Focal atrial tachycardia is an uncommon cause of supraventricular tachycardia in children.Reference Kang, Etheridge and Kantoch1 As a life-threatening complication, 10% of patients with focal atrial tachycardia develop tachycardia-mediated cardiomyopathy.Reference Medi, Kalman and Haqqani2 There is a high risk of heart failure in patients with incessant tachycardia (37%) and tachycardia originating from the atrial appendages (42%).
Medical therapy is the preferred treatment in younger children, who have a 50% chance of spontaneous resolution within the first year of life.Reference Kang, Etheridge and Kantoch1 However, medical therapy achieves control of focal atrial tachycardia only in 72% of children. Drug therapy is associated with the risk of serious adverse events in 5.8% of the patients. Catheter ablation of focal atrial tachycardia is successful in 81% of children at a mean age of 12.8 (95% confidence interval 12.0–13.7 years).Reference Kang, Etheridge and Kantoch1 Repeat catheter ablation due to ablation failure (7.2% of the procedures) or focal atrial tachycardia recurrence (9.6% of the procedures) was less effective (at 66%) with serious complication in 6% of the cases.
Multiple randomised controlled trials prove the effect of omega-3 fatty acids in cardiovascular disease. The American Heart Association recently updated prior recommendations for patients with prevalent coronary heart disease and patients with high risk of cardiovascular diseaseReference Siscovick, Barringer and Fretts3: Supplementation with omega-3 fatty acids is reasonable (class IIa) for the prevention of sudden cardiac death, coronary heart disease, and to improve outcome in patients with heart failure (class IIa). However, omega-3 fatty acids are not recommended for primary and secondary prevention of atrial fibrillation (class III).
We report on a 14-year-old boy with focal atrial tachycardia from left atrial appendage with failure of catheter ablation and medical therapy with metoprolol and flecainide. He received 2 g of omega-3 fatty acid supplementation while waiting on repeat ablation.
Case report
Arrhythmia in our patient was noted in cardiovascular monitoring during the operation of a radius fracture at the age of 14. The patient has never had palpitations before and cardiovascular monitoring during an operation at the age of 12 was equivocal. The 24-hour Holter electrocardiography confirmed the diagnosis of a focal atrial tachycardia, showing sinus rhythm alternating with supraventricular tachycardia. There was no clinical evidence for heart failure and echocardiography ruled out CHD or systolic dysfunction. Two months later, focal atrial tachycardia was confirmed prior to catheter ablation with the origin being the left atrial appendage. Catheter ablation was performed but was unsuccessful, and medical therapy was started with 47.5 mg metoprolol succinate and 100 mg flecainide. According to medical therapy, focal atrial tachycardia was reduced to one-third of the 24-hour Holter electrocardiographs (Fig 3). While waiting on repeat ablation, we started additional supplementation with 2 g omega-3 fatty acids per day (DAS gesunde PLUS Omega-3™ 1000 mg) 1 week later. This therapeutic approach was based on its reported antiarrhythmic properties in childrenReference Oner, Ozdemir and Doksoz4 which align with our own experience. If focal atrial tachycardia disappears within 4 weeks of omega-3 fatty acid supplementation, we are able to wean out the antiarrhythmic therapy within the next 4 weeks step-by-step (Fig 1). The time-table for the boy is shown in Figure 2a and b by 24-hour Holter electrocardiogram analysis: after catheter ablation and medical therapy with 1 mg/kilogram per day of metoprolol and 2 mg/kilogram per day of flecainide at day 108, the ongoing focal atrial tachycardia was terminated after additional omega-3 fatty acids at day 152. While weaning out antiarrhythmic therapy until day 182, we observed an increase of heart rate and decrease of heart rate variability, indicated by the vagal parameters RMSSD and pNN50, which spontaneously increased to normal values at day 250. Nine months after catheter ablation the boy is arrhythmia free, taking 2 g omega-3 fatty acids per day.
