Introduction
Depression is a frequent complication of eating disorders (EDs) and eating disturbances are common manifestations of depressive illness. The nature of the relationship, however, has been a source of controversy. A shared etiology postulates a common set of risk factors leading to the development of both EDs and depression.Reference Puccio, Fuller-Tyszkiewicz and Ong1 Mood disorder onset might precede, follow, or develop simultaneously to the ED,Reference Godart, Radon and Curt2 suggesting the need of specifically evaluating the individual case.
Diagnosis of depression in EDs constitutes a difficult task. Not surprisingly, comorbidity rates of major depressive disorder (MDD) display wide fluctuations from 40% to 80%Reference Godart, Radon and Curt2, Reference Godart, Perdereau and Rein3 and lack predictive value as to response to antidepressant therapy.Reference Mischoulon, Eddy and Keshaviah4 Overlapping symptomatology, such as excessive weight loss, over-eating, sleep disturbance, fatigue, irritability, concentrating difficulties, and poor memory,Reference Meehan, Loeb and Roberto5, Reference Mattar, Huas and Duclos6 may account for inflated depression diagnoses in this clinical population.Reference Garfinkel and Garner7, Reference Casper8
It has been suggested that exclusive reliance on conventional diagnostic classification systems may not provide sufficient clinical information, and assessment may benefit from additional sources of information.Reference Fava, Rafanelli and Tomba9 One source derives from expanding collection of symptoms to clinical manifestations that frequently occur in the longitudinal development of mood disorder.Reference Fava10 The Clinical Interview for DepressionReference Paykel11, Reference Guidi, Fava and Bech12 is uniquely suited for capturing such manifestations. Another important element of the clinical process comes from the concept of demoralization,Reference Fava, Freyberger and Bech13, Reference Fava, Cosci and Sonino14 a feeling state characterized by the perception of being unable to cope with some pressing problems and/or of lack of adequate support from others.Reference Tecuta, Tomba and Grandi15 Demoralization, seldom investigated in EDs,Reference Abbate-Daga, Delsedime and Nicotra16 may co-occur with major depression or be independentReference Tecuta, Tomba and Grandi15 and is associated with adverse health outcomes and poor quality of life. Finally, a neglected area in assessment is psychological well-being, despite the availability of validated instruments and its growing importance in establishing resilience. Dimensions of positive functioning were found to affect the complex balance between positive and negative affects both in moodReference Fava, Cosci and Guidi17 and eatingReference Tomba, Offidani and Tecuta18, Reference Tomba, Tecuta and Schumann19 disorders.
The aim of the current study was to broaden the evaluation of depressive symptomatology in EDs with instruments that capture clinical phenomena such as demoralization and subclinical distress and to examine their associations with dimensional measures of psychological well-being. More specifically, the study aimed to provide a comprehensive and innovative assessment of mood in EDs, capturing not only traditional psychiatric disturbances such as depression but also subclinical manifestations and psychological states such as demoralization. We hypothesize that a subset of ED patients exhibits demoralization syndrome in the absence of major depression and vice versa. In addition, we hypothesize that demoralization is associated with significant distress and impaired positive functioning.
Methods
Participants
Consecutively recruited patients (n = 81) who met Diagnostic and Statistical Manual of Mental Disorders 5 (DSM-5) criteria for EDs,Reference First, Williams and Karg20 anorexia nervosa (AN), bulimia nervosa (BN), binge-eating disorder (BED), and other specified feeding or eating disorder (OSFED) were recruited from specialized ED treatment centers, Centro Gruber and Residenza Gruber (Bologna, Italy), before commencing treatment. ED diagnoses were established at intake by the consensus of a psychiatrist and a clinical psychologist independently using the Structured Clinical Interview for DSM-5 (SCID).Reference First, Williams and Karg20 With the exception of two patients who refused to participate, all invited patients took part in the study (n = 79).
Ethical review committees of the Centro Gruber and Residenza Gruber in Bologna, Italy, approved the study and all patients provided written informed consent after the procedures were explained to them.
