Introduction
Aggression and agitation are among the most frequent reasons for psychiatric hospitalization in adulthood. Aggressive and agitated psychotic patients frequently refuse treatment; moreover, these behaviors typically emerge in patients who relapse after they stop their medications. Aggressive behaviors increase the burden of care for families and require large amounts of staff time and effort at psychiatric inpatient units. Aggression is also a major contributor to the stigma of mental illness.
Psychotic patients sometimes resist such care as bathing, and they frequently refuse their medications because of a lack of insight into their mental illness. These problems may lead to disagreements and conflicts between patients and their caregivers or ward staff. Such conflicts may aggravate the patients’ behavioral problems, including aggression.
In addition, persons with cognitive impairment and dementia often exhibit behaviors that are stressful for their care providers, and these disturbances are the most common reason for institutionalization.Reference Phillips and Diwan 1 There are several reasons for these behaviors—for example, a lack of understanding of their situation and communication problems, delusions and hallucinations, boredom because they cannot continue in pleasurable activities, and unmet needs.
Development of effective strategies for management of these behaviors is hindered by inconsistent and often contradictory terminology. Most confused terminology is related to agitation and aggression, which are two distinct constructs. It is problematic that most measurement scales for agitation do not take into consideration the circumstances of the behavioral symptoms. The terms “agitation” and “aggression” are sometimes conflated, such as in a definition of agitation that incorporates aggression.Reference Cummings, Mintzer and Brodaty 2 The current paper will demonstrate that agitation and aggression are two distinct syndromes and suggest how they can be differentiated and measured.
Definitions
Agitation
Numerous definitions of agitation have been offered:
A state of excessive psychomotor activity accompanied by increased tension and irritability. 3
Motor restlessness, heightened responsivity to stimuli, irritability, inappropriate and/or purposeless verbal or motor activity, decreased sleep, and fluctuation of symptoms over time. (p. 6)Reference Lindenmayer 4
Excessive motor or verbal activity (p. 2139).Reference Citrome and Volavka 5
Behaviors that communicate to others (who observe the patient) that the patient is experiencing an unpleasant state of excitement and that remain after interventions to reduce internal or external stimuli have been carried out.Reference Hurley, Volicer and Camberg 6
Aggression
Aggression is overt behavior of animals or humans involving intent to harm another organism or inanimate object.Reference Volavka 7 Many classifications of aggression exist. The phenomenological classification of human aggression defines four main groups: verbal aggression, physical aggression against other people, aggression against objects, and self-directed aggression (self-directed aggression is outside the scope of this review).
Classification based on motivation recognizes reactive and proactive aggression. Reactive aggression is an impulsive aggressive response to a perceived threat, loss, danger, or provocation, whereas proactive aggression is defined as behavior that anticipates a reward and involves planning and premeditation.Reference Gardner, Archer and Jackson 8 , Reference Miller and Lynam 9 Assaults in psychiatric patients can be motivated by such psychotic symptoms as delusions or hallucinations, personality features/psychopathy, or other factors alone or in combination.Reference Nolan, Czobor and Roy 10
In persons with advanced dementia, aggression develops most frequently when a caregiver provides care for a person who does not understand the need for it or misperceives the action as threatening, and resists the caregiver’s actions.Reference Ryden, Bossenmaier and McLachlan 11 If the caregiver persists, the person with dementia will defensively resist unwanted attention, become combative, and may strike the care provider. Thus, the behavior is evoked by an interaction with others and may result in reactive aggression. Such behaviors comprise “the repertoire of behaviors with which persons with dementia withstand or oppose the efforts of a caregiver.”Reference Mahoney, Hurley and Volicer 12
Violence denotes physical aggression among humans, and can thus be seen as a subtype of aggression (p. 2136).Reference Citrome and Volavka 5 “Hostility” is a loosely defined term that, in general, encompasses unfriendly attitudes among humans (p. 2).Reference Volavka 7 It may include temper tantrums, irritability, uncooperativeness, jealousy, suspicion, and other attitudes and behaviors.
Distinguishing agitation from aggression
On the basis of these definitions, we propose that the principal difference between agitation and aggression is this: agitation is excessive motor or verbal activity without any focus or intent, whereas aggression is a provoked or unprovoked behavior intended to cause harm. Aggression used in self-defense can be called “reactive aggression.”
