Ventricular septal defect (VSD) is the most common type of congenital heart defect, and is responsible for approximately 32% of all heart defects diagnosed during the first year of postnatal life. Reference Axt-Fliedner, Schwarze, Smrcek, Germer, Krapp and Gembruch1 VSD can occur sporadically or in association with TBX5 and GATA4 gene mutations, and is commonly associated with other congenital anomalies. Reference Bravo-valenzuela, Peixoto and Araujo Júnior2 Foetal cardiac anomalies can be found in patients with no identifiable risk factors, and therefore examination of the foetal heart is an integral part of routine obstetric ultrasound. Reference Todros, Capuzzo and Gaglioti3
Echocardiographic prenatal diagnosis of congenital heart defects such as VSD is challenging. It requires a team of specialists and subspecialists as well as sonographers. Moreover, the sensitivity of detection is highly variable and depends on many factors such as operator experience, gestational age, and the position of the foetus. This can result in patients with clinically significant CHDs being missed, as approximately 10–30% of patients who die from CHD are undiagnosed until autopsy. Reference Graham4
To combat this, pulse oximetry measurements can be utilised in order to aid the identification of newborns who may benefit from early treatment of CHD. This is a painless and easily accessible examination that can be effortlessly fitted into the assessment of newborns. It is used to measure the capillary concentration of oxygen-saturated haemoglobin in an extremity, and the reading is expressed as a percentage. Reference Ewer5
Surgical intervention may be required if the infant fails to gain weight and develop adequately, or symptoms of heart failure develop requiring pharmacological treatment. Reference Fu6 Traditionally, treatment for large muscular VSDs consisted of open surgical closure, through sternotomy (an incision made in the middle of the sternum giving access to the heart), with cardiopulmonary bypass. The defect is usually accessed through the atrioventricular or semilunar valves, and this has the benefit of avoiding the need for ventriculotomy. Reference Penny and Vick7 Potential complications of open surgery include complete heart block, residual VSD, neurologic injury, or even death. Reference Graham8 New minimally invasive techniques of VSD repair have increasingly become a viable management option. This eliminates the need for cardiopulmonary bypass and can potentially decrease the length of recovery and hospital stays.
Aim of this study
The primary aim of this literature review is to explore and discuss existing diagnostic and therapeutic options for neonatal ventricular septal defects.
Methodology
Search strategy and selection
Using the search strings “Congenital VSD diagnosis”, “Congenital VSD screening”, “congenital VSD management”, and “congenital VSD treatment” on Scopus, PubMed, and MEDLINE, 115 articles were initially identified following PRISMA guidelines. These databases were used as they are large and easily accessible. The references of studies found were also searched to identify additional studies that may be of interest. It was decided to use these search strings as they allowed the acquisition of an appropriate number of papers whilst also ensuring the results were narrowed down and relevant to the aims of the review.
The eligibility criteria utilised for this review were as follows:
-
Studies published within the last 10 years (2010–2020).
-
Any study design including randomised control trials, non-randomised control trials, prospective or retrospective cohort studies, or systematic reviews.
-
Studies focusing on diagnostic investigations for VSD, and studies comparing transcatheter versus open surgical closure of defects.
Specific exclusion criteria were used in order to further reduce the numbers of papers, and these were as follows:
-
Age – papers more than 10 years old were automatically excluded.
-
Language – the paper must be in English, and not require translational services.
-
Content – the paper must have a specific focus on the effectiveness of either the screening, diagnosis, or treatment processes.
The utilisation of the inclusion and exclusion criteria was followed by a manual analysis of the remaining papers, in order to deem if relevant to include in the analysis.
Results
Searches of relevant databases and application of inclusion and exclusion criteria resulted in 24 papers being eligible. Ten of these papers were selected for analysis and in-depth review.
