Management of aortopulmonary window with interrupted aortic arch is complex, particularly if the patient presents beyond infancy.Reference Sharma, Ameta and Shukla1–Reference Daily, Sissman, Lipton and Shumway5 This predisposes to early pulmonary vascular disease. Surgical repair is challenging owing to the difficulty in mobilisation of the aortic arch and descending thoracic aorta.Reference Sharma, Ameta and Shukla1–Reference Daily, Sissman, Lipton and Shumway5
Case report
A 6-year-old girl presented with exertional dyspnea and palpitation for 2 years. On examination, pulses were equally palpable with no pressure gradients in all limbs. Oxygen saturation was 94% without differential cyanosis. A grade 2/6 systolic murmur and loud pulmonary component of second heart sound were audible at pulmonary area. Chest X-ray revealed cardiothoracic ratio 0.75, dilated pulmonary arteries, and increased pulmonary vascular markings (Fig 1A). Left atrial and left ventricular enlargement was evident on electrocardiogram. Transthoracic echocardiography demonstrated large aortopulmonary window with low velocity left-to-right flow, suggesting severe pulmonary arterial hypertension. Left atrium and left ventricle were dilated with normal biventricular systolic function.
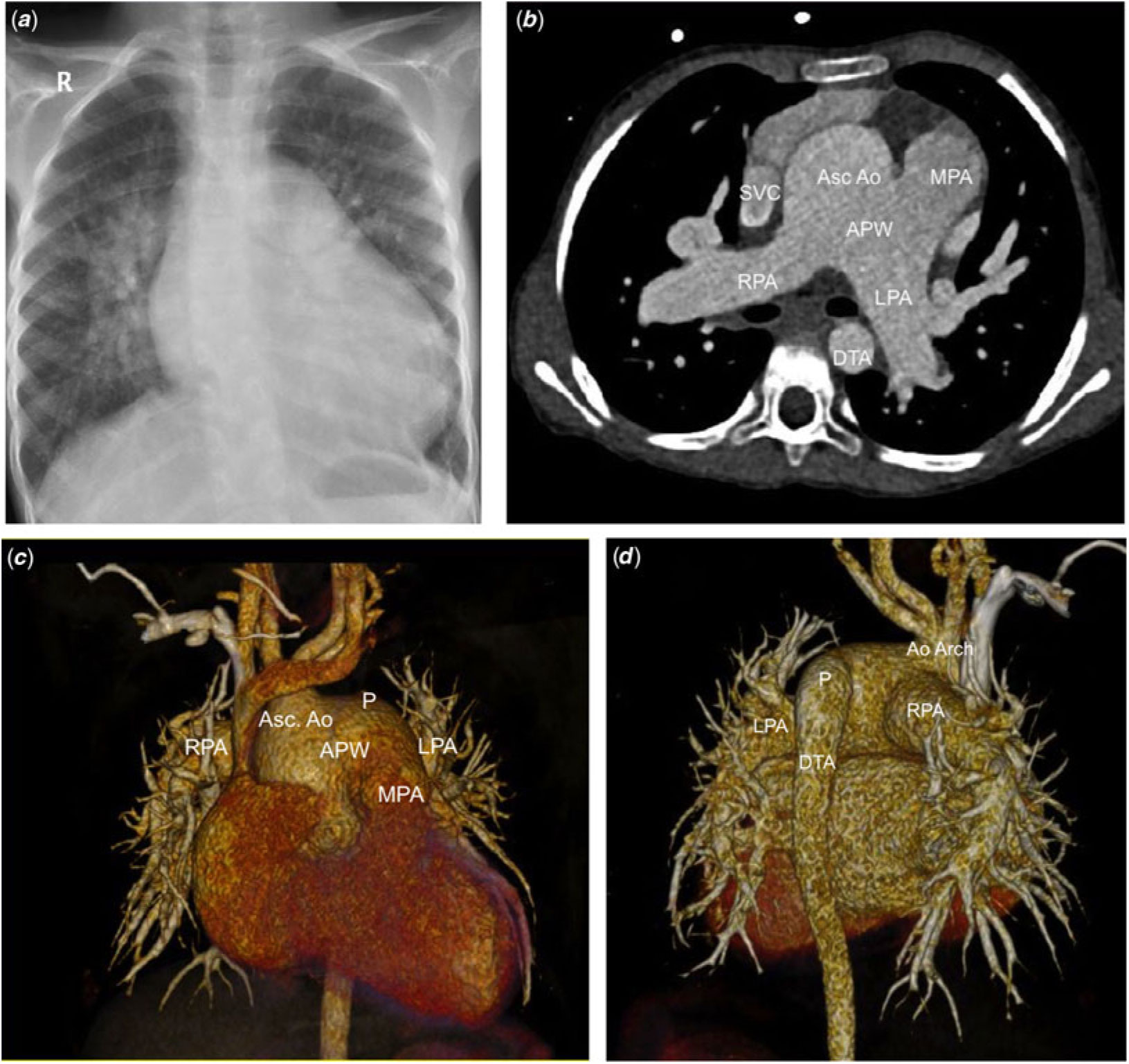
Figure 1. (a and b) Pre-operative images. (a) Chest X-ray showing cardiomegaly; (b) computed tomographic (CT) angiography, axial view at the level of aortopulmonary window (APW). (c and d) Reconstructed CT angiography images. (c) Anterior view showing APW. (d) Posterior view showing absent isthmus and continuity of patent arterial duct with descending thoracic aorta (DTA).