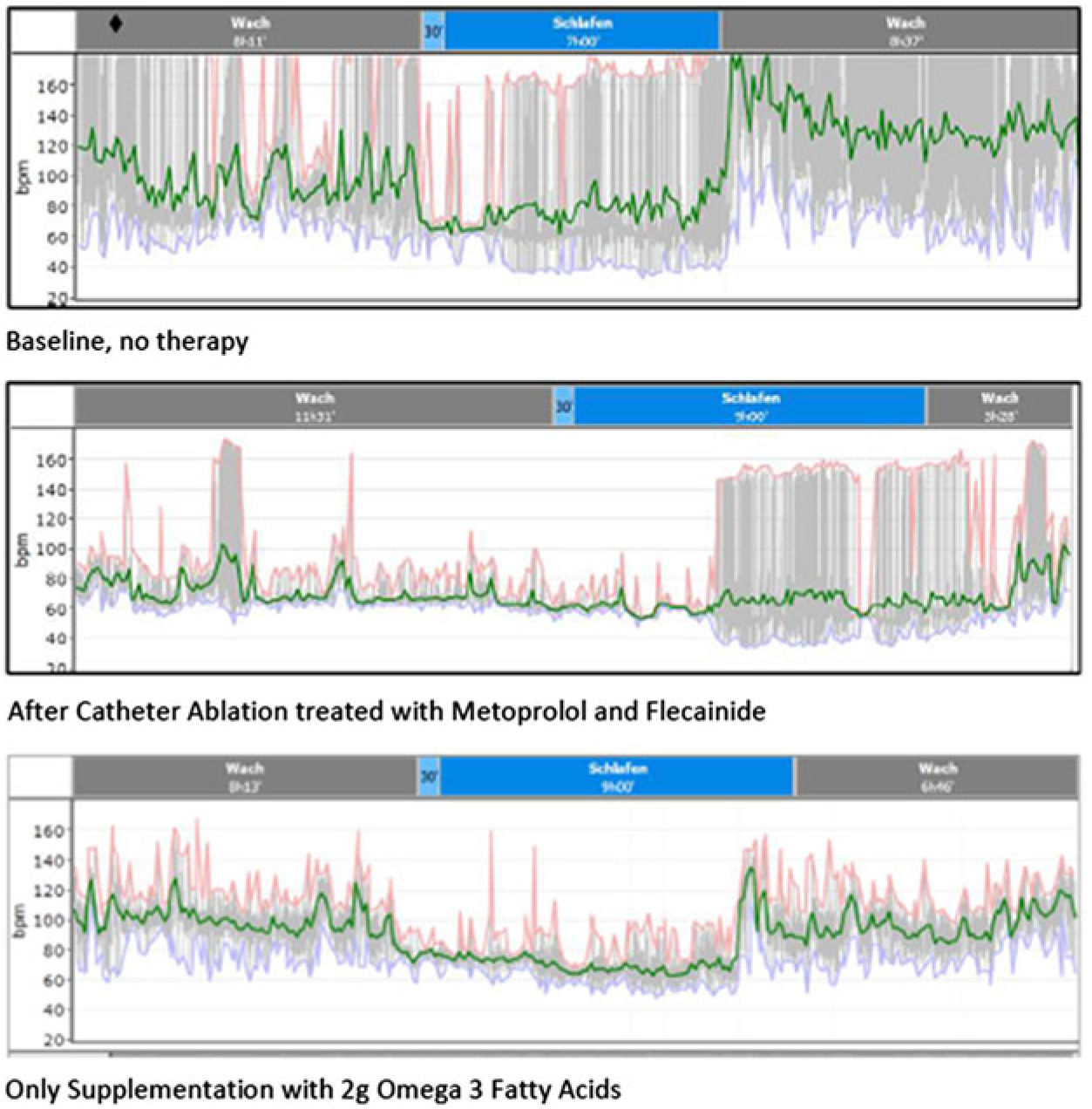
Figure 1. Original Holter ECG reprints demonstrating focal atrial tachycardia as gray bars indicating the deviation of the heart rate from the baseline: 1) Sinus rhythm alternating with focal atrial tachycardia the whole day without therapy 2) focal atrial tachycardia at night after catheter ablation with metoprolol/flecainide and 3) the resolution of focal atrial tachycardia after omega 3 fatty acid supplementation.

