Interventional cardiology for paediatric and congenital cardiac disease is a relatively young and rapidly evolving field. A common system of nomenclature for interventional cardiology is imperative, particularly as we go beyond evaluating our individual practice to establishing multi-institutional and multi-national databases.Reference Jacobs1–Reference Jenkins, Beekman and Bergersen5 The purpose of this two-part series of manuscripts is to present the version of nomenclature of The International Paediatric and Congenital Cardiac Code updated to include a new system of nomenclature for cardiovascular catheterisation for congenital and paediatric cardiac disease, focusing both on procedural nomenclature and the nomenclature of complications associated with interventional cardiology.
This manuscript is the second part of a two-part series. Part 1 covered the procedural nomenclature associated with interventional cardiology as treatment for paediatric and congenital cardiac disease.Reference Bergersen, Everett and Giroud6 Part 2 will cover the nomenclature of complications associated with interventional cardiology as treatment for paediatric and congenital cardiac disease. These two “companion” papers are designed to be read together. Specific complications related to transcatheter procedures involving arrhythmias, such as ablation and procedures involving pacemakers, are not included in this paper; these complications related to transcatheter procedures involving arrhythmias have already been discussed somewhat in prior publications from our groupReference Jacobs1 and likely will be addressed further in additional publications from our group. In order to place these papers in perspective, Part 1 begins with a brief summary of the history and current status of The International Paediatric and Congenital Cardiac Code and the IMPACT Registry™ (IMproving Pediatric and Adult Congenital Treatment) of the National Cardiovascular Data Registry®.
The creation of a comprehensive listing of complications associated with interventional cardiology as treatment for paediatric and congenital cardiac disease is crucial because of the increasing interest in the benchmarking and establishment of outcomes for these treatments. A critical component in the determination of outcomes after cardiac catheterisation is a comprehensive list of complications to serve as the basis for establishment of benchmarks related to the safety of patients. Using the process developed by The International Society for Nomenclature of Paediatric and Congenital Heart Disease during the creation of The International Paediatric and Congenital Cardiac Code, we describe the development of a comprehensive effort to develop a list of complications for the procedures associated with congenital cardiac catheterisation.
Methodology of the development of the list of complications of The International Paediatric and Congenital Cardiac Code
The basis for this long list of complications originated with the use of the structure and crossmap of terms developed by The International Society for Nomenclature of Paediatric and Congenital Heart Disease during the creation of The International Paediatric and Congenital Cardiac Code.Reference Franklin, Jacobs, Tchervenkov and Béland7–Reference Béland, Franklin and Jacobs12 The list was further refined by taking advantage of two large ongoing studies of outcomes after paediatric and congenital cardiac catheterisation in the United States of AmericaReference Jenkins, Beekman and Bergersen5: The Congenital Cardiac Catheterization Outcomes Project (C3PO)Reference Bergersen, Marshall and Gauvreau13 and the Mid-Atlantic Group of Interventional Cardiology (MAGIC).Reference Everett, Ringel and Rhodes14 This process allowed for the addition of further codes drawn from the experience of multiple cardiologists. In total, 329 codes of complications associated with congenital cardiac catheterisation were developed along with 166 codes for associated modifiers. The list of codes was particularly enhanced by incorporating the structure for modifiers used in the Congenital Cardiac Catheterization Outcomes Project for the following five variables (the first three of these variables are related to “process” and the last two of these variables are related to “outcome”):
• the relationship of the complication to a specific component of the procedure (such as related to the administration of sedation: “Sedation related”, or related to the dilation component of the procedure: “Dilation related”, etc.),
• the timing of the complication (in or out of the catheterisation laboratory, before access, after removal of sheaths, etc.),
• the preventability of the complication,
• the outcome of the complication, and
• the severity of the complication (none to catastrophic).
Results
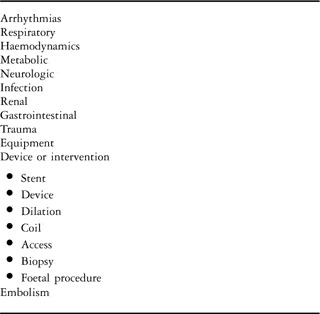
Using the International Paediatric and Congenital Cardiac Code and the hierarchical structure of the International Congenital Heart Surgery Nomenclature and Database Project of The European Association for Cardio-Thoracic Surgery and The Society of Thoracic Surgeons, codes for complications are broken down into main categories (Table 1) and then expanded in further detail beneath each branch level. For example, if tricuspid insufficiency is present after transcatheter closure of an atrial septal defect, the term “Trauma” is chosen from the level 2 of the hierarchy (Table 1), followed by the more detailed anatomic descriptor, “Heart valve”, and the specific complication “Tricuspid valve insufficiency, New onset”. Fully coded, this complication appears as:
“Cardiac catheterization, Complication, Trauma, Heart valve, Tricuspid valve insufficiency, New onset”.
Table 1 Complication code hierarchy main categories (level 2).
This complication equates to the following numerical codes and mapped terms in the version of The International Paediatric and Congenital Cardiac Code derived from the European Paediatric Cardiac Code of the Association for European Paediatric Cardiology:

This example illustrates how either version of The International Paediatric and Congenital Cardiac Code can be used by individual institutions for use in comparisons of outcomes. The complete lists of codes for complications associated with cardiovascular catheterization for congenital and paediatric cardiac disease, as laid out in the two versions of The International Paediatric and Congenital Cardiac Code described above, are available for free download at http://www.IPCCC.net. These lists are also available as electronic tables from the Cardiology in the Young Website at http://journals.cambridge.org/action/displayJournal?jid=CTY.
After coding a complication as described above, qualifiers for process and outcome subsequently are added as shown in Tables 2, 3, 4, and 5. The qualifiers for process include qualifiers for relationship, timing, and preventability. These qualifiers for process were developed, in part, to understand where, in the process of the procedure, the complication occurred. First, the qualifiers for process include qualifiers to document the relationship to a defined portion of the procedure, such as related to access, or related to placement of a device (such as, in the example above, an atrial septal defect occluder resulting in tricuspid insufficiency). Second, a complication is coded for the timing of the complication, such as “after sheaths inserted” or “with device release”, etc. Third, a qualifier for process is chosen to address the “preventability” of the complication.
Table 2 Complication code qualifiers for relationship or attributability.
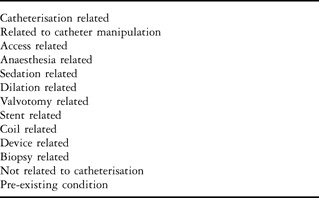
Table 3 Complication code qualifiers for timing.
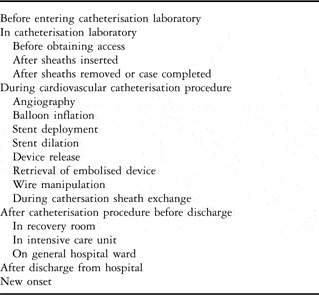
Table 4 Complication code qualifiers for preventability and definitions.

Table 5 Complication code qualifiers for severity and definitions.

Finally, qualifiers for outcome are also chosen for each complication. These qualifiers for outcome can provide more information about a complication. For example, the complication of “Metabolic acidosis” can be followed by the final outcome, such as “Resolved, Spontaneously”. The final qualifier for outcome is for the severity of the complication (Table 5). These codes to describe severity are subjective, but help stratify the significance of the complication. Please note that the complete detailed lists of nomenclature (shown in part in Tables 1, 2, 3, 4, and 5) are all available for free download at http://www.IPCCC.net. These lists are also available as electronic tables from the Cardiology in the Young Website at http://journals.cambridge.org/action/displayJournal?jid=CTY.
Discussion
Using the structure of The International Paediatric and Congenital Cardiac Code, we have developed a comprehensive set of terms to code for the complications related to cardiac catheterisation for paediatric and congenital cardiac disease. A key feature of this set of codes is the inclusion of qualifier codes for attributability that put the complication in the context of the process of catheterisation. This feature is essential for efforts designed to improve quality.
Currently, no uniform set of terms exist to code for the complications related to cardiac catheterisation for paediatric and congenital cardiac disease. Therefore, it is impossible to compare studies from individual centres to understand what the real risk of the cardiac catheterisation is to a specific patient. This problem is best exemplified by the recent single-institution reports by Mehta and colleaguesReference Mehta, Lee, Chaturvedi and Benson15 and Bergersen and colleaguesReference Bergersen, Gauvreau, Lock and Jenkins16 that document a rate of complications of 7.3% and 19%, respectively. Standardisation of the coding of complications related to cardiac catheterisation for paediatric and congenital cardiac disease, as described in this paper, is essential for meaningful analysis of multi-institutional studies. Importantly, the nomenclature and associated codes for complications listed in this paper are identical to those within the structure of The International Paediatric and Congenital Cardiac Code where they relate to complications associated with other strategies of management, such as for surgery or arrhythmias, and are thus compatible with other existing international surgical and cardiological databases.Reference Jacobs1







