Over the last three decades, the Fontan operation has been modified to make more patients eligible.Reference Kaulitz and Hofbeck1 It has become the most common surgical procedure for treating congenital cardiac disease after the age of 2 years.Reference Gersony2 Two modifications (total cavopulmonary connections) include the extra-cardiac repair, using a baffle, excluding the right atrium, and the lateral tunnel, incorporating the right atrial wall as part of the tunnel connecting the inferior caval vein and the pulmonary artery.Reference Kaulitz and Hofbeck1 In both approaches, a fenestration is often created to relieve any subsequent rise in pressure in the venous system. The majority of survivors (83%) are free of transplantation for at least 15–20 years after surgery,Reference Khairy, Fernandes and Mayer3 thus more late complications are being observed.
We report the case of a 12-year-old girl with a rudimentary right ventricle, double inlet left ventricle, and transposition of the great arteries. After a lateral tunnel Fontan operation 8 years previously, she presented with increasing symptoms of being unwell on exercise owing to a combination of stenosis in the inferior caval venous pathway, and the presence of a fenestration and leak in the lateral tunnel. These were successfully treated with a single custom-made stent graft.
Materials and methods
A 12-year-old girl presented with a 1-year history of intermittent greyness, clamminess, and disorientation after exercise. Previously, an antenatal diagnosis of usual atrial arrangement, double inlet left ventricle, a large ventricular septal defect, a rudimentary right ventricle, and discordant ventriculo-arterial connections was confirmed at post-natal echocardiography. At 7 weeks of age, she underwent pulmonary artery banding and at 10 months a right-sided hemi-Fontan anastomosis. The conversion to lateral tunnel Fontan was performed at 3 years of age when a fenestration was also created. The oxygen saturation increased from 79% pre-operatively to 87% post-operatively.
Cardiac catheterisation and angiography at the age of 11 years showed a veno-venous collateral between the left subclavian and the left pulmonary veins. This was occluded with two Amplatzer vascular plugs of 6 and 4 millimetres (AGA Medical Inc., Plymouth, MN, United States of America). In addition, a stenosis was demonstrated in the mid portion of the lateral tunnel, measuring 11 millimetres × 13 millimetres with no pressure gradient. The tunnel was dilated below (31 millimetres) and above (40 millimetres) the stenosis. There was right-to-left shunting through the fenestration and a leak in the lateral tunnel.
At the multidisciplinary meeting, we agreed that this patient was better treated by an interventional approach rather than surgery. We felt a custom-made covered stent graft would be the best method to achieve closure of both the shunts and dilating the anastomotic stenosis. Such a stent graft (32 millimetres diameter and 55 millimetres long) was constructed (Fig 1) with full-thickness woven polyester sewn to the self-expanding Nitinol stent with braided polyester fabric and monofilament polypropylene suture (William Cook Europe ApS, Bjaeverskov, Denmark). This is a variant of the Zenith TX2 TAA low-profile endovascular graft, which is manufactured and widely available. To prevent migration of the stent graft, anchoring hooks were placed at the distal end of the stent. The stent was premounted within its own sheath, thus a long sheath was not required for its delivery. 18Fr sheath was required for passage through the femoral vein.

Figure 1 Picture of the custom-made stent graft used in our patient.
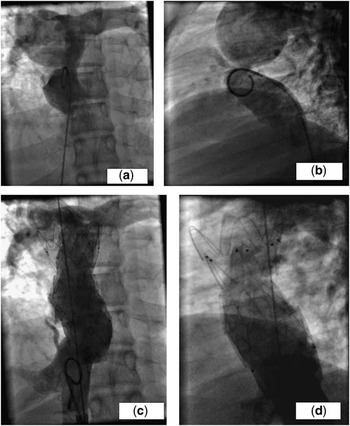
Through the left femoral vein, the lateral tunnel was crossed and a 0.035″ Lunderquist wire (William Cook Europe ApS, Bjaeverskov, Denmark) was positioned in the right subclavian vein. The self-expanding stent graft assembly was then advanced into the correct position with frequent angiograms. The covering sheath was withdrawn slowly so as to expose and deploy the graft. After deployment, there was a residual waste within the graft measuring 15 millimetres. In order to eliminate the waste, the graft was dilated serially with 18-, 20-, and 22-millimetre Cristal balloons (BALT Extrusion, Montmorency, France) to achieve a diameter of 20 millimetres (Fig 2a–d). There was excellent improvement in the degree of stenosis, with complete occlusion of the tunnel leak and fenestration. The regular aspirin maintenance medication was stopped 5 days before the procedure and warfarin was started after the procedure for 6 months.

