Aortopulmonary window is a rare congenital cardiac anomaly occurring due to incomplete separation of conotruncus by the aorticopulmonary septum with separate semilunar valves. The usual presentation is in early infancy and childhood due to congestive heart failure.Reference Backer1 Early surgical closure is required before progression to irreversible pulmonary hypertension beyond infancy, which contradicts closure. Recently, attempts have been made for transcatheter device closure of this anomaly, but it is not possible in all cases, particularly for large proximal and distal types. Surgical closure is feasible for all types with excellent long-term outcomes.Reference Aggarwal, Mishra and Sai2 Here, we present the case of a 14-year-old boy, with a large type I aortopulmonary window who developed severe pulmonary artery hypertension causing the dilated pulmonary artery to cause compression of the left main coronary artery. He underwent a successful anterior sandwich repair after a failed attempt at device closure.
Case summary
A 14-year-old boy was presented to the cardiologist with complaints of dyspnoea and angina on exertion and palpitations for the past 1 year. Clinically, there was no cyanosis. His resting ECG was essentially normal with no ST-T changes. On echocardiography, there was an enlarged left atrium, left ventricle, and main pulmonary artery with severe pulmonary artery hypertension. There was a large type I aortopulmonary window of 24 mm. CT angiography (Fig 1b) was done that confirmed the above findings. On the catheterisation study (Fig 1a), pulmonary artery pressures were at systemic levels, which reduced transiently after partial device occlusion. Main pulmonary artery was dilated (3.5 cm) and was seen compressing the left main coronary artery. The closure was attempted with a 24 mm ventricular septal defect device and 28 mm atrial septal defect device (Amplatzer, Abbott), but was unsuccessful despite multiple attempts. Also, there were transient ST-T changes while deploying the device, hence the procedure was abandoned and was referred for surgical closure of aortopulmonary window. Under normothermic cardiopulmonary bypass, aortic root cardioplegia was given after snaring both pulmonary arteries with a left ventricular vent in situ. A trans-window vertical incision was used for opening the defect (Fig 2a). The right pulmonary artery (Fig 2b) and coronary ostia (Fig 2c) were away from the defect. Polytetrafluoroethylene patch was used to close the window with the anterior sandwich technique. The left main coronary artery was seen arising eccentrically to the left and a little higher than usual, but the caliber was found to be adequate on putting a Garrett probe (®Scanlan Memory Garrett). Post cardiopulmonary bypass, PA was found to be soft, less distensible and PA pressures were 50% of the systemic pressures. The post-operative course was uneventful and the patient was discharged on day 5. The patient is doing well in the follow-up clinic. We have attached the post-operative echocardiography images (Fig 3). At 6 months follow-up, the patient is doing well. He is NYHA class I and maintaining a saturation of 98% on room air. ECG shows sinus rhythm with echocardiography showing no residual flow across the aortopulmonary window patch. Right ventricular systolic pressure measured by the TR jet was 30 mmHg.

Figure 1. ( a ) Cardiac catheterisation showing the aortopulmonary window with the compression of the left main coronary artery by dilated main pulmonary artery (marked by an asterisk) and ( b ) CT angiography showing the same.

Figure 2. Intraoperative pictures. ( a ) Intraoperative anatomy of the heart showing the aortopulmonary window and the dilated main pulmonary artery. ( b ) On opening the aortopulmonary window with a probe in right pulmonary artery. ( c ) On opening the aortopulmonary window with a probe in left main coronary artery.