CT angiography (Fig 1B–D) confirmed the findings. The aortopulmonary window extended up to the aortic arch. The right pulmonary artery was separate from the main pulmonary artery and was arising from the posterior ascending aorta (Fig 1B). Aortic arch was interrupted beyond the left subclavian artery (Type A interrupted aortic arch) with a patent arterial duct continuing as the descending thoracic aorta. Cardiac catheterisation (Table 1) revealed equal pressures in aorta and pulmonary artery, pulmonary to systemic flow ratio of 3.3 and pulmonary vascular resistance index 9.6 Wood Units.m2 on room air. The pulmonary vascular resistance index fell to 2.8 Wood Units.m2 following oxygen supplementation. In view of high pulmonary blood flow and oxygen-responsive pulmonary vascular resistance index, she was considered operable.
Table 1. Cardiac catheterisation data

* SaO2 (PaO2).
After sternotomy, bilateral pulmonary arteries and patent arterial duct were dissected. Aorta was right and posterior to the dilated pulmonary artery. There was a large distal aortopulmonary window, and the right pulmonary artery was arising from the right side of the ascending aorta at a higher level compared to left pulmonary artery, which was present at the same level and on the left side of aortopulmonary window. The aorta was interrupted beyond the left subclavian artery with patent arterial duct continuing as descending thoracic aorta (Fig 1).
A 6-mm-wide polytetrafluoroethylene graft was sutured to the right innominate artery for arterial inflow. Cardiopulmonary bypass was instituted after cannulating the superior and inferior vena cavae. Both pulmonary arteries were snugged to prevent run-off into the lungs. After cooling to 18 °C, aorta was cross-clamped, and a single dose of del Nido cardioplegia was administered into the aortic root. Since the arterial cannula was inserted via graft on right innominate artery and not on the aorta, it allowed sufficient space for aortic cross-clamping distal to the snugged right pulmonary artery. Total circulatory arrest was performed with removal of the aortic cross-clamp to facilitate exposure. Aortopulmonary window was divided and orifices of both pulmonary arteries were identified. The patent arterial duct was divided at its junction with descending thoracic aorta and its pulmonary end was suture closed. The right pulmonary artery was detached from the ascending aorta leaving a cuff of aortic tissue with it. Even after maximal mobilisation of the descending thoracic aorta, a wide gap precluded a tension-free anastomosis between the proximal ascending and descending thoracic aorta with possibility of tracheobronchial compression by an excessively mobilised descending thoracic aorta. Therefore, a 16-mm-wide ringed polytetrafluoroethylene graft was sutured with a continuous 5-0 polypropylene suture to the descending thoracic aorta. The proximal quarter of the aortic side of aortopulmonary window was closed by direct running 5-0 polypropylene suture. The rest of the orifice of the aortopulmonary window formed the proximal anastomotic line between the graft and the ascending aorta. An oval-shaped polytetrafluoroethylene patch was used to cover the deficiency caused by the harvest of right pulmonary artery on the right side of ascending aorta. Once aorta was reconstructed, the circulation was re-established, with gradual rewarming. Right pulmonary artery was fully mobilised, was passed behind the reconstructed aorta, and anastomosed end-to-side to the defect in the main pulmonary artery that resulted from the division of the aortopulmonary window (Fig 2). The patient was uneventfully weaned off cardiopulmonary bypass on elective inotropic support of dobutamine (5 µg/kg/minute) and noradrenaline (0.05 µ/kg/minute). Cardiopulmonary bypass time was 152 minutes and the total circulatory arrest time was 49 minutes. Post-operative recovery was uneventful. Sildenafil and bosentan were continued, and she was discharged on the 17th post-operative day. Post-operative echocardiography showed adequate surgical repair, normal right ventricular function; right ventricular systolic pressure predicted by tricuspid regurgitation jet was 30 mmHg. Check CT angiogram (Fig 3) revealed normal flow in aortic arch, descending thoracic aorta and pulmonary arteries.

Figure 2. (a and b) Intraoperative images. (a) Pre-repair anatomy of APW and interrupted aortic arch (IAA). The cross-clamp has been placed on the ascending aorta and the right innominate artery has been connected to the arterial circuit of CPB via 6-mm-wide polytetrafluoroethylene graft. Absence of aortic isthmus can be appreciated. (b) Post-repair image showing reconstruction of aortic arch with 16-mm-wide polytetrafluoroethylene ringed graft. (c and d) Line diagram. (c) Pre-operative anatomy. The right pulmonary artery is arising at a higher level from the aorta after the defect. (d) Post-operative anatomy; 1- polytetrafluoroethylene patch used to cover the harvest site of right PA from ascending aorta, 2- direct suture closure of quarter of aortic side of APW, 3- anastomotic line between right PA and main PA at the orifice of pulmonary side of APW, 4- suture closed pulmonary end of patent ductus arteriosus, 5- proximal anastomotic line of no-16 polytetrafluoroethylene graft with ascending aorta at the aortic side of APW, 6- distal anastomotic suture line between interposition graft and DTA.