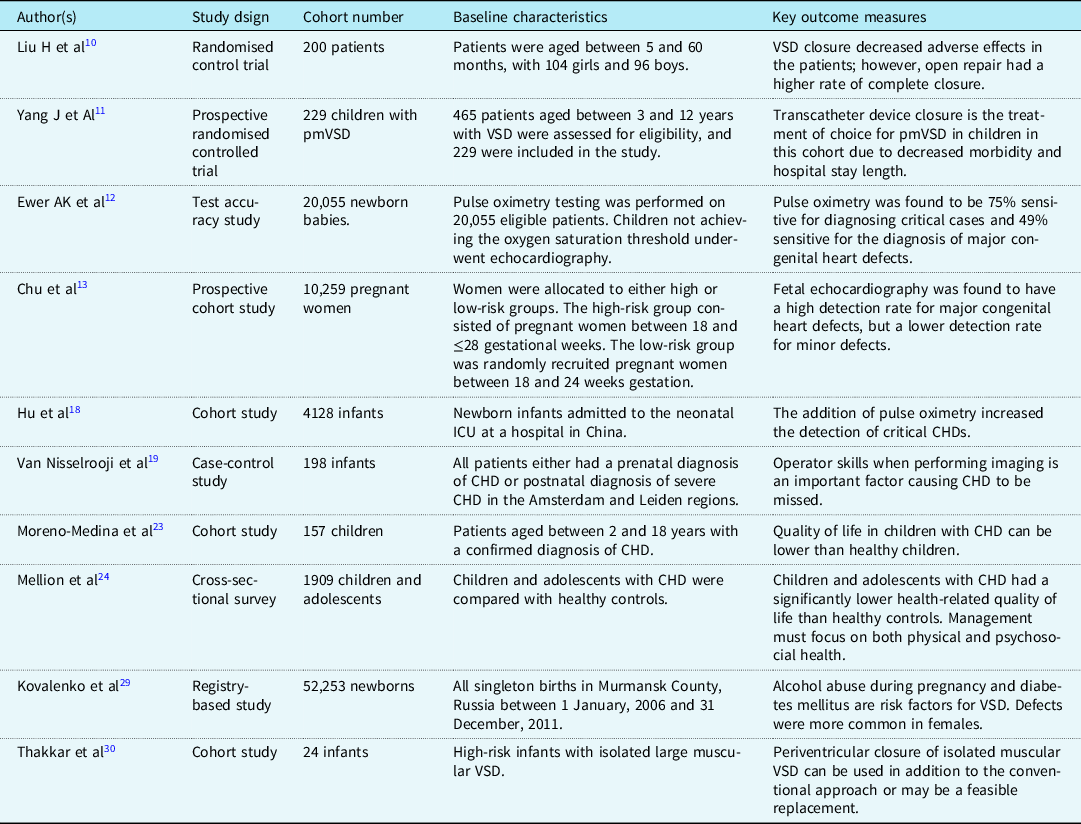
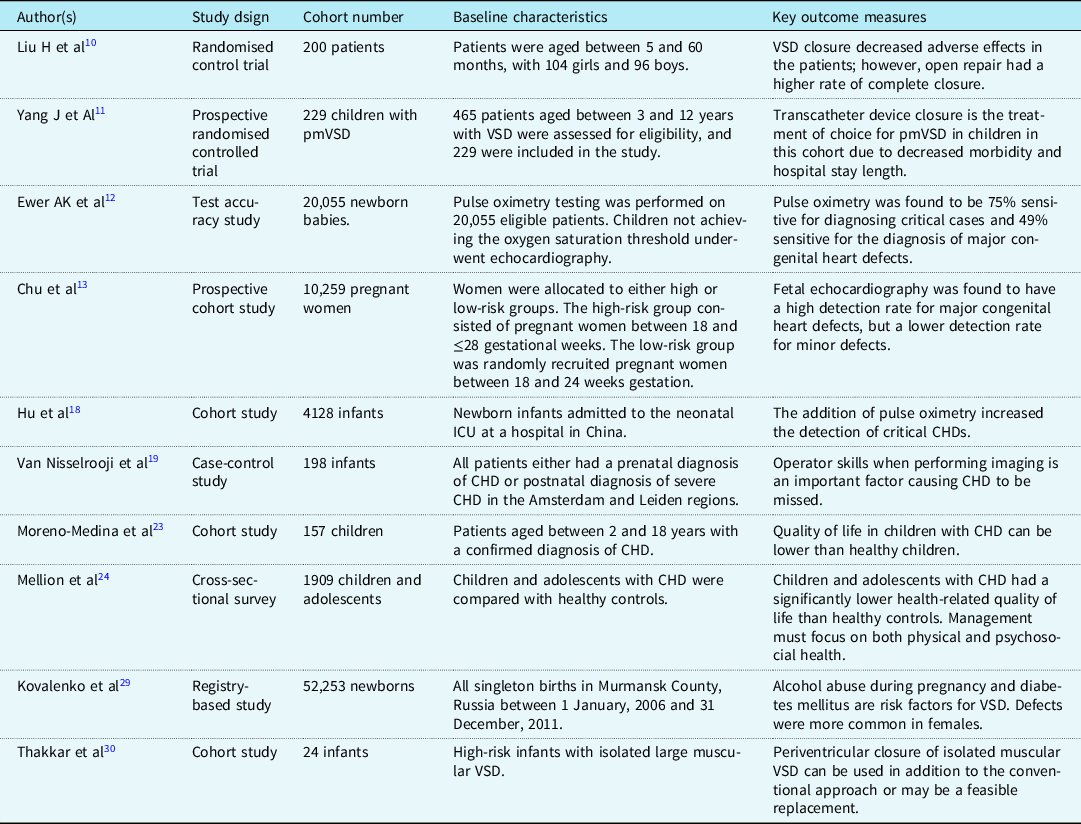
Searches were conducted without any date restrictions and identification of articles was guided by the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA). Reference Moher, Liberati, Tetzlaff, Altman and The9 The flowchart is illustrated in Fig 1. Of the initial 115 articles, 10 were eventually reviewed (Fig 1). The characteristics and outcomes of the selected studies are demonstrated in Table 1.