Measures and clinical variables
The evaluation was performed during routine assessment visits. Participants underwent detailed clinical interviews by a trained clinical psychologist and completed several self-rating questionnaires for the assessment of distress and psychological well-being. Data were collected between April 2016 and October 2017.
(1) Depressive disorder diagnoses were obtained using the SCIDReference First, Williams and Karg20 for depressive disorders. For a diagnosis of major depression, patients had to exhibit five out of eight symptoms one of which was depressed mood or loss of interest or pleasure. The criterion of significant weight gain or loss or change in appetite was excluded as ED patients exhibit changes in weight and appetite in accordance with ED disorder diagnosis. For a diagnosis of persistent depressive disorder, in addition to depressed mood for most of the day, for more days than not for 2 years, the patients had to exhibit at least two additional symptoms, with the exception of poor appetite or overeating.
(2) Depressive symptoms were assessed with the change version of the Clinical Interview for Depression 20-item interview,Reference Paykel11, Reference Guidi, Fava and Bech12 a dimensional observer-rated assessment instrument which consists of an expanded version of the Hamilton Rating Scale for Depression.Reference Hamilton21 The interview covers 20 symptom areas. In this modified version, two items concerning appetite and weight gain/loss (items 12 and 13) were omitted due to the potentially confounding aspects of ED-related symptomatology. Each item is rated on a 1–7 point scale, with 1 indicating the absence of symptoms and 7 severe incapacitating manifestations. A score of 3 or above in the individual items was considered the cut-off for the presence of the symptom. The scale encompasses a wide range of symptoms (such as irritability and phobic anxiety) compared to other scales and is particularly suitable to assess subclinical symptoms of mood disorders.Reference Fava10, Reference Guidi, Fava and Bech12, Reference Bech22 One item concerning reactivity to social environment, selected from the full version of the CID, was added to the 18 items.
(3) Demoralization diagnosis was obtained using The revised Structured Interview for the Diagnostic Criteria for Psychosomatic Research (DCPR)-Demoralization Criteria.Reference Fava, Cosci and Sonino14 Diagnoses were formulated independently of DSM diagnostic findings. Items of the interview for DCPR are scored through a yes/no response format. The structured interview has demonstrated high inter-rater reliability, and Cohen’s kappa for demoralization was found to be 0.90.Reference Galeazzi, Ferrari and Mackinnon23 The revised DCPR criteriaReference Fava, Cosci and Sonino14 allow differentiation of two expressions of demoralization: helplessness (the individual maintains the capacity to react, but lacks adequate support) and hopelessness (when the individual feels he/she alone is responsible for the situation and there is nothing he /she or anyone else can do to overcome the problem).
(4) Self-report depressive symptoms were assessed with the Beck Depression Inventory II (BDI-II)Reference Beck, Steer and Brown24 a 21-item questionnaire. A total score ranging 0–63 indicates depression severity with higher total scores indicate more severe depressive symptoms. Composite scales of cognitive and somatic-affective symptoms were calculated.Reference Wang and Gorenstein25
(5) Positive functioning was evaluated with the Psychological Well-being Scales – PWB,Reference Ryff26, Reference Ryff27 an 84-item self-rated questionnaire that covers six inter-related areas of psychological well-being which allow the development of optimal functioning: autonomy, environmental mastery, personal growth, positive relations with others, purpose in life, and self-acceptance. Items are constructed on a six-point 1–6 Likert scale, yielding six subscale scores ranging from 14 to 84. Subscale scores range from 0 to 98 with higher scores indicate greater psychological well-being in specific dimensions.
(6) ED symptomatology was assessed with the Eating Attitudes Test-40,Reference Garner and Garfinkel28, Reference Garfinkel and Newman29 a 40-item screening measure identifying behaviors and cognitive patterns of EDs. Items are constructed on a 0–3 four-point Likert scale, yielding three subscale scores for dimensions of dieting, body, and food preoccupation, oral control, and a total score ranging from 0 to 120. Higher scores indicate greater ED psychopathology.
