrum was an advance diagnostically, as it helped to remove pseudo-specificity and to create an all-inclusive diagnosis for a very heterogeneous disorder.Reference Wilson, Gillan and Spain 6
A second major change in autism diagnosis was the reduction of 3 core domains down to 2 core domains. Upon significant review within the field, a consensus was reached that it was arbitrary to distinguish the social and communication domains; therefore these 2 areas were combined, such that the new system of ASD classification includes social and communication deficits as one domain, and repetitive and restrictive behaviors as the second required domain. 7 Given the removal of the NOS category, individuals who do not present with a full range of these 2 symptom domains are no longer eligible for a diagnosis of ASD. Therefore, the Neurodevelopmental Disorders chapter now includes an option for diagnosis of social (pragmatic) communication disorder for persons presenting with the social and communicative limitations associated with autism, but lack the repetitive and restrictive behaviors.Reference King, Navot, Bernier and Webb 4
There were considerable discussions regarding the revisions made for the DSM-5 Neurodevelopmental Disorders chapter. Many of these criticisms have been overshadowed in light of the demonstrated success of the DSM-5 as an improved diagnostic system compared with the previous DSM-IV-TR version.Reference King, Navot, Bernier and Webb 4 The most prominent arguments were 2-fold. The first surrounded the removal of the Asperger’s syndrome (AS) diagnosis, and the second regarded the potential impact that diagnostic revisions might have on access to services for children and adolescents with ASD and ADHD (considering that fewer needed criteria were listed for neurodevelopmental disorders such as autism and ADHD). A legitimate concern, and one that should be considered for future classification system revisions, was the complaint over the lack of preparation in the community for the removal of these separate PDDs, specifically AS. It is important to ensure that the clinical and patient communities at large be well informed of the reasons and logic behind major diagnostic revisions.
Attention deficit/hyperactivity disorder (ADHD)
ADHD was another childhood and adolescent psychiatric disorder that underwent notable revisions for the DSM-5. The inclusion in the category of Neurodevelopmental Disorders was in and of itself a major change for ADHD, whereas in the DSM-IV-TR, ADHD was classified as a disruptive behavior disorder. The diagnostic criteria of ADHD also underwent some revisions in DSM-5. The same 18-symptom criteria were included as before, but specific examples were added under each criterion, to facilitate easier classification of the disorder across the lifespan. The change in onset age was revised, so that onset must occur prior to 12 years of age, rather than the previously more restrictive onset barrier symptom demonstration before 7 years of age. Specifiers were also included, in order to designate either predominantly inattentive or predominantly hyperactive/impulsive presentations of ADHD. The criterion for adult diagnosis of ADHD underwent a symptom threshold change: adults now have a cutoff of 5 symptoms of inattention or hyperactivity, in contrast to the required 6 symptoms in younger persons. Finally, the DSM-5 chapter of Neurodevelopmental Disorders allows for the comorbid diagnosis of ADHD and ASD, which was not permitted in the DSM-IV-TR.Reference Harris 1 Many patients with ADHD were missed in the DSM-IV-TR, either because they had milder symptoms, or were able to compensate for their difficulties through other coping mechanisms. The new system is aimed toward a greater sensitivity for these individuals, providing earlier detection, diagnosis, and treatment planning.Reference Wilson, Gillan and Spain 6 Overall, the goal behind the addition of the neurodevelopmental disorders section in the DSM-5, and the revisions of ASD and ADHD, is to create a category that represents the developmental trajectories of these disorders, which will create diagnostic systems that accurately accommodate the plasticity of neurodevelopment over the lifespan.Reference Wilson, Gillan and Spain 6
ICD-10: Autism and ADHD
Pervasive developmental disorders