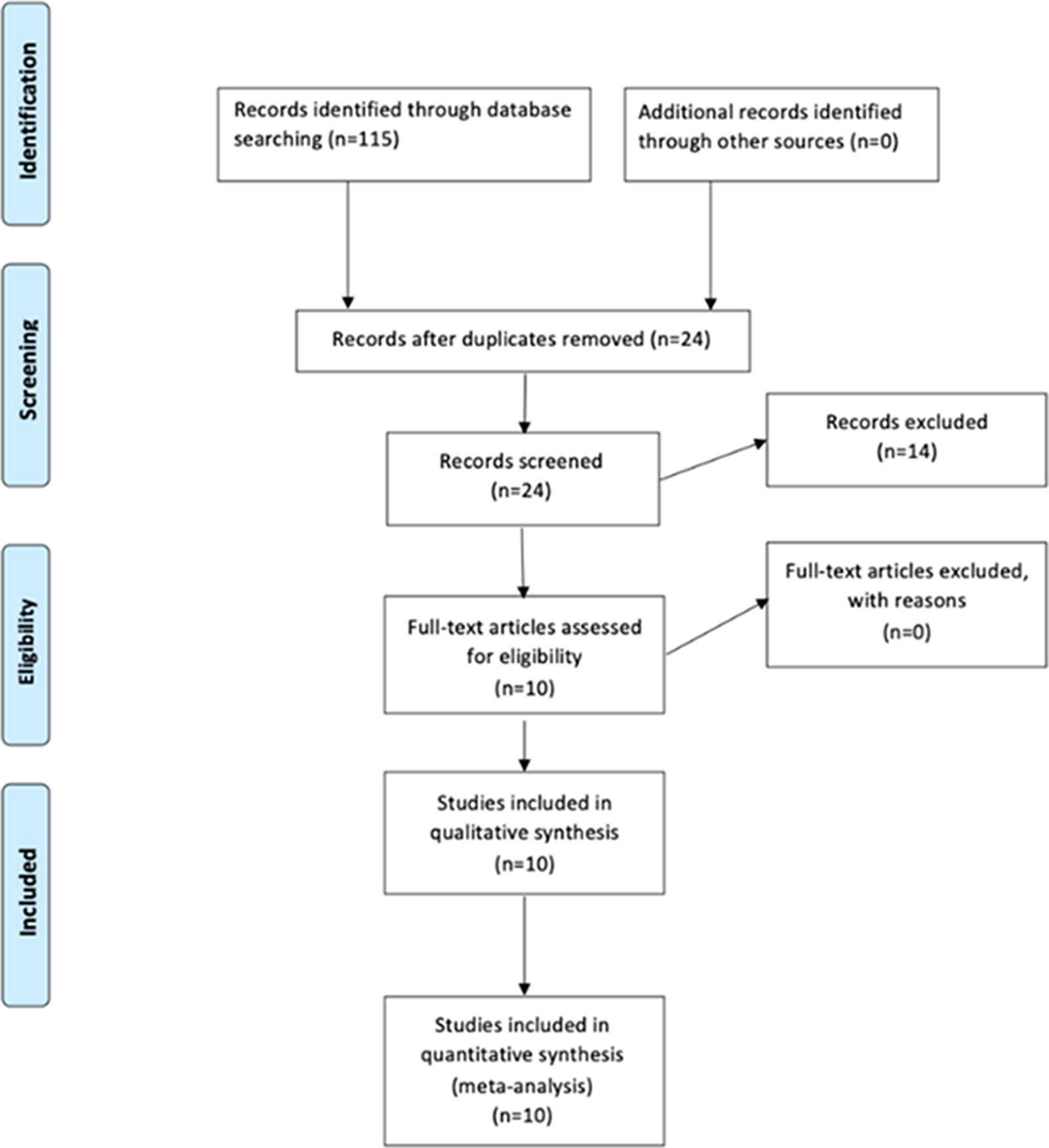
Figure 1. PRISMA chart of search results.