In addition to administering these clinical scales, Body mass index (BMI), illness duration in months, and type of antidepressant therapy were collected from the medical records.
Data analysis
Descriptive analyses were run for frequency of CID-rated specific depression symptoms and frequencies of demoralization and depressive illness (persistent depressive disorder and MDD) in the total sample. Univariate analyses of variance using the general linear model were performed to test for associations between DSM-5 Depressive Disorders and the DCPR-based classification of demoralization and average scores on dimensional psychological measures after controlling for illness duration. DSM-5 and DCPR-based diagnoses were examined separately. For all tests performed, the significance level was set at 0.05, two-tailed. In view of the exploratory nature of the investigation, adjustment for multiple testing was not performed. Age, educational level, and BMI were not significantly correlated with any outcome variable and were therefore excluded from analyses.Reference Miller and Chapman30
Results
ED patients characteristics
The patient response rate was high with 97.53% (n = 79) of ED outpatients out of 81 agreeing to participate (see Table 1 for descriptive socio-demographic and clinical data). Data on specific depression symptoms through CID interview were available for 72 patients. The 79 ED patients were all female with mean age 28.83 ± 11.25 years, range 15–58 years, and mean educational years 14.44 ± 3.15. About half, 53.2% (n = 42), were outpatients and the remaining 46.8% were inpatients (n = 37). Outpatients and inpatients did not differ significantly in main socio-demographic characteristics, that is age, education, or in BMI. They differed significantly in illness duration (p = 0.04) with inpatients reporting longer length of illness (11.69 ± 9.02 years) compared to outpatients (7.49 ± 8.96 years). Almost a third (n = 22, 27.8%) of patients were currently on antidepressants, the most common being selective serotonin-reuptake inhibitors (n = 18). Inpatient and outpatient groups did not differ significantly in severity (BDI and CID total scores) of depression. Diagnostic subgroups (AN, BN, BED, and OSFED) also did not differ in severity of depression. See Table 1.
TABLE 1. Socio-demographic characteristics of ED patient sample (n = 79)

Note. AN, anorexia nervosa; BED, binge-eating disorders; BN, bulimia nervosa; and OSFED, Other-specified feeding or eating disorder.
* Pearson Chi-squared.
+ T-test for independent samples.
Frequency of depressive symptoms in ED patients
The most common CID depressive symptoms in the ED sample (n = 72) were feelings of guilt, environmental reactivity, depressed mood, and low energy or fatigue, which were present in about two-thirds of the sample. Please see Table 2 for frequencies of these and of other depressive symptoms.
TABLE 2. Frequency of depression symptoms (CID items) in ED patients (n = 72)

Note. CID, Clinical Interview for Depression.
Relationship of DSM depression diagnoses and DCPR demoralization
Diagnoses are displayed in Figure 1. Nineteen patients (24.0%) were without any mood-related comorbidity (i.e., unaffected). A fifth of patients reported only demoralization (20.3%), 12 with helpless demoralization, and 4 cases of hopeless demoralization. In terms of DSM-defined diagnoses, comorbid persistent depressive disorder was reported by 16.5% of the patients, while MDD was the most prevalent (39.2%). Demoralization overlapped partially with both persistent depressive disorder and MDD. None of the unaffected ED patients and about half (n = 16) of the comorbid MDD group were on antidepressant medications. Three demoralized and four ED patients with persistent depressive disorder were also on antidepressants.

FIGURE 1. Prevalence of demoralization subtypes, persistent depressive disorder, and major depression in ED patients.
Notes: DCPR, Diagnostic Criteria for Psychosomatic Research; ED, eating disorder; MDD, major depressive disorder.