Selected Assessment Instruments
There are many instruments developed over the years by clinicians working with adult psychiatric patients and elderly patients with dementia. A recent review evaluated 83 instruments developed to measure the behavioral and psychological symptoms of dementia.Reference van der Linde, Blossom, Dening and Brayne 13 In addition, we identified at least seven instruments that are employed in adult psychiatry, which are described below and in Tables 1 and 2. Some of these instruments measure many aspects of behavioral symptoms, while others measure just one or a few. Some instruments consist of a single item, for example, the Clinical Global Impression of Aggression, 14 Agitation Calmness Evaluation Scale, Reference Meehan, Zhang and David 15 and Behavioral Activity Rating Scale,Reference Swift, Harrigan, Cappelleri, Kramer and Chandler 16 and, therefore, cannot distinguish between agitation and aggression. We focused this review on composite scales that could provide some information about distinctions between agitation and aggression.
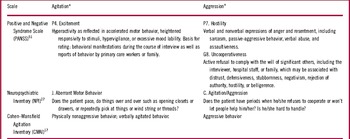
Table 1 Commonly used composite scales with items predominantly related to agitation or aggression
* Excessive motor or verbal activity without any focus or intent.
+ Provoked or unprovoked behavior intended to cause harm. Aggression used in self-defense can be called reactive aggression.
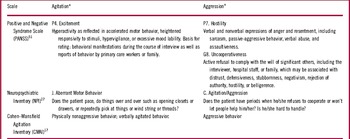
Table 2 Other composite scales that clearly separate agitation and aggression
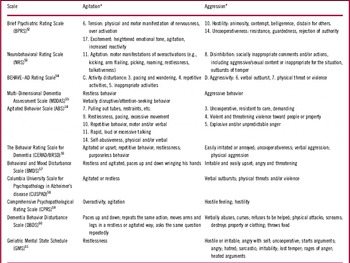
* Excessive motor or verbal activity without any focus or intent.
+ Provoked or unprovoked behavior intended to cause harm. Aggression used in self-defense can be called reactive aggression.
Composite scales
In most composite scales, it is possible to separate items that are predominantly related to agitation from other items predominantly related to aggression. When a total score is calculated, it reflects a combination of both syndromes and often other behavioral problems. We listed items related to agitation and aggression for each of the following types of scales:
1. scales that are currently most commonly used for the evaluation of agitation and aggression without clearly separating these two syndromes—for example, the Positive and Negative Syndrome Scale (PANSS), the Neuropsychiatric Inventory (NPI), or the Cohen–Mansfield Agitation Inventory (CMAI) (listed in Table 1); and
2. composite scales that clearly separate agitation and aggression; many of these scales are older and are not used frequently, but they represent the shared wisdom of generations of clinicians and researchers (Table 2).
Positive and Negative Syndrome Scale (PANSS)
Several individual PANSS items measure aspects of agitation and aggression. The PANSS Excitement item is closest to our definition of agitation (Table 1), and Hostility is a single item in the PANSS scale that reflects our definition of aggression. The Hostility item of the PANSS is rated on a severity scale ranging from 1 to 7. A rating of 1 indicates absence of hostility. A rating of 6 (severe) denotes “uncooperativeness and verbal abuse . . . patient may be violent,” and a rating of 7 (extreme) denotes “marked anger . . . or episode of physical assault.” Thus, these high severity scores imply a likelihood of aggression, and the Hostility item of the PANSS has been used as a proxy measure of aggression in a large number of psychopharmacological and other studies since the 1990s.Reference Volavka, Swanson and Citrome 17
The relationship between the PANSS Hostility item scores and overt physical aggression was studied in the patient set of the Clinical Antipsychotic Trials of Intervention Effectiveness (CATIE).Reference Lieberman, Stroup and McEvoy 18 For each unit increase on the 7-point Hostility item rating scale, the odds of serious aggression (or “violence”) detected with the MacArthur Community Violence InterviewReference Steadman, Mulvey and Monahan 19 were reported to increase by a factor of 1.65 (p<0.001).Reference Swanson, Swartz and Van Dorn 20 The results of a study examining the specific anti-hostility effects of clozapine using the PANSS Hostility itemReference Citrome, Volavka and Czobor 21 were consistent with an analysis from the same study that measured overt aggression.Reference Volavka, Czobor and Nolan 22
Uncooperativeness is another single item on the PANSS scale that reflects our definition of aggression. This item includes hostility, and the overlap is understandable, because uncooperativeness is a common trigger that may result in hostility.Reference Ryden, Bossenmaier and McLachlan 11