Table 1. Summary of study characteristics included in this review.
Critical Appraisal Skills Programme (CASP) 14–16 checklist for systematic review was employed to help analyse the studies selected. This particular programme was used as it allowed for a thorough, in-depth review of the literature.
Discussion
Risk factors for VSD
There are a variety of genetic and environmental factors predisposing to VSD. These are summarised in Table 2.
Table 2. Outline of the genetic and environmental factors attributing to VSD.

The majority of cases are attributed to multifactorial causes with Trisomy 21 being the commonest genetic association. VSDs commonly present with other septal defects, particularly ASDs in cases of genetic septal defects. Alcohol and illicit drug use is associated with septal malformation, thus, predisposing to VSDs. This may be explained by the effect of the teratogen on outflow tract formation and migration of neural crest cells resulting in a malformed cardiac septum. Sands et al Reference Sands, Casey, Craig, Dornan, Rogers and Mulholland17 conducted a study to assess the incidence of VSDs in “low-risk” neonates, and to identify risk factors. The study also found a gender association, with girls having a higher incidence of VSDs (p=0.004) than boys in a population of 173 “low risk” infants. Reference Sands, Casey, Craig, Dornan, Rogers and Mulholland17
Diagnosing VSD
Congenital heart defects are predominantly diagnosed in utero using foetal ultrasonography. However, there is a risk of clinically significant defects being missed on an initial investigation, which can have implications on the timing of treatment initiation. This is evidenced by Van Nisselroojj et al who found that many congenital heart defects are still missed in prenatal screening programmes. Reference Nisselrooij, Teunissen and Clur18 It was found that the major reason for this was the inadequate quality of the second-trimester standard anomaly scans used in the missed group. In 49% of the missed cases, inadequate imaging was the main cause which raised the lack of detection of congenital heart defects. Reference Nisselrooij, Teunissen and Clur18 This study concluded that congenital heart defects were being missed due to poor adaptation skills which caused poor quality SAS. Reference Nisselrooij, Teunissen and Clur18 Missed congenital heart defects can have grave implications on the infants’ health and delay the timing of treatment initiation. However, if left till late, missed congenital heart defects can result in severe morbidity or death.
A multicentre prospective cohort study was conducted in 2017 by Chu et al Reference Chu, Yan, Ren, Li and Gui13 which evaluated the effectiveness of foetal echocardiography in the prenatal diagnosis of congenital heart defects. Women in the first trimester of pregnancy were recruited for the study; those eligible were given detailed fetal echocardiography during the second trimester of pregnancy (18–28 weeks). A total of 10,259 pregnant women were included in the study, split into high and low-risk groups. The study found that fetal echocardiography was highly sensitive for detecting major congenital heart defects, but was less sensitive in diagnosing minor defects. When compared with muscular VSDs, perimembranous VSDs had greater sensitivities, but this was still markedly lower than major congenital heart defects such as Hypoplastic Left Heart Syndrome. Reference Chu, Yan, Ren, Li and Gui13 It was concluded that the utilisation of fetal echocardiography would be beneficial in the detection of major defects and would, therefore, aid parental counselling. Reference Chu, Yan, Ren, Li and Gui13 However, there was still a risk of delayed diagnoses due to the reduced sensitivity of echocardiography in detecting minor defects.
