Published online by Cambridge University Press: 16 September 2005
Aim: To identify patients with visceral heterotaxy who are at risk from fulminant sepsis. Methods: We studied 38 patients, 37 having undergone abdominal ultrasound, all 38 having examination of blood films to establish presence of Howell-Jolly bodies, and all 38 documented to have had pneumococcal vaccination and prophylaxis with penicillin. We checked whether the parents were aware of the splenic state of their child, and when possible, we compared current results of blood films with those obtained postnatally. Results: Two of the 17 patients with multiple spleens, all 11 without a detectable spleen, and 1 of 9 patients with a normal spleen, showed Howell-Jolly bodies in their blood films. In 5 of 23 patients with serial blood films, Howell-Jolly bodies had not been seen postnatally, but could now be detected in current blood films. Of these patients, 2 had multiple spleens, 1 did not have a spleen, and 1 had a solitary spleen of normal size. In the other patient, ultrasound could not be performed. Only one of these patients was receiving penicillin prophylactically, and had received pneumococcal vaccination. Of the 15 patients in whom Howell-Jolly bodies were present in the blood, only 8 parents knew about the potential risk for infection. Another 7 parents were sure that their child was taking penicillin regularly, and had received pneumococcal vaccination. Conclusions: Howell-Jolly bodies can be found in the blood of patients with visceral heterotaxy independent of the anatomical state of the spleen. As Howell-Jolly bodies can be encountered in the blood of such patients with increasing age, those with multiple and solitary spleens should be monitored regularly to identify those at risk. Parental knowledge of the splenic state, and compliance for prophylaxis using penicillin, and pneumococcal vaccination, were unsatisfactory in our cohort.
Visceral heterotaxy is characterised by symmetry of the lungs, the bronchial tree, and atrial appendages, all of which typically show left or right morphology bilaterally.1 The association of congenital absence of the spleen with isomerism of the right atrial appendages is well recognised, as is the presence of multiple spleens in the setting of isomerism of the left atrial appendages, together with abnormal arrangement of the other abdominal organs. Exceptions to these rules, nonetheless, are equally well recognsied.2
Mortality due to the complex cardiac malformations encountered in these patients is high, despite innovations in cardiac surgery.3–5 Functional or anatomical asplenia in some, with its resultant susceptibility to fulminant sepsis, especially due to pneumococcal infections, contributes to this high mortality.6, 7 Thus, it is mandatory to identify patients at high risk for infections. It remains unclear, nonetheless, how best to make a reliable diagnosis of functional asplenia.
In this prospective study, we have compared the splenic state evaluated by abdominal ultrasound with results of testing for Howell-Jolly bodies in the blood of our cohort of patients with visceral heterotaxy. We have also investigated the adherence to penicillin prophylaxis, pneumococcal vaccination, and the knowledge of the parents about the possible consequences of functional asplenia in their children.
We discovered 74 patients with the diagnosis of visceral heterotaxy who had undergone cardiac surgery at Birmingham Children's Hospital between 1985 and 2001. Data, including the cardiac diagnosis and surgical repairs, was extracted from our cardiac database, case notes, reports of echocardiography and catheterisation, and the operative notes. The diagnosis of either left or right isomerism of the atrial appendages was suspected after echocardiographic or angiographic evidence of either a juxtaposed abdominal aorta and inferior caval vein for isomerism of the right atrial appendages, or continuation of the inferior caval vein through the azygos venous system for isomerism of the left atrial appendages, together with attempts made pre-operatively to determine the morphology of the atrial appendages.8 The diagnosis was confirmed at the time of surgery, when the atrial appendages in all patients were found to be of either left or right morphology on both sides.