The PANSS Excited Component (PANSS–EC) is commonly used in studies of patients with agitation (see also the section on Regulatory Aspects, below). However, the PANSS–EC conflates agitation with aggression because it consists of the sum of the following five PANSS items: Excitement, Hostility, Tension, Uncooperativeness, and Poor Impulse Control. The PANSS–EC was first identified as a component of the PANSS by principal-component analysis of the PANSS scores of 240 schizophrenic inpatients.Reference Kay and Sevy 23 The PANSS–EC has been validated against other scales, and factor analysis confirmed its unifactorial structure.Reference Montoya, Valladares, Lizan, San, Escobar and Paz 24 Factor analysis of several studies of schizophrenia and mania patients has yielded a PANSS–EC with four items (Excitement, Poor Impulse Control, Hostility, and Uncooperativeness), which was used by others.Reference Huber, Hochstrasser, Meister, Schimmelmann and Lambert 25 A PANSS–EC with three items (Tension, Excitement, and Hostility) has also been utilized.Reference Swift, Harrigan, Cappelleri, Kramer and Chandler 16
The Cohen–Mansfield Agitation Inventory (CMAI)
The CMAIReference Cohen–Mansfield, Marx and Rosenthal 26 was designed on the basis of behavioral observations of 408 nursing home residents. Nurses used a 7-point scale to rate how often each resident manifested 29 agitated behaviors. Factor analysis yielded three syndromes of agitation: aggressive behavior, physically nonaggressive behavior, and verbally agitated behavior. The reliability and convergent validity of the CMAI in patients with Alzheimer’s disease have been published,Reference Koss, Weiner and Ernesto 27 and the scale has been widely used.
The manual for administration of the CMAI contains instructions regarding the questions that an interviewer should ask the caregiver about a patient’s behavior. The questions are limited to the observed behavior (e.g., hitting, kicking, pushing) without any attempt to explore the context in which such behaviors emerged.Reference Cohen–Mansfield 28
The Neuropsychiatric Inventory (NPI)
The NPIReference Cummings, Mega, Gray, Rosenberg-Thompson, Carusi and Gornbein 29 uses probing questions in 10 behavioral and two neurovegetative areas: delusions, hallucinations, agitation/aggression, depression/dysphoria, anxiety, elation/euphoria, apathy/indifference, disinhibition, irritability/lability, aberrant motor behavior, sleep and nighttime behavior disorders, and appetite and eating disorders. If an answer to probing questions is positive, the severity of this symptom is further evaluated. 30
The NPI is currently considered the gold standard in research related to the behavioral symptoms of dementia, but it has several shortcomings. The first is that it combines agitation and aggression in a single item: “agitation/aggression.” The probing questions for this item are: ”Does the patient have periods when he/she refuses to cooperate or won’t let people help him/her?” and “Is he/she hard to handle?” It therefore measures rejection of care. Rejection of care may result in combativeness and reactive aggression, but it does not fit our definition of agitation.
Agitation is reflected mostly in the area called “aberrant motor behavior,” but the questions included there do not include verbal agitation. An analysis of the NPI structure yielded conflicting data,Reference Aalten, Verhey and Boziki 31 but an analysis of data from the CATIE study clearly differentiated aggressiveness and aberrant motor behavior.Reference Nagata, Shinagawa and Nakajima 32
Other scales that differentiate agitation and aggression are listed in Table 2.
Scales measuring just one syndrome
Scale for Observation of Agitation in Persons with DAT (SOAPD)Reference Hurley, Volicer and Camberg 6
The SOAPD was developed by an examination of existing scales and articles related to agitation in Alzheimer’s disease. It started with 47 discrete behaviors that were reduced to 23 and used to develop a 7-item scale measuring body movements and vocalizations. This scale used the magnitude of estimated scaling to generate the weights of different observed symptoms for the total score, and it has demonstrated good interrater reliability. A principal-components factor analysis yielded two factors: three verbal items and four physical items. Detailed descriptions and forms are available.Reference Volicer and Hurley 33
MacArthur Community Violence Interview
The MacArthur Community Violence Interview was designed for and first utilized in the MacArthur Violence Risk Assessment Study.Reference Steadman, Mulvey and Monahan 19 Subjects (discharged psychiatric patients) and collateral informants were asked whether the subject had in the previous 10 weeks engaged in “violence” (defined as any assault using a lethal weapon or resulting in injury, any threat with a lethal weapon in hand, or a sexual assault), or other (less serious) aggressive acts.
