Case report
A 34-month-old boy from a foreign country was admitted to our hospital for management of his CHD. Echocardiography revealed type A interrupted aortic arch with a perimembranous ventricular septal defect and dilated main pulmonary artery. CT confirmed the findings of echocardiography (Fig 1). Cardiac catheterisation was carried out and pulmonary vascular resistance was calculated as 8.9 WU·m2 at room air. It fell to 5.8 WU·m2 with 100% inspired oxygen.

Figure 1 Preoperative CT. ( a ) Anterior view. ( b ) Posterior view. AA=ascending aorta; DA=descending aorta; MPA=main pulmonary artery.
Surgery was carried out under aorto-bicaval cardiopulmonary bypass with additional cannulation through the patent ductus arteriosus. The ventricular septal defect was closed using a bovine pericardial patch with a 5.6 mm fenestration. Next, a generous portion of the anterior wall of the main pulmonary artery was resected and an autograft tube of diameter 12 mm was made using 6–0 polypropylene continuous suture. After complete removal of ductal tissue from the descending aorta, the autograft was anastomosed to the descending aorta using 6–0 polypropylene continuous suture. Anastomosis between the autograft and the distal ascending aorta was performed in an end-to-side fashion using 6–0 polypropylene continuous suture after advancing the aortic cannula into the innominate artery. The defect in the main pulmonary artery was repaired primarily. The cardiopulmonary bypass time was 292 minutes, the aortic cross-clamp time was 130 minutes, and the lower body ischaemia time was 68 minutes.
The patient could not be weaned from cardiopulmonary bypass because of pulmonary hypertension and right ventricular dysfunction. He underwent extracorporeal membrane oxygenation support for 3 days during which period pulmonary hypertension gradually regressed and right ventricular function improved. Postoperative course was complicated by mediastinal bleeding and small amount of subdural haematoma without neurologic sequelae. Echocardiography at discharge revealed left-to-right shunt through a ventricular septal defect fenestration and normal biventricular systolic function. Postoperative CT showed wide patent aortic arch with natural geometry and patent left main bronchus (Fig 2).
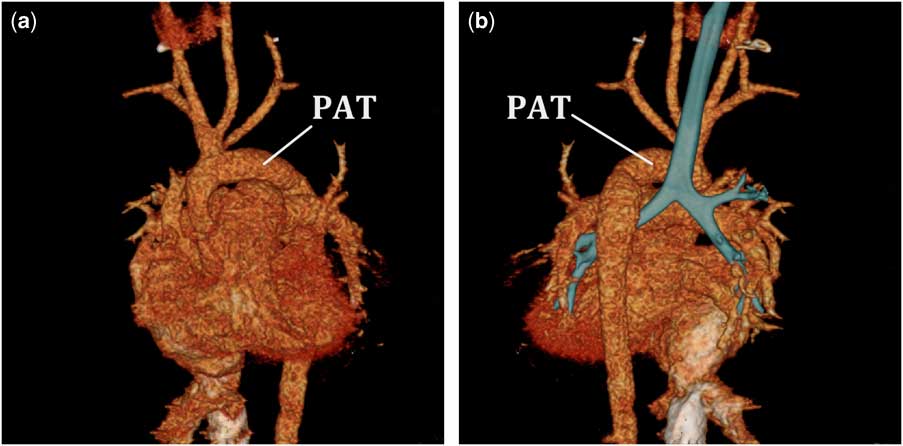
Figure 2 Postoperative CT. ( a ) Anterior view. ( b ) Posterior view with reconstructed airway showing patent left main bronchus. PAT=pulmonary autograft tube.
Discussion
There are several options for the repair of interrupted aortic arch.Reference McCrindle, Tchervenkov and Konstantinov 1 , Reference Jegatheeswaran, McCrindle and Blackstone 2 Among several techniques used for the repair of interrupted aortic arch, direct anastomosis is the most commonly used.Reference McCrindle, Tchervenkov and Konstantinov 1 , Reference Jegatheeswaran, McCrindle and Blackstone 2 However, it may cause several problems including anastomotic site stenosis due to excessive tension, left main bronchus compression, and acute-angled aortic arch.Reference Hussein, Iyengar and Jones 3 Ou et al found that acute-angled aortic arch (gothic arch) geometry was associated with late systemic hypertension in patients who had undergone successful repair of coarctation of the aorta.Reference Ou, Bonnet and Auriacombe 4 Interposition of a prosthetic graft is another option for repair of interrupted aortic arch. Although this technique may be helpful in avoiding tension on suture lines and preventing left main bronchus compression, the prosthetic graft has no growth potential with unacceptably high reintervention rate.Reference McCrindle, Tchervenkov and Konstantinov 1
In the present case, we used a pulmonary autograft tube to avoid the potential problems of conventional techniques for interrupted aortic arch repair. This technique was originally reported by Bergoënd et al.Reference Bergoënd, Bouissou, Paoli, Roullet-Renoleau, Duchalais and Neville 5 Our patient presented late with resultant long distance between the ascending and descending aorta. We thought that direct anastomosis in this patient might result in excessive tension on suture line and/or left main bronchus compression. There was no arch-related complication and the geometry of the aortic arch was satisfactory. Regarding growth potential of the graft, we believe that the pulmonary autograft tube will grow in accordance with the patient’s somatic growth. Bergoënd et al showed a good growth of the pulmonary autograft tube by CT performed 3 years after the repair.Reference Bergoënd, Bouissou, Paoli, Roullet-Renoleau, Duchalais and Neville 5 However, as with other uses of autologous pulmonary arterial tissue in the systemic circulation, the risk for aneurysmal dilation is not insignificant. Careful long-term follow-up is mandatory.
In conclusion, repair of interrupted aortic arch using a pulmonary autograft tube can be a good option in selected patients because of its ability of maintaining natural arch geometry, growth potential, and beneficial effect in preventing compression of the left main bronchus.
Acknowledgements
None.
Financial Support
This research received no specific grant from any funding agency, commercial or not-for-profit sectors.
Conflicts of Interest
None.