At the time of this study, 51 of the patients were alive. We made contact with these 51 survivors and their families, who were invited to be part of a prospective study into splenic state and function. Of the 38 who volunteered to be part of the study, 23 had isomerism of the left atrial appendages, with a mean age of 6.8 years, and a range from 1.7 to 15.1 years, and 15 had isomerism of the right atrial appendages with a mean age of 7.5 years, and a range from 3.2 to 15.9 years. We were able to undertake abdominal ultrasound in 37 of the patients, while in all the patients we made blood films to look for Howell-Jolly bodies, documented the general state of vaccination, including pneumococcal polysaccharide vaccination with Pneumovax®, assessed the practice of penicillin prophylaxis, and established the parental knowledge of the splenic state of their child, and its implications for the potential risk of infection. In 23 patients, we were able to compare blood films made previously with those currently available. Of our cohort of 38 patients, 18 had undergone their first operation within the neonatal period, and 24 within the first 3 months of life. Biventricular circulations had been established in 16 patients, with 22 undergoing functionally univentricular palliation.
Abdominal ultrasound was performed to diagnose the splenic state, using a Phillips ATL HDI 5000 machine (Bothell, Washington, USA). The examinations were done using curvilinear transducers of 4 to 7 megahertz, with the patients lying supine. The studies were carried out by experienced paediatric radiologists (HW, LS) who were unaware of the cardiac diagnoses, or the results of the blood films. In each case the presence or absence and the number of spleens were documented, along with the site when splenic tissue was identified. If there was a solitary spleen, its longest diameter was measured on a coronal image obtained through the splenic hilum.9 Multiple spleens were defined as ultrasonic detection of 2 or more spleens.
Howell-Jolly bodies were counted in blood films stained by the Giemsa/May-Grünwald method. The results were expressed as the number of Howell-Jolly bodies per 10,000 peripheral red cells. Detection of more than 1 Howell-Jolly body was considered a positive result. The films were examined by a technician experienced in haematology, who had no clinical information regarding the patients from whom the samples had been obtained.
Other possible causes of anatomical or functional hypoplasia or absence of the spleen could be excluded in all cases. None of the patients had undergone a splenectomy, or was suffering from coeliac or haematologic disease at the time of the study.
The record for vaccination was established by checking the health documents of the child. Parents were asked about the practice of penicillin prophylaxis, pneumococcal vaccination, and their knowledge of the splenic state of their child, and its implications for the potential risk for fatal infections in case of asplenia according to a prepared questionnaire.
The study was approved by the local research ethics committee, and informed consent to participate in the study was obtained from all parents.
We found multiple spleens in 16 of 22 patients (73 percent) known to have isomerism of the left atrial appendages, and in 1 of 15 patients (7 percent) with isomerism of the right atrial appendages (Fig. 1). It was not possible to detect a spleen in 11 (73 percent) of our patients with isomerism of the right atrial appendages. A solitary and normally sized spleen was found in 6 patients (27 percent) with isomerism of the left atrial appendages, and in 3 (20 percent) with isomerism of the right atrial appendages. We were unable to perform an ultrasonic investigation in 1 of our patients with isomerism of the left atrial appendages because of lack of cooperation. In this patient, however, we did discover Howell-Jolly bodies in the blood. In all, we found Howell-Jolly bodies in the blood of all the patients without a visible spleen, in 2 of 17 patients (12 percent) with multiple spleens, and in 1 of 9 patients (11 percent) with a solitary spleen of appropriate size for age (Fig. 2).
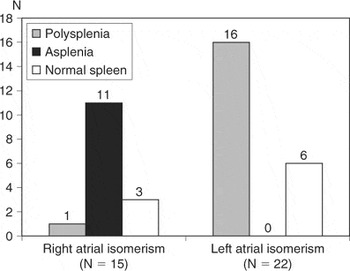
Figure 1. Abdominal ultrasonic findings in 37 patients with visceral heterotaxy. It proved impossible to perform an ultrasonic investigation in 1 patient with isomerism of the left atrial appendages.