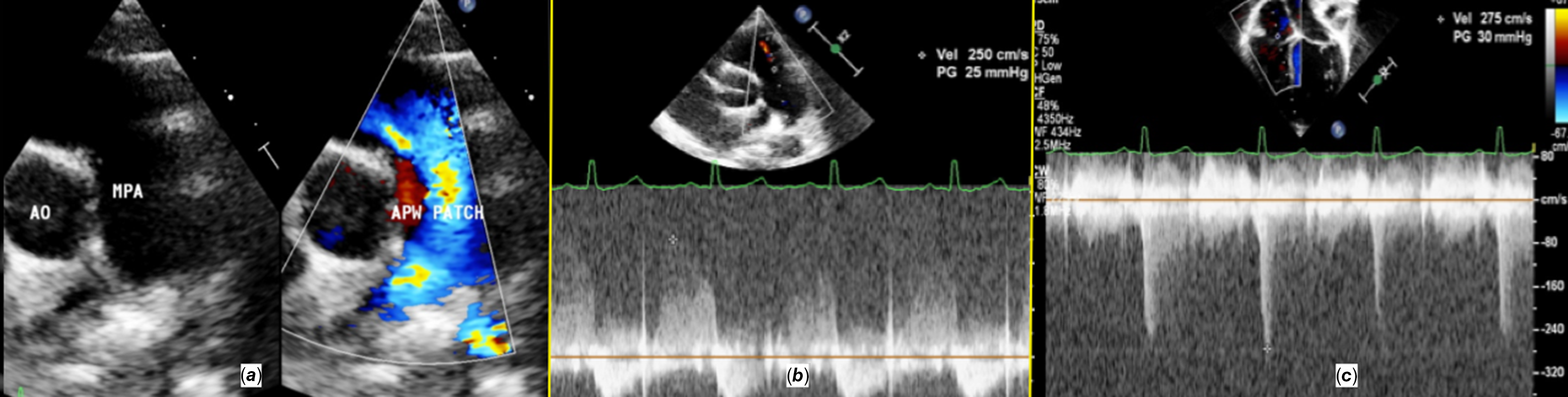
Figure 3. ( a ) Parasternal short-axis view showing patch across aortopulmonary window with no residual shunt. ( b ) Parasternal short-axis view showing trivial pulmonary regurgitation with a peak of 25 suggesting normal PA pressure. ( c ) Apical four-chamber view showing mild tricuspid regurgitation jet with RV systolic pressures of 30 mmHg.
Discussion
Aortopulmonary window may occur as an isolated lesion, or it can be associated with other cardiac abnormalities in one-third to one half of the cases.Reference Backer1 Echocardiography usually establishes diagnosis in most cases. Assessment of operability can be determined by the clinical status, absence of cyanosis, cardiomegaly on chest X-rays, features of left ventricular volume overload on electrocardiogram, and cardiac catheterisation findings.Reference Aggarwal, Mishra and Sai2
Still, presentation beyond infancy is not so uncommon in developing countries due to poor socio-economic conditions.Reference Kothari3 In the presence of severe pulmonary artery hypertension, if significant reversibility in the pulmonary vascular resistance index could be demonstrated with oxygen, the condition can be successfully corrected with good long-term outcomes. Severe pulmonary artery dilatation has been described as a predisposing risk factor for left main coronary artery compression in patients with pulmonary artery hypertension.Reference Mesquita, Castro, Ikari, Oliveira and Lopes4 The pulmonary artery diameter is the most important aspect of the left main coronary artery stenosis in these cases, but other aspects like mean pulmonary artery pressure or angina symptoms are not significantly associated with coronary compression.Reference Mesquita, Castro, Ikari, Oliveira and Lopes4
It is important to confirm myocardial ischaemia due to left main coronary artery compression before indicating a treatment.Reference Pina, Exaire and Sandoval5 There are patients in whom the haemodynamics can be stabilised only by treating the cause of pulmonary hypertension. Although percutaneous coronary intervention and rarely coronary artery bypass grafting may be an option, but as in our case, just treating the cause of the massive pulmonary artery dilatation could help resolve the compression of left main coronary artery.
Device closure of aortopulmonary window in adolescents is rarely reported because of the rarity of the defects with good margins, associated congenital cardiac anomalies requiring cardiac surgery, early development of Wiesenberger syndrome in this population, or due to technical challenges precludes device closure.Reference Trehan, Nigam and Tyagi6 We approached this case through the window for surgical closure. It provides excellent exposure of the defect along with a clear view of ostia of left coronary artery, right coronary artery, and right pulmonary artery. It isn’t associated with semilunar valves distortion and post-surgical great arteries stenosis.
Conclusion
Though a rare congenital cardiac anomaly, presentation of the aortopulmonary window in the adolescent age group is observed amongst developing countries. Irreversible pulmonary artery hypertension precludes closure of the defect. Device closure is restricted for intermediate types with adequate superior and inferior rims. Surgical closure can be safely achieved for reversible pulmonary hypertension cases with excellent long-term outcomes.
Acknowledgements
None.
Financial support
This research received no specific grant from any funding agency, commercial, or not-for-profit sectors.
Conflicts of interest
None.
Ethical standards
The manuscript was approved by the departmental ethical committee. Informed consent was taken from the patient and his parents for publication purposes.