The International Classification of Disease, 10th Revision (ICD-10) is the worldwide recognized system of medical diagnosis. The ICD is created and supported by the World Health Organization (WHO), and its primary goal lies in that of classification, rather than the primary goal of diagnosis, as in the DSM.Reference Rutter 8 The WHO is not a psychiatric society like the American Psychiatric Association (APA), and the ICD reflects different initiatives than those of the DSM.Reference Baird 9 The ICD serves as a general medical system, with specifiers for underlying etiology, similar to classification of all other medical diseases. In the ICD-10, autism is classified under Chapter V, “Mental and Behavioural Disorders, Disorders of Psychological Development (F80-89).” The disorders in this chapter subtype are described as having the following in common: “(a) onset invariably during infancy or childhood, (b) impairment or delay in development of functions that are strongly related to biological maturation of the central nervous system, and (c) a steady course without remission or relapses.” 10 Autism is listed under the subcategory of Pervasive Developmental Disorders, code F84. These PDDs are defined similarly as they were in the DSM-IV-TR, as “characterized by qualitative abnormalities in reciprocal social interactions and in patterns of communication, and by a restricted, stereotyped, repetitive repertoire of interests and activities. These qualitative abnormalities are a pervasive feature of the individual’s functioning in all situations”. 11 Under PDDs in the ICD-10, there are 8 different disorders listed: Childhood Autism (F84.0), Atypical Autism (F84.1), Rett Syndrome (F84.2), Other Childhood Disintegrative Disorder (F84.3), Overactive Disorder Associated with Mental Retardation and Stereotyped Movements (F84.4), Asperger Syndrome (F84.5), Other Pervasive Developmental Disorders (F84.8), and finally, Pervasive Developmental Disorder, Unspecified (F84.9). This system of separate diagnosis is quite similar to that of the outdated DSM-IV-TR, and clearly differs significantly from the current version of the DSM. There is a stark contrast between the one Autism Spectrum Disorder in the DSM-5 and the 8 different Pervasive Developmental Disorders in ICD-10. It remains to be seen whether ICD-11 will move in the direction of DSM-5 in consolidating the various distinct conditions into a broader spectrum. Currently, all practicing clinicians in the United States are going through training to incorporate the ICD-10 codes into their practice. All individuals diagnosed with a DSM-5 mental disorder in the U.S. will also be given an ICD-10 code, with appropriate specifiers. It is still unclear how well this new adaptation of coding will be executed, specifically in the neurodevelopmental disorders of the DSM-5 and pervasive developmental disorders of the ICD-10.
ADHD is not included in the previous category along with autism, but rather is classified under F90-F98, “Behavioral and Emotional Disorders with Onset Usually Occurring in Childhood and Adolescence.” In the ICD-10, ADHD is actually referred to under Hyperkinetic Disorders (F90), which are characterized by the following: “an early onset (usually in the first five years of life), lack of persistence in activities that require cognitive involvement, and a tendency to move from one activity to another without completing any one, together with disorganized, ill-regulated, and excessive activity.” 10 ADHD can be found in the ICD-10 under the code F90.0, Disturbance of Activity and Attention, and “attention deficit” can be defined as one of the following: attention deficit disorder with hyperactivity, attention deficit hyperactivity disorder, or attention deficit syndrome with hyperactivity. 10 Hyperkinetic disorder associated with conduct disorder (F90.1) is listed as an exclusion for ADHD. Notably, in the ICD-10, pervasive developmental disorders are classified as exclusionary for hyperkinetic disorders. This exclusion was eliminated in the DSM-5 for autism, with a comorbid diagnosis of ADHD allowed, and vice versa. It is clear that, overall, the classification of ADHD varies considerably between the current DMS-5 and the ICD-10. Similar to the discrepancy between autism in DSM versus ICD, it remains to be seen how application of the ICD-10 codes will come to fruition regarding cases diagnosed with DSM-5 ADHD.
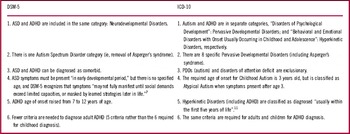
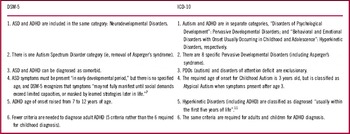
The 2 systems of diagnostic classification demonstrate considerable contrasts (see Table 1). Considering that the APA and WHO reflect differing goals, it is not unexpected that the DSM and ICD would vary to some degree. However, examination of the classification and diagnostic criteria of ADHD and autism in the 2 systems illuminates the potential issues that could ensue as the ICD-10 comes online in the United States. This review demonstrates the progress made by the DSM-5, and the discrepant areas needing improvement in the revision of ICD-10 in the future development of ICD-11.