Figure 2. Timeline of heart rate variability analysis (2a time domaine analysis; 2b frequency domaine analysis) starting after diagnosis: During sinus rhythm alternating with focal atrial tachycardia up to catheter ablation and metoprolol/flecainide at day 121 the heart rate variability seems to be high. After resolution of focal atrial tachycardia with omega 3 fatty acid supplementation, the heart rate variability drop down to very low values that indicates severe autonomic dysfunction. The follow up until day 244 shows a slow recovery of heart rate variability.

Figure 3. ECG example showing focal atrial tachycardia after catheter ablation and a medical therapy with metoprolol and flecainide.
Discussion
The antiarrhythmic effect of omega-3 fatty acids on ventricular and atrial arrhythmias is still discussed. Billman published a critical reassessment of the effects of omega 3 fatty acids on cardiac rhythmReference Billman5:
Omega-3 fatty acids reduce the activity of membrane sodium channels in cardiomyocytesReference Xiao, Kang, Morgan and Leaf6 and modulate the activity of L-type calcium channels.Reference Hallaq, Smith and Leaf7
Based on his own experimental studies,Reference Billman5 Billman discusses how omega-3 fatty acids reduce baseline heart rate via alterations in the intrinsic pacemaker rate.
However, most authors assume that the antiarrhythmic properties of omega-3 fatty acids depend on the well-known effects on the autonomic nervous system as discussed by La Rovere and Christensen.Reference La Rovere and Christensen8 In summary, omega-3 fatty acids reduce heart rate and increase heart rate variability which indicates improvement of autonomic imbalance due to sympathetic dominance, a risk factor of arrhythmias. It is a methodological dilemma that a decrease of intrinsic heart rate ushers the increase of heart rate variability. Current methodological standards are not able to differentiate a lower intrinsic heart rate from a higher vagal activity by analysis of heart rate variability.
It is believed that the anti-inflammatory properties of omega-3 fatty acids contribute to their cardioprotective effects as shown in non-ischemic dilated cardiomyopathy.Reference Nodari, Triggiani and Campia9
We routinely use omega-3 fatty acids to modulate the autonomic nervous system in children with autonomic dysfunction due to multiple indications: recently, we demonstrated the highly significant effect of omega-3 fatty acids in children with reduced heart rate variability due to attention deficit disorder,Reference Buchhorn, Koenig and Jarczok10 short stature,Reference Buchhorn, Willaschek and Norozi11 and obesity.Reference Baumann, Rakowski and Buchhorn12 In all these children, heart rate significantly decreased and heart rate variability significantly increased. The effect of omega-3 fatty acids on heart rate is contradictory in our case that focal atrial tachycardia is stopped but the sinus rhythm heart rate increases from 80 to 90 bpm from prior to catheter ablation to after termination of antiarrhythmic therapy as shown in Figure 2a. We speculate that the underlying autonomic dysfunction in our case was veiled by the incessant focal atrial tachycardia, perhaps by beta receptor down regulation. After treating the autonomic nervous system with omega-3 fatty acids, focal atrial tachycardia was stopped and the underlying autonomic dysfunction was unmasked. Omega-3 fatty acids are incorporated into the phospholipid bilayer of cell membranes of the central nervous network rather than the heart. This mechanism may explain the observed delay between supplementation and the effects on heart rate.
Based upon the documented effects of omega-3 fatty acid supplementation on heart rate variability in children with attention deficit disorder, short stature, and obesity, we anticipate a beneficial effect of omega-3 fatty acid supplementation on the autonomic nervous system which may be important for children with arrhythmias. Our case demonstrates the resolution of a therapeutic-resistant focal atrial tachycardia after omega-3 fatty acid supplementation. However, if the arrhythmia had an artificial effect on heart rate variability, this case demonstrates the methodological limitations of heart rate variability analysis in these children.
Author ORCIDs
Reiner Buchhorn 0000-0003-3474-8239
Acknowledgements
We would like to thank Luise Hessing for editorial support.
Financial Support
This research received no specific grant from any funding agency, commercial or not-for-profit sectors.
Conflict of Interest
None.
Ethical Standards
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national guidelines on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008, and has been approved by the institutional committee (Caritas Krankenhaus Bad Mergentheim).