Figure 2. Comparison of the anatomical state of the spleen as diagnosed by abdominal ultrasound with the results of testing for Howell-Jolly bodies in the peripheral blood.
In 23 of the patients, we were able to compare the current blood films with those performed postnatally within the first month of life. The findings proved incongruent in 8 of the patients (35 percent – Table 1). In 5 patients, aged now a mean of 3.4 years, with a range from 1.7 to 4.4 years, Howell-Jolly bodies had not been detected postnatally, but were now found in current blood films. Only one of these patients, who was asplenic, was receiving penicillin prophylaxis and had evidence of pneumococcal vaccination. A further patient, with multiple spleens, was on penicillin prophylaxis only. The other 3 patients who now had Howell-Jolly bodies in their blood were unprotected. In 3 patients, with a mean age of 8.4 years, and a range from 6.7 to 10.4 years, initially positive postnatal results had changed into current negative blood films. Of these patients, one was on penicillin prophylaxis only, and one was taking penicillin and had received pneumococcal vaccination.
Table 1. Changes in current blood films compared to first postnatal blood films in 8 out of 23 patients.

Of the 15 patients now shown to have Howell-Jolly bodies in their blood films, only 8 parents (53 percent) knew about the potential risk for infection in their children, and the measures they should take in case of fever. Of these 8 sets of parents, 7 were sure that their child was taking penicillin regularly and had received pneumococcal vaccination. One child, however, was neither on penicillin, nor had received the vaccination. The remaining 7 sets of parents were not sure if there was a risk for infection. Of these children, 2 were on penicillin and had received pneumococcal vaccination, 3 were on penicillin without vaccination, but 2 were neither on penicillin nor had received the vaccine.
Thus, of the 15 patients with Howell-Jolly bodies now detected in their blood, only 9 (60 percent) had optimal prophylaxis against pneumococcal infection, receiving penicillin and having been vaccinated, 3 (20 percent) had incomplete prophylaxis in that they only received penicillin, and 3 (20 percent) had no prophylaxis at all (Table 2). Of the 23 patients without Howell-Jolly bodies in their blood, 2 (9 percent) were taking penicillin and had received the vaccine, while 7 (30 percent) were either on penicillin or had been vaccinated (Table 2).
Table 2. Penicillin prophylaxis and pneumococcal vaccination due to the presence of Howell-Jolly bodies in the blood.