Early measurement of pulse oximetry can be utilised as an option to promote early detection of congenital heart defects including VSD. Reference Stockman19 The PulseOx study Reference Ewer, Middleton and Furmston12 was a prospective test accuracy study aiming to assess the accuracy of pulse oximetry as a screening tool for congenital heart defects such as VSD. The study analysed all asymptomatic babies born at six maternity units in the United Kingdom (20,055 babies in total), who were screened with pulse oximetry prior to discharge. Subsequently, infants not achieving predetermined oxygen saturations were given echocardiography after clinical examination. Reference Ewer, Middleton and Furmston12 The results of the study found that 50% of the babies with critical congenital heart defects had already been suspected at the antenatal screening, but 36% of those with major congenital heart defects (critical and serious) had been detected at screening. Six babies with critical congenital heart defects were falsely negative on pulse oximetry, and a further 21 babies with normal pulse oximetry findings had serious congenital heart defects such as VSD. The overall sensitivity of pulse oximetry was found to be 76% for critical cases, and 49% for serious cases. Reference Ewer, Middleton and Furmston12 The study, therefore, concluded that pulse oximetry was a “safe, feasible test” that aids in the screening process by helping to detect cases of critical CHD that aren’t detected by ultrasound. Reference Ewer, Middleton and Furmston12 These findings are further supported by another pulse oximetry study by Xiao-jing Hu et al who tested the use of pulse oximetry on 4128 newborn infants without a prenatal diagnosis of congenital heart defects. Reference Hu, Zhao and Ma20 Of these infants, 19 were found to have critical congenital heart defects. Reference Hu, Zhao and Ma20 However, if pulse oximetry was not used then there would have been seven missed cases of congenital heart defects. Reference Hu, Zhao and Ma20 Therefore, this study concluded that incorporating pulse oximetry into the screening process for congenital heart defects was vital in preventing delayed cases which would have been detrimental for those infants’ health.
Indications for repair of VSD
Indications for surgical intervention in VSD vary depending on the characteristics of the defect, such as the size and anatomical type. Small defects don’t require surgical closure as they usually undergo spontaneous closure. However, intervention may be required if the defect is moderately sized. Indications for closure in these cases include failure to thrive and poor development, significant enlargement of the left atrium or ventricle and/or elevated pulmonary arterial pressure, or a pulmonary–systemic flow ratio of greater than 2:1. Reference Rao21 Another indication for surgical repair is the development of significant aortic regurgitation due to prolapse of one of the aortic cusps. If congestive heart failure is present, it should be treated promptly. If the defect is large, a surgical closure is indicated in cases where systolic pressures in the right ventricle and pulmonary artery are close to left ventricular and aortic pressures. Reference Rao21
Open versus minimally invasive approaches to VSD closure
Traditionally, patients with VSD requiring treatment underwent open surgical intervention, however with advances in medical technology, there are now minimally invasive options available. Liu H et al conducted an open-label randomised controlled trial comparing the traditional open surgical approach to the new minimally invasive periventricular approach. Reference Liu, Lu and Zhou10 This study found that periventricular closure of ventricular septal defects was associated with a decreased rate of haemodynamic compromise, disorders of respiratory mechanics and cardiomyocyte viability, and tissue perfusion when compared with surgical closure. Reference Liu, Lu and Zhou10 However, it was also found that open surgical approaches were associated with a greater degree of complete defect closure than the periventricular technique. Continuous data were presented as means and standard deviations and compared by t-test by adhering to the normal Gaussian distribution. Reference Liu, Lu and Zhou10
In 2014, Yang J et al randomised 229 infants into two treatment arms, one receiving open surgical closure and the other undergoing a minimally invasive transcatheter approach. Reference Yang, Yang and Yu11 The infants were followed up for 2 years afterwards and a record was made of any major/minor adverse events, and laboratory testing was carried out measuring levels of CK-MB, ALT, BUN, and cTnI. Also, an echocardiogram was conducted 3 days after surgery to measure the degree of VSD closure. The results of the study found that neither the transcatheter or surgical procedures were associated with mortality or major adverse effects. However, there were 32 minor adverse effects in the surgical group and 7 in the transcatheter group (32.3% versus 6.9%). Fisher’s exact test was used to establish statistical significance, and there was a significant difference in minor adverse events found (p < 0.001). Reference Yang, Yang and Yu11 The study concluded that the transcatheter approach has a lower incidence of injury to the myocardium and is associated with a faster recovery and shorter hospital stay (Table 3).
Table 3. Comparative outcomes of studies reporting on minimally invasive versus open repair of ventricular septal defect (VSD).

VSD and other pathologies
VSD results in a shunt creation between the right and left ventricles. The degree of blood shunted and the direction of flow can determine the severity and haemodynamic significance. The pathophysiology of VSDs arises from a failure of development or fusion of the interventricular septum Reference Dakkak and Oliver22 . Membranous VSDs are the commonest subtype overall, whereas atrioventricular canal VSD (AVSD) are seen in Down syndrome. Muscular VSDs tend to occur in children due to the spontaneous closure with age. VSDs tend to occur in conjunction with other congenital heart defects. Most frequently, they are seen in tetralogy of Fallot, transposition of great arteries, and with pulmonary atresia.