Associations between DSM 5 Depressive Disorders and dimensional psychological variables
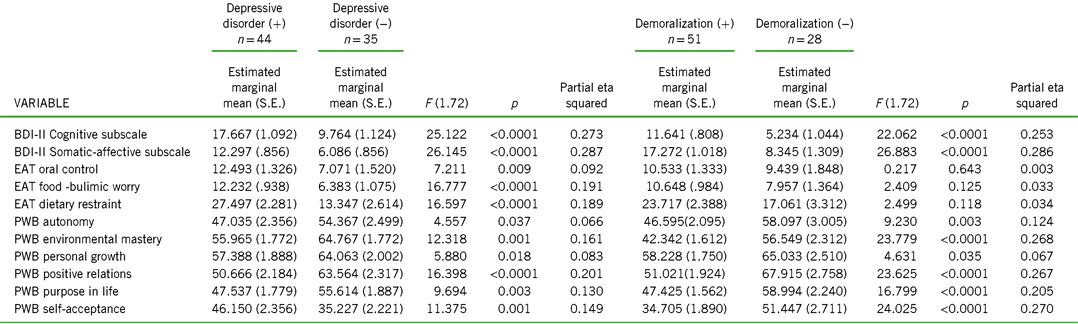
According to univariate analyses of variance comparisons, comorbid depressive disorder (MDD or persistent depressive disorder) was associated with significantly greater distress in terms of depressive symptoms in BDI-II as well as in EAT-eating-related pathology, including oral control, food and bulimic worry, and dietary restraint. In terms of psychological well-being, presence of a depressive illness was associated with significantly worse functioning in PWB dimensions of environmental mastery, positive relations with others, purpose in life, and self-acceptance. Table 3 displays the comparisons between ED patients with and without comorbid DSM depressive illness.
TABLE 3. Associations of DSM-5 depressive disorders and DCPR-based demoralization with dimensional psychological measures (n = 79)

Note. (+) Disorder or syndrome present; (−) Disorder or syndrome absent; BDI-II, Beck Depression Inventory II; EAT, Eating Attitudes Test; PWB, Psychological Well-Being scales.
Associations between DCPR demoralization and dimensional psychological variables
Univariate analyses of variance yielded some significant associations between diagnoses formulated according to the DCPR-based demoralization and dimensional psychological variables. Demoralization diagnosis in ED patients was also associated with significantly greater distress in terms of BDI-II scores but not in terms of EAT-eating-related pathology, in which no significant differences between demoralized and non-demoralized ED patients emerged. Nonetheless, in PWB dimensions of psychological well-being, occurrence of demoralization was associated with significantly worse functioning in environmental mastery, positive relations with others, purpose in life, and self-acceptance. Table 3 illustrates the comparisons between demoralized and non-demoralized ED patients.
Discussion
Despite some limitations of the current study, namely the small sample size and cross-sectional design, the joint use of a comprehensive clinical interview for depressionReference Paykel11, Reference Guidi, Fava and Bech12 with the DSM diagnostic criteriaReference First, Williams and Karg20 and demoralization and psychological well-being assessment has yielded important clinical insights into mood disturbances in EDs.