Figure 2 (a) and (b) shows an anteroposterior and lateral projection of an angiogram showing stenosis within the tunnel. The leak and the fenestration are best shown in the lateral projection. (c) and (d) shows an anteroposterior and lateral projection of an angiogram showing the stent graft in place with relief of the stenosis and closure of the leaks and fenestration.
At follow-up 6 weeks later, the patient was well with improved effort tolerance. The oxygen saturation was 94%.
Discussion
Managing a lateral tunnel dehiscence with a balloon-expandable covered stent graft has been reported.Reference Hijazi, Ruiz, Patel, Cao and Dorros4, Reference Richens, Houston, Ruiz and Wilson5 A custom-made self-expandable stent has been used to close a fenestration and a lateral tunnel dehiscence.Reference Uberoi, Roberts, Barnes and Wilson6 However, in our patient, the symptoms were caused by a combination of stenosis within the lateral tunnel, right-to-left shunting from a leak within the tunnel, and through the fenestration, all of which were treated with a custom-made stent graft. The Zenith TX2 TAA endovascular graft does not have adequate radial strength to overcome the stenosis and therefore needed to be redilated with higher-pressure balloons. However, had there been a recoil of the stenosis, then a bare metal stent would have been implanted to provide extra radial strength.
Previously, a custom-made Cheatham-Platinum stent was used to close a leak in the Fontan circulation, but there was no additional stenosis.Reference Ewert, Schubert and Peters7 Cheatham-Platinum stents are fitted with reinforced welds to resist the mechanical forces associated with the stenosis.Reference Ewert, Schubert and Peters7 However, the diameters required in our patient precluded the use of such a stent. Furthermore, a self-expandable stent graft is more likely to adhere to the walls of the lateral tunnel and conform to its shape, improving the chances of covering the leak fully and reducing the risk of graft dislodgement and venous stasis.
The alternative methods of treating the tunnel stenosis, leak, and the fenestration include Amplatzer plugs and septal occluders,Reference Masura, Borodacova, Tittel, Berden and Podnar8 while treating the stenosis with conventional bare metal stents. However, the diameters of the tunnel precluded the use of the latter. Despite the use of Amplatzer occluders in a variety of clinical situations, they may be effective only in small leaks,Reference Ewert, Schubert and Peters7 and multiple occluders would need to be used to close both the fenestration and the lateral tunnel leak.
It is arguable whether the stenosis needed to be dilated, since there was no pressure gradient detected in the anastomosis. However, in the Fontan low flow circulation, gradients are not easy to detect. Furthermore, a morphological narrowing without a pressure gradient may still resist passive venous flow.Reference Ovroutski, Ewert, Alexi-Meskishvili, Peters, Hetzer and Berger9 Therefore, in order to optimise the flow through the tunnel, the stenosis was dilated.
The presence of the fenestration and lateral tunnel leaks resulted in lowering of the oxygen saturation and decreased exercise tolerance. By dealing with these, the oxygen saturation increased from 89% pre-operatively to 94% post-operatively with an improvement in the symptoms.
Conclusion
Following a Fontan operation, maintaining an optimum quality of life often requires repeat percutaneous interventions to deal with different haemodynamic problems. In our patient, we have shown that tunnel stenosis, closure of fenestration, and lateral tunnel leak can be addressed with a single, custom-made stent graft.
Acknowledgements
We wish to acknowledge Professor Shakeel Qureshi and Dr John Reidy for their role in the management of this patient.