TOF involves a VSD along with right ventricular hypertrophy, overriding aorta, and pulmonary stenosis. Pulmonary atresia with VSD can occur as a congenital defect due to an underdevelopment of the right ventricular outflow tract along with atresia of the pulmonary valve and trunk. Management of VSD varies with associated syndromes and other cardiac defects. For instance, definitive management of transposition of the great arteries involves an arterial switch (Jatene) procedure whilst VSD in pulmonary stenosis requires the Rastelli procedure Reference Rao23 . Multistep surgical correction is often required when VSD occurs in conjunction with other cardiac defects.
Prenatal screening
Early detection of congenital heart defects such as VSD is crucial in ensuring the best possible outcomes for patients, therefore it is important to have an effective prenatal screening process. In most countries, the screening process consists of a scan taking place at approximately 20 weeks gestation. Reference Sharland24 Both high and low-risk pregnancies are screened, and this is critical as risk factors are identified in only 10% of patients diagnosed with defects. Reference Allan25 Van Velsen et al Reference Ramaekers, Mannaerts and Jacquemyn26 conducted a geographical cohort study evaluating the effectiveness of a national screening programme in the Netherlands implemented in 2007, which consisted of a uniform national ultrasound anomaly scan for all pregnancies. The anomaly scan utilised a four-chambered view of the heart, with right and left outflow tract views. If congenital heart defects such as VSD are suspected on this scan, patients were referred to a tertiary centre for more detailed fetal echocardiography. After the screening programme implementation, the prenatal detection rate of VSD increased by 10.3% (from 28.7 to 39.0%), with >90% of diagnoses occurring before 24 weeks gestation. Reference Ramaekers, Mannaerts and Jacquemyn26 This demonstrates the beneficial effects of a uniform screening process for CHD in ensuring early diagnosis.
Quality of life of patients with VSD
Moreno-Medina et al conducted a study to assess the effects of congenital heart defects on the quality of life of children. In this study, 157 children with CHD underwent quality of life (QoL) assessment with 112/157 (71%) achieving 1-year follow-up. Reference Moreno-Medina, Barrera-Castañeda and Vargas-Acevedo27 The PedsQL 4.0 scale, which included generic and cardiac-specific modules was used for QoL evaluation. Reference Moreno-Medina, Barrera-Castañeda and Vargas-Acevedo27 Results from both modules showed that the children with CHD showed a better perception in the QoL evaluation compared to their caregivers who showed a less prominent perception of their children’s QoL. Overall, there was a lower score recorded for QoL in follow-up compared to baseline evaluation for both the children and their caregivers. Results showed that “emotional health” and “school functioning” were the most affected scores in the evaluation. In the cardiac-specific module, “cognitive status” showed the lowest scores in the evaluation both at baseline and follow-up. Reference Moreno-Medina, Barrera-Castañeda and Vargas-Acevedo27 Therefore, this shows that although children perceive their quality of life to be better than their caregivers, the overall quality of life of children with CHD was generally lower than that of a healthy child. This is also in line with a study carried out by Katelyn Mellion et al, which stated that children with CHD had a significantly lower score on QoL assessment compared to that of healthy controls. Reference Mellion, Uzark and Cassedy28 In this cross-sectional survey study, there were 1138 patients in the CHD group (625 children and 513 adolescents) and 771 patients in the healthy group (528 children and 243 adolescents). Patients with CHD scored lower on the evaluation in “total”, “physical health”, and “psychosocial health” compared to the controls (p < 0.0001). Reference Mellion, Uzark and Cassedy28 Therefore, this study showed the presence of worsened quality of life in children and adolescents with CHD and the need for intervention to improve the lower scores obtained.
Conclusion
Pulse oximetry and fetal echocardiography are established non-invasive diagnostic tools for VSD. The recent advances in minimally invasive treatment options including periventricular approach and transcatheter techniques have improved patient outcomes than traditional open repair of VSD, yet at the expense of higher residual rates. Careful patient selection for each technique and follow-up should be planned through multi-disciplinary team meetings.
Acknowledgements
None.
Funding
This research received no specific grant from any funding agency, commercial, or not-for-profit sectors.
Conflict of interest
None.
Ethical standards
None.