First, diagnostic criteria place particular emphasis on a specific set of symptoms within a certain symptomatology. Such priority, however, does not necessarily apply to a setting of comorbidity, where other symptoms may be prominent and characteristic. The innovativeness of the applied assessment approach resides in the use of the clinimetric approach. Clinimetrics refers to clinically relevant information frequently ignored by traditional psychiatric approaches such as patterns of symptoms, severity of illness, effects of comorbid conditions, timing of phenomena, rate of progression of illness, functional capacity, and other aspects such as positive functioning. The use of a macro-analytic evaluation using clinician-rated scales such as the CID and DCPR, followed by the use of a micro-analysis of specific symptoms through self-rating scales, allows to capture subclinical symptoms, which would have been otherwise undetected.Reference Fava, Rafanelli and Tomba9 Using the CID, the most common depression symptoms in EDs were depressed mood, feelings of guilt, and abnormal reactivity to social environment. Guilt has been found to be exceedingly common in ED patients, not globally, but in particular, in relation to eating and eating behaviorsReference Frank31, Reference Petry, Vasconcelos and Costa32 and in relation to body shame.Reference Burney and Irwin33 Moreover, it has been found to persist throughout the recovery process from the disorder.Reference Frank31 Reactivity to social environment refers to the changes in mood and symptomatology, as a result of environmental circumstances, either improvement or worsening. It has been found to characterize cyclothymiaReference Tomba, Rafanelli and Grandi34 and to be prevalent in the prodromal phase of BN compared to unaffected controls.Reference Raffi, Rondini and Grandi35 Recent studies on emotional reactivity in EDsReference Tapajóz, de Sampaio and Soneira36 suggest that such reactivity in AN and BN might be related to social situations in which patients are pressured to consume high-calorie food, evoking states of anxiety, and depression.Reference Gutiérrez-Maldonado, Ferrer-García and Caqueo-Urízar37
Anxiety, whether generalized, somatic or phobic, was also found to be very common. Studies have shown that anxiety symptomatology is often comorbid and may precede EDs.Reference Swinbourne and Touyz38 More specifically, EDs have been found to be associated with body anxiety, eating and food preoccupations, pre-meal anxiety,Reference Steinglass, Albano and Simpson39 and avoidance behaviors relating to food, body, and interpersonal situations.Reference Arkell and Robinson40, Reference Bamford, Attoe and Mountford41 Indeed, recent research explores the efficacy of exposure therapy and response prevention in the treatment of AN.Reference Steinglass, Albano and Simpson42
Figure 1 illustrates the complexity of mood assessment in EDs. Using DCPR criteria, 20% of patients met the criteria for demoralization. Such patients would not be identified using DSM criteria only. The percentage of demoralization cases is in line with varying prevalence rates in the medical and psychiatric setting.Reference Tecuta, Tomba and Grandi15 In EDs, a previous study which had not taken into account a possible overlap with major depression and dysthymic disorder had reported higher rates.Reference Abbate-Daga, Delsedime and Nicotra16 Interestingly, cases of demoralization in the absence of depressive disorder were mostly of the helpless subtype.
Associations of DCPR demoralization with dimensional psychological measures provide further support to its validity and utility. Consistent with previous studies,Reference Tecuta, Tomba and Grandi15, Reference Grandi, Sirri and Tossani43 demoralization was found to be associated with lower psychological well-being and greater distress. Moreover, the same number of significant associations was found between demoralization and depressive illness and psychological variables, with the exception of ED-related symptoms, which were not associated with demoralization. Findings lend support to the hypothesis that DCPR demoralization might be suitable for classifying psychological distress in EDs that is not confounded by the ED symptoms themselves. Indeed, demoralization does not seem to depend on illness type or severity, affecting a wide range of psychiatric and medical illnesses alike.Reference Tecuta, Tomba and Grandi15
Subjective incompetence (a feeling of being trapped or blocked because of a sense of inability to plan or start actions toward goals) is a major component of demoralization.Reference de Figueiredo44, Reference de Figueiredo45 Such feelings of inadequacy and low self-efficacy have been previously documented in EDs.Reference Garner46, Reference Surgenor, Maguire and Russell47 Individuals, who perceive themselves as incompetent are uncertain and indecisive as to their directions, display high reactivity to environmental stimuli and low psychological well-being. Not surprisingly, patients with EDs were found to present with very high rates of dropout.Reference Fassino, Pierò and Tomba48