Abdominal ultrasound not only has been recommended as a method of choice for splenic imaging, but has also been shown to be a reliable method with which to diagnose splenic status in children with visceral heterotaxy.10, 11 This is significant, since we failed to demonstrate a spleen in only three quarters of our patients with isomerism of the right atrial appendages, the syndrome frequently described as “asplenia”, while multiple spleens were found in only three quarters of the patients with isomerism of the left atrial appendages, so-called “polysplenia”. We did not find any instances of absence of the spleen in those with isomerism of the left atrial appendages, albeit that Uemura et al.2 have reported such an incidence on one-twentieth of such patients studied at autopsy. Solitary spleens of normal size, however, were demonstrated in patients known to have both left and right isomerism. Our ultrasonic findings, therefore, confirm the fact that the state of the spleen can vary markedly in patients with so-called visceral heterotaxy.2, 4, 5
Howell-Jolly bodies are unextruded nuclear inclusions found in erythrocytes circulating in the blood stream. They are a morphologic indicator of defective splenic function.12 Corazza et al.13 have shown that counting these bodies is a simple and sensitive method for identifying and monitoring those patients with a real risk of overwhelming infections. As expected, all our patients in whom we were unable to demonstrate a spleen using ultrasound had Howell-Jolly bodies circulating in their blood. To date, as far as we know, there have been two early reports describing Howell-Jolly bodies in patients with suspected isomerism of the atrial appendages and either multiple or normal spleens. Rodin et al.14 demonstrated Howell-Jolly bodies in a patient with multiple spleens, while Pearson et al.,15 reported on 2 infants known to have isomerism of the atrial appendages along with Howell-Jolly bodies despite having a normal spleen. We can now support these previous findings, as we found positive blood films in 2 of our patients with multiple spleens, and in 1 patient with a solitary normal spleen. It should also be noted, nonetheless, that Howell-Jolly bodies can be present transiently in healthy newborns and disappear as the infant matures.16, 17 In one of the 2 patients reported by Pearson et al.15 Howell-Jolly bodies could be observed at 14 days of age, but disappeared 3 weeks later. Similarly, in 3 of our patients with positive postnatal blood films, 2 with multiple spleens and 1 with a single normal spleen, Howell-Jolly bodies could no longer be detected in the current films.
Of further significance, and to the best of our knowledge not previously reported, is that we have identified 5 patients with initially normal blood films, but who were shown on present films to have Howell-Jolly bodies. Ours is the first study, therefore, to offer evidence that functional asplenia can develop in patients with visceral heterotaxy independent of the anatomical state of the spleen, since ultrasound: in 4 of these patients revealed multiple spleens in 2, absence of the spleen in 1, and a normal spleen in the other. Based on this experience, we suggest that a detailed ultrasonic scan to diagnose splenic state should be performed in any patient suspected to have visceral heterotaxy. As the situation with regard to Howell-Jolly bodies can change with age, patients known to have multiple or solitary but normal spleens should have their blood films monitored regularly, we suggest on a yearly basis.
Of the 74 patients originally identified with visceral heterotaxy, 23 did not survive to medium-term. Of these patients, three-tenths were known to have died from sepsis late after surgery, a proportion comparable with other series.6, 7 The majority of these were known to have true or functional asplenia. This high mortality due to sepsis may, in part, be a consequence of poor compliance for prophylaxis using penicillin and pneumococcal vaccination, which in itself is related to inadequate information provided to the patients, their parents, and their doctors.7, 18 We found that, amongst our cohort, parental knowledge of splenic status, and the potential risk for infection and thus compliance for penicillin prophylaxis and pneumococcal vaccination, was unsatisfactory. Only half of the parents with children known to have Howell-Jolly bodies in their blood had been informed about the potential risk for infection. Of these patients, one-fifth was without penicillin prophylaxis, and two-fifths had not been vaccinated against the pneumococcus. These findings endorse the notion that more needs to be done to inform parents, patients and doctors about the possible consequences of functional asplenia in patients with visceral heterotaxy.
It is significant in this respect that both antibiotic prophylaxis and pneumococcal vaccinations have been shown to reduce significantly the incidence of pneumococcal infections.19 Those patients who either have Howell-Jolly bodies in their blood smear, or are known to lack a spleen subsequent to abdominal ultrasound, therefore, should receive penicillin prophylactically as well as being vaccinated against the pneumococcus.20–22 In children younger than 2 months of age known to have Howell-Jolly bodies in the blood, the blood smear should be repeated in one month's time. Omitting prophylaxis with penicillin should be considered only if the abdominal ultrasound shows multiple spleens, or a normal sized spleen, and the Howell-Jolly bodies disappear from subsequent blood films. Due to the unforeseeable risk of developing functional asplenia at a later stage, all patients with visceral heterotaxy should be vaccinated against the pneumococcus. Should Howell-Jolly bodies be detected in subsequent blood films, prophylaxis with penicillin should be commenced immediately.
We conclude that Howell-Jolly bodies can be found in patients with visceral heterotaxy irrespective of the anatomical state of the spleen. As the presence of these bodies in the blood can change with age, we suggest that regular monitoring of blood films is warranted. Parental knowledge of the state of the spleen, with its potential risk for fatal infections and compliance for penicillin prophylaxis and pneumococcal vaccination, was unsatisfactory amongst the parents of our patients. If our experience is representative of that in other centres, then provision of better information for parents, patients, and doctors seems mandatory.

Abdominal ultrasonic findings in 37 patients with visceral heterotaxy. It proved impossible to perform an ultrasonic investigation in 1 patient with isomerism of the left atrial appendages.

Comparison of the anatomical state of the spleen as diagnosed by abdominal ultrasound with the results of testing for Howell-Jolly bodies in the peripheral blood.

Table 1.

Table 2.