Table 1 Differences in autism and ADHD: DSM-5 versus ICD-10
ICD-11: Looking Forward for Neurodevelopmental Disorders
The ICD-11 is due for publication in 2017, and is currently in the process of review by representatives from over 200 countries.Reference Levy 12 Given the recent revisions in the publication of DSM-5 in May 2013, clinicians and research scientists alike can expect to see some complementary re-structuring in the ICD-11. The question that does still remain, however, is to what extent the ICD-11 will mirror the DSM-5, keep with the structure of the ICD-10, or encompass a new paradigm shift towards domain-based classification for mental disorders.
It is logical to expect that the transition from the ICD-10 to the ICD-11 will demonstrate some parallel to changes from the DSM-IV-TR to the DSM-5. It is also important that ICD-11 build on progress from the DSM-5, and take advantage of the exposure of its shortcomings. The criticisms of the DSM-5, particularly in reference to the neurodevelopmental disorders section, may serve as a reference for ICD-11 planning. One critique in particular, regarding the lack of preparation in the community regarding the removal of the Asperger’s syndrome diagnosis, is something that can be taken into consideration when it comes time to implement the new ICD-11. In regard to ADHD, research has demonstrated an important finding that executive function (EF) difficulties serve as consistently important predictors of ADHD diagnosis in affected adults, though these symptoms were not present before the age of 7. A possible improvement for the ICD-11 could be to include more EF items, considering that these issues are present in most adults with ADHD.Reference Kessler, Green and Adler 13 A recent study also examined how introducing cross-cutting dimensions could help to improve the categorical framework of the DSM-5, but unfortunately this implementation was not validated in time for its publication. This new framework is still a viable option for the ICD-11.Reference Bakker, Wichers, van Harten, Myin-Germeys, Delespaul and van Os 14 By building off the DSM-5 and ICD-10, the ICD-11 should serve as a more unified, valid, and reliable classification system worldwide.
In looking toward the future of mental disorder classification, it is important to consider the paradigm shift of RDoCs. FirstReference First 15 examines the influence of the Research Domain Criteria (RDoC) initiative of the National Institute of Mental Health (NIMH), and how this could represent a significant change in the world of mental health classification. This shift refers to moving away from defining disorders based on descriptive phenomenology and focusing instead on neural circuitry. Considering the developmental trajectory, sensitive periods, and dynamic interactions of systems that are inherent to neurodevelopmental disorders, this perspective provides a viable argument for the dimensional, rather than diagnostic, approach of the RDoC initiative.Reference Casey, Oliveri and Insel 16 While domain-based classification could improve reliability of objective measurement and overall causal validity, it is important to maintain phenomenological description and subtypes for the sake of diagnostics.Reference Levy 12 Ideally, the goal for ICD-11 should be to serve as a superior general medical system for mental disorders that uses a classification system cohesive with that of the DSM-5, draws on the success of the ICD-10, and incorporates the enrichment of a domain-based system to eliminate the heterogeneity. Specific to neurodevelopmental disorders, the ICD-11 should include specified language geared toward pediatric populations, while also organizing neurodevelopmental disorders so that they orient across the lifespan. Recent studies have examined the possible advantages of cluster-based organization when considering the meta-structure of the DSM-5 and the ICD-10, finding that this type of organizational system could lead to improved clinical practice, public administration, and research.Reference Andrews, Goldberg and Krueger 17 The goal is for the DSM-5, the ICD-11, and the RDoC to serve as complementary systems in order to improve diagnosis, prognosis, and treatment for children and adults diagnosed with neurodevelopmental disorders.
Disclosures
Ellen Doernberg does not have anything to disclose. Eric Hollander has the following disclosures: for consultancy, Roche, Coronado, and Transcept; for research support, Roche, Sunovion, Lundbeck, Forest, Coronado, and Brainsway.