In both standard assessment and treatment approaches, most studies focus on pathological symptomatology and its reduction, as well as modifications of physical and behavioral aspects, ignoring gains in positive aspects such as quality of life and psychological well-being.Reference Tomba, Offidani and Tecuta18, Reference Tomba, Tecuta and Schumann19, Reference Ackard, Richter and Egan49 The pursuit of euthymia, defined as how the individual adjusts the psychological dimensions of well-being to changing needs, may thus become one of the targets of treatment. Such positive functioning characteristics have been found to be persistently compromised in various psychiatric illnesses including EDsReference Tomba, Offidani and Tecuta18 and their impairments are correlated with increased vulnerability to future adversity and may thus be a viable psychotherapeutic target.Reference Jahoda50–Reference Fava53
The high comorbidity rates found in the current study between EDs and depression are in line with those in the literature, ranging from 40% to 80%, as well as high comorbidity rates with dysthymic disorder which surpass those found in the general population.Reference Godart, Radon and Curt2–Reference Mischoulon, Eddy and Keshaviah4 In the current study, depressive disorders were associated with worse overall functioning in terms of both psychological distress and well-being, a result that is in line with the literature. Depressed ED patients exhibit greater dietary restriction, body dissatisfaction, and worse quality of life,Reference Padierna, Quintana and Arostegui54 socialReference Hatsukami, Mitchell and Eckert55and global functioning compared to unaffected ED patients.Reference Bulik, Sullivan and Carter56–Reference Brand-Gothelf, Leor and Apter58 Moreover, it is well-documented that ED severity is significantly associated with severity of the depression.Reference Herpertz-Dahlmann and Remschimdt59
As expected, an overlap between the demoralization and depressive illness was found, as in other medical psychiatric populations.Reference Tecuta, Tomba and Grandi15
Clinical guidelines for the screening of depression in EDs recommend the Beck Depression Inventory-II and the Hamilton Depression Rating Scale.Reference Anderson, Lundgren and Shapiro60, Reference Bowers, Haedt-Matt, Preedy, Watson and Colin61 However, such standardized screening measures mainly based on DSM criteria might not be sufficient in such a complex clinical population with frequent medical complications.
Conclusion
The presence of demoralization syndrome in EDs is undoubtedly relevant to treatment and recovery from EDs. Hopelessness and helplessnessReference Waller62 and poor self-efficacyReference Wade, Wilksch and Paxton63, Reference Dawson, Rhodes and Touyz64 have been identified by ED patients themselves as barriers to change and recovery in qualitative studies. In chronic AN patients, the recovery process may be hindered by feelings of hopelessness and “feeling stuck.”Reference Nordbø, Espeset and Gulliksen65 Indeed, demoralization has been found to affect response to psychotherapy.Reference Frank66, Reference Tomba, Tecuta and Guidi67
Moreover, the clinical utility of depression diagnoses in ED populations is called into question by treatment trials. Depression comorbidity in EDs has an unclear role in treatment response with inconsistent results across ED categories.Reference Agras, Walsh and Fairburn68, Reference Collin, Power and Karatzias69 For instance, inconclusive or mixed findings have been reported for FDA-approved fluoxetine in BN70–Reference Romano, Halmi and Sarkar72 with lack of improvement in AN.Reference Walsh, Kaplan and Attia73 Antidepressants in ED patients were devoid of impact on likelihood and persistence of recovery from MDD in a longitudinal study.Reference Mischoulon, Eddy and Keshaviah4
Fava, Rafanelli, and TombaReference Fava, Rafanelli and Tomba9 have advocated that exclusive reliance on diagnostic criteria has impoverished the clinical process in psychiatry. Customary clinical taxonomy in psychiatry does not include clinical distinctions that demarcate major prognostic and therapeutic differences among patients who otherwise seem to be deceptively similar since they share the same psychiatric diagnosis.Reference Fava, Rafanelli and Tomba9 This investigation has illustrated how a broader perspective in evaluation of mood disturbances in EDs may lead to an individualized assessment of the complex balance between euthymia, dysthymia, and eating behavior which may entail important treatment implications. Further studies, using a comprehensive clinimetric approach,Reference Fava, Carrozzino and Lindberg74 with larger samples and a longitudinal design, are needed.
Funding
This research received no specific grant from any funding agency, commercial, or not-for-profit sectors.
Disclosures
Lucia Tecuta, Giovanni Andrea Fava, and Elena Tomba have nothing to disclose.