Rejection of Care in Dementia (RTC–DAT)
The RTC–DATReference Mahoney, Hurley and Volicer 12 is distinct from related concepts such as agitation and is psychometrically sound. The RTC–DAT has detected differences in rejection of care during bathing and morning activities of daily living. It requires 5-minute observations during an activity and is scored for the duration of the behavior (0–4) and its intensity (1–3). Item severity score is obtained by multiplying duration and intensity scores, and the final score is the sum of item severity scores (range 0–156). The RTC–DAT was employed in research investigating “elderspeak” communicationReference Williams, Hermann, Gajweski and Wilson 34 and strategies for providing morning oral care.Reference Hammar, Emami, Gottel and Engstrom 35 A detailed description and forms for the RTC–DAT are available.Reference Volicer and Hurley 36
Scales for the assessment of trait aggressiveness
Several scales assessing the life history of aggression exist.Reference Brown, Goodwin, Ballenger, Goyer and Major 37 , Reference Coccaro, Berman and Kavoussi 38 These details can be found elsewhere.Reference Volavka 7
Regulatory aspects
Several agents have received approval by the U.S. Food and Drug Administration (FDA) and other regulatory bodies for the treatment of agitation associated with schizophrenia or bipolar mania.Reference Citrome 39 , Reference Citrome 40 However, none of these medications have been approved for patients with dementia. In addition, there are no agents specifically approved for the treatment of aggression.
Historically, the accepted primary outcome measures for studies of interventions to address agitation have evolved from the single-item Behavioral Activity Rating Scale used in the development of intramuscular ziprasidone (leading to its approval for the treatment of agitation associated with schizophrenia), to the PANSS–EC, where change from baseline at 2 hours postadministration was used to support the approval of intramuscular olanzapine, intramuscular aripiprazole, and inhaled loxapine for agitation associated with schizophrenia or bipolar mania.
Change in CMAI total score from baseline to week 12 is currently being used as the primary outcome measure in phase III clinical trials of brexpiprazole for agitation associated with dementia of Alzheimer’s type (MacArthur Community Violence Interview, NCT01862640), change to week 10 in a phase III clinical trial of aripiprazole for the identical indication (NCT02168920), and change from baseline to week 4 in a phase III clinical trial of ITI–007 for agitation in patients with dementia, including Alzheimer’s disease (NCT02817906). Change in the NPI “agitation/aggression” domain from baseline to week 12 is currently being used as the primary outcome measure in phase III clinical trials of AVP–786 for agitation associated with dementia of Alzheimer’s type (NCT02442765, NCT02442778).
Clinical Observations
In individual adult psychiatric patients, we can observe agitation without aggression, aggression appearing as an extreme form of agitation, or aggression alone. Agitation can escalate into aggression, and thus appropriate management of agitation can be seen as prevention of this form of aggression.Reference Citrome and Volavka 41
This classification leaves out some important environmental and motivational aspects involving agitation and aggression in mental illness. What is seen as agitation may in many cases in fact be resistance to care, which is a defensive reaction. This has been clearly demonstrated in dementia patients.Reference Ryden, Bossenmaier and McLachlan 11
Similar to adult psychiatric patients, by distinguishing aggression and agitation, it is possible to separate persons with dementia into three groups—persons exhibiting: agitation only, aggression only, and both agitation and aggression. Pure agitation and aggression have different relationships with severity of dementia.Reference Volicer, Bass and Luther 42 While agitation may be present even in mild dementia and its prevalence does not increase with dementia severity, aggression starts occurring in moderate dementia and increases together with increasing communication deficit. Some persons with dementia exhibit both agitation and aggression but not at the same time. Agitation and aggression do share some commonalities in terms of risk—for example, depression is a risk factor for the development of both agitation and aggression.Reference Volicer, Frijters and van der Steen 43 , Reference Galindo-Garre, Volicer and van der Steen 44
It is possible that a similar situation develops in some cases of apparent aggression or agitation in general psychiatric adult patients. Ward staff and inpatients at a forensic psychiatric unit were separately asked about reasons for assaults on the unit.Reference Harris and Varney 45 The most frequent reason given by the staff was that the patient was “ordered to do something.” We know that many such orders (e.g., a request for a patient to take a bath or take medication) are related to care. More investigations like this need to be undertaken, and appropriate instruments assessing environmental effects and patients’ motivations relating to agitation and aggression should be developed. Some of the instruments available today are not helpful in this respect (see Table 1). For example, the NPI mislabels a patient’s rejection of care as “agitation/aggression.”Reference Volicer 46 Such misunderstandings are a source of confusion in the literature.
