A 15-year-old adolescent was brought to our institution because of chest pain, orthopnoea, and pharyngalgia. He had experienced an upper respiratory infection 1 week before admission. On admission, his temperature was 37.6°C and pulse rate was 116 beats per minute. His respiratory rate was 22 per minute, and he had mild goiter and thyroid tenderness. There were no wheezes, rhonchi, or basilar rales bilaterally. Cardiac examination showed strong heart sounds at the apex, with third heart gallop. His serum levels of total triiodothyronine/thyroxine, free triiodothyronine/thyroxine increased, and thyroid-stimulating hormone decreased (Table 1). The serum was negative for antithyroglobulin antibody, antimicrosomal antibody, and thyroid-stimulating hormone-binding inhibiting immunoglobulin (Table 1). The C-reactive protein was 40.80 milligrams per litre and the erythrocyte sedimentation rate was 37 millimetres per hour. His leukocyte count was 10,050 per microlitre with left shift. A thyroid scan showed a markedly decreased uptake of 99m technetium–pertechnetate and thyroid iodine uptake rate. These findings were compatible with the thyrotoxic phase of subacute thyroiditis. The initial electrocardiogram showed a regular sinus tachycardia with ST segment extensively elevation except AVR and V1 leads (Fig 1). All indicators of myocardial damage – creatine kinase MB isoenzyme, high-sensitivity Troponin T, and aspartate aminotransferase – increased strikingly (Table 2). A chest X-ray picture at that time showed enlargement of the heart shadow (Fig 2). Transthoracic echocardiography demonstrated left ventricular hypokinesia – left ventricular ejection fraction was 34%. On the second day of admission, the chest pain and dyspnoea became worse, and he was given a selective beta-blocker (Metoprolol), diuretics, and Trimetazidine. There was great clinical improvement during the following 5 days. His chest pain and dyspnoea disappeared. Repeated electrocardiography began to show the segment of ST recovered and diffuse T-wave inversion on the 6th day of admission (Fig 1). With the clinical and myocardial zymogram improved, the chest radiography (Fig 2) and echocardiography demonstrated left ventricular rehabilitation; 12 days after admission, left ventricular ejection fraction increased to 64%. The thyroid function test indicated that his serum levels of total triiodothyronine/thyroxine, free triiodothyronine/thyroxine, and thyroid-stimulating hormone were showing signs of recovery. The presence of Epstein–Barr virus, cytomegalovirus, and Rubella rubivirus deoxyribonucleic acid in plasma were negative, and serum virus-specific antibodies to cytomegalovirus, type I herpes, and cytomegalovirus were not found during the course of illness.
Table 1 Results of thyroid function tests.

T3 = triiodothyronine; T4 = thyroxine; TGAb = thyroglobulin antibody; TG = thyroglobulin; TMAb = antimicrosomal antibody; TSH = thyroid-stimulating hormone

Figure 1 Changes of electrocardiogram during the admission. Sinus tachycardia and diffuse ST elevation were seen on admission. Distinguished sinus tachycardia was observed on day 2. Elevated ST segment recovered on day 6 after admission. Diffuse T-wave inversion occurred on day 13.
Table 2 Biochemical studies at admission and during the admission.

AST = aspartate aminotransferase; CK = creatine phosphokinase; CK-MB = creatine kinase MB isoenzyme; CRP = C-reactive protein; MYO = myoglobin
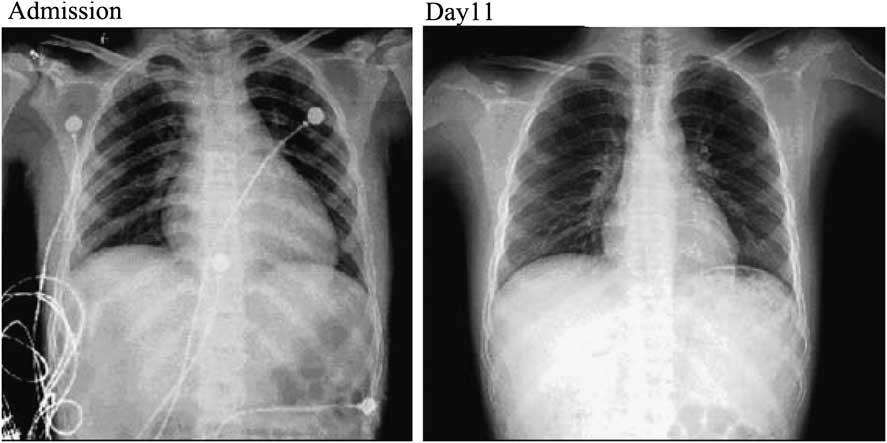
Figure 2 Chest radiography of the patient. The heart shadow enlarged on the day of the admission. The heart shadow returned to normal 10 days after admission.
Discussion
Subacute thyroiditis, known as de Quervain's disease, is a self-limiting inflammatory disorder of the thyroid gland in which a viral infection has most often been implicated as the cause. Compared with Graves’ disease and Hashimoto's thyroiditis, subacute thyroiditis is uncommon, occurring at the rate of about 1 case per 5 cases of Graves’ disease and 1 case per 15 or 20 cases of Hashimoto's thyroiditis.Reference Guimaraes 1 Although the disease has been described at all ages, it is rare in children. Subacute thyroiditis commonly occurs in middle-aged women; female patients outnumbered male patients in a ratio of 3–6:1, and there is a preponderance of cases in the third to fifth decades.Reference Singer 2 – Reference Volpe 3 A recent study of Mayo Clinic result showed an age- and sex-adjusted incidence of 4.9 cases per 100,000 per year.Reference Fatourechi, Aniszewski, Fatourechi, Atkinson and Jacobsen 4 Viral infection is the most common cause of the disease. Often, it is preceded by pharyngitis, which subsides a week or two before the symptoms of thyroiditis appear