Figure 3. (a and b) Post-operative CT angiography images. (a) Right PA has been implanted to main pulmonary artery and confluent patent good-sized bilateral PA can be appreciated. (b) Continuity of aortic arch with DTA has been established with 16-mm-wide polytetrafluoroethylene ringed graft. Blood flow through wide patent graft and lack of compression of nearby airways can be appreciated. (c and d) Reconstructed CT angiography images. (c) Anterior view showing repaired APW and IAA. (d) Right-sided view showing reconstructed arch with 16-mm-wide polytetrafluoroethylene ringed graft.
Discussion
Aortopulmonary window with interrupted aortic arch is uncommon.Reference Sharma, Ameta and Shukla1–Reference Daily, Sissman, Lipton and Shumway5 The hypoplasia of aorta is thought to result from diversion of a larger proportion of blood to right pulmonary artery during foetal life.Reference Berry, Bharati and Muster6 Type A interrupted aortic arch is the most common type seen in association with distal aortopulmonary window.Reference Berry, Bharati and Muster6, Reference Konstantinov, Karamlou and Williams7 Echocardiography and CT angiography are diagnostic.Reference Joshi, Gujare, Merchant and Sankhe2
Only eight cases have been published about this combination beyond infancy.Reference Sharma, Ameta and Shukla1–Reference Daily, Sissman, Lipton and Shumway5 Only three of these underwent corrective surgery and one underwent a pulmonary artery band. One patient, who was repaired, died after 2 years and was lost to follow-up.
A patent arterial duct is important to maintain continuity of systemic perfusion in this anomaly. Oppenheimer et al.Reference Oppenheimer-Dekker, Gittenberger-de Groot and Roozendaal8 have found that in these patients, the duct varies from one with normal to abnormal intimal cushions and recommend surgical repair with excision of all ductal tissue.Reference Oppenheimer-Dekker, Gittenberger-de Groot and Roozendaal8
Direct anastomosis of aortic arch to descending thoracic aorta or a left subclavian plasty is preferred since it preserves growth potential.Reference Murin, Sinzobahamvya and Blaschczok9, Reference Gargiulo, Zannini and Albanese10 Some advocate single autologous pericardial patch technique even in neonates and infants to avoid complications of stenosis of aortic arch, pulmonary artery branches, and tracheobronchial compression.Reference Roubertie, Kalfa, Vergnat, Ly, Lambert and Belli11 Anterior translocation of the right pulmonary artery is recommended in patients with bronchial compression.Reference Chang, Sung, Kim and Lee12
We decided to use an interposition graft between the ascending aorta and the descending aorta because a direct anastomosis without tension was improbable and there was a distinct possibility of resultant airway compression.Reference Roubertie, Kalfa, Vergnat, Ly, Lambert and Belli11 Moreover, 16-mm-wide graft was considered large enough to accommodate the increased demand of blood flow even when she reaches adulthood. The cuff of aorta taken along with right pulmonary artery helped in decreasing the distance between the right pulmonary artery and the pulmonary orifice of the aortopulmonary window, resulting in a tension-free anastomosis.
In older patients, pulmonary arterial hypertension may persist.Reference Sharma, Ameta and Shukla1–Reference Daily, Sissman, Lipton and Shumway5 Daily et al.Reference Daily, Sissman, Lipton and Shumway5 reported staged closure of aortopulmonary window with interrupted aortic arch in a 15-year-old boy who died 2 years following repair. Dong et al.Reference Dong, Yinglong and Junwu4 reported a 13-year-old child in their case series of five patients of aortopulmonary window with interrupted aortic arch without details. However, one of their patients died post-operatively due to pulmonary hypertensive crisis and another had recurrence of symptomatic pulmonary hypertension 22 months after surgery.Reference Dong, Yinglong and Junwu4 Near-normal pulmonary artery pressure and normal right ventricular function in immediate post-operative period in our patient are assuring, but need more follow-up.Reference Neutze, Ishikawa, Clarkson, Calder, Barratt-Boyes and Kerr13
Conclusions
Aortopulmonary window with interrupted aortic arch presenting after infancy is rare. A careful stepwise haemodynamic assessment is needed to decide operability. Older age of presentation mandates technical modification and long-term follow-up for possible residual or recurrent pulmonary arterial hypertension.
Acknowledgement
None.
Financial Support
This research received no specific grant from any funding agency, commercial or not-for-profit sectors.
Conflicts of Interest
None.
Ethical Standards
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant Indian national guidelines on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008, and have been approved by the All India Institutional Institute of Medical Sciences, New Delhi, India institutional committee.