It is important to distinguish agitation and aggression because their management requires different strategies. In persons with dementia, agitation is ameliorated by meaningful activities,Reference Cohen–Mansfield, Marx, Dakheel-Ali, Regier, Thein and Freedman 47 while reactive aggression caused by rejection of care is best managed by modification of care procedures—for instance, substituting bed bath for tub or shower bath.Reference Sloane, Honn, Dwyer, Wieselquist, Cain and Meyers 48 Among persons with schizophrenia, episodes of aggression can be influenced by several factors, including impulsivity, psychopathy, and psychosis, with agitation not a necessary prerequisite.Reference Volavka and Citrome 49 Thus, the appropriate interventions will be dependent on the main drivers for the behavior for that individual patient at that point in time.
We propose that, in studies that investigate different strategies for management of behavioral symptoms of dementia and challenging behaviors in persons with psychotic conditions, the outcomes should be evaluated separately for agitation and aggression. This is especially important for investigation of drug effectiveness because combining both syndromes can lead to incomplete information about drug effectiveness (the medication may be effective against one syndrome and not the other), and this information will be lost in summary scores of combined syndromes, causing the study to be negative. In addition, calling all behavioral symptoms of dementia “agitation” may lead to indiscriminate use of antipsychotics that are effective in decreasing aggression but have a limited impact on the symptoms of agitation.Reference Ballard and Corbett 50
This has important implications for drug development, particularly for persons with dementia, where there are at present no FDA-approved options for the treatment of agitation or aggression.Reference Garay, Citrome, Grossberg, Cavero and Llorca 51 Since several studies investigating the effects of medications on the behavioral symptoms of dementia used the NPI to assess outcomes, there is a danger that “agitation/aggression” may become the indication for the use of new medications.Reference Soto, Abushakra and Cummings 52 That would perpetuate the current confused nomenclature of behavioral symptoms, because effectiveness assessed with the “agitation/aggression” item is actually effectiveness against rejection of care, which may result in reactive aggression, and which is separate from agitation itself. It would be important to measure not only the effect on the “agitation/aggression” item, but also on the “aberrant motor behavior” item, which reflects the actual level of agitation. This separation would also be in agreement with MDS 3.0 evaluation of behaviors, which clearly separates behavioral symptoms not directed toward others (agitation), and physical and verbal behavioral symptoms directed toward others53 that could be characterized as aggression.
Conclusions
Psychosis in adulthood and dementia in the elderly differs in terms of pathophysiology and course. Nevertheless, agitation and aggression may develop in either condition. Agitation in psychosis is phenomenologically similar to that observed in dementia, and the same applies to aggression (e.g., hitting, kicking, pushing). However, agitation and aggression are two distinct syndromes. This should be recognized in drug development trials in both psychiatric and dementia patients.
Many scales have been developed to assess these behavioral disturbances in psychosis and in dementia. Most of the scales commingle agitation and aggression in a final or summary score. Furthermore, the motivation and environmental circumstances of aggression have been largely ignored in available scales. This contrasts with the increasing evidence that resistance to care is an important cause of reactive aggression in dementia. Resistance to care that gives rise to conflicts is also a clinically important issue in the management of psychosis in adulthood, but this problem has been underresearched. Recognition of distinction between agitation and aggression would promote more detailed investigations and the development of better pharmacological and nonpharmacological treatment strategies.
Disclosures
Ladislav Volicer and Jan Volavka hereby state that they have nothing to disclose. Leslie Citrome reports personal fees from Acadia, Alexza, Alkermes, Allergan, Avanir, Boehringer Ingelheim, Bristol-Myers Squibb, Eli Lilly, Forum, Genentech, Janssen, Jazz, Lundbeck, Merck, Medivation, Mylan, Neurocrine, Novartis, Noven, Otsuka, Pfizer, Reckitt Benckiser, Reviva, Shire, Sunovion, Takeda, Teva, Valeant, and Vanda; personal fees from Acadia, Allergan, Alkermes, AstraZeneca, Avanir, Bristol-Myers Squibb, Eli Lilly, Forum, Janssen, Jazz, Lundbeck, Merck, Novartis, Otsuka, Pfizer, Shire, Sunovion, Takeda, and Teva; and others from Bristol-Myers Squibb, Eli Lilly, J&J, Merck and Pfizer outside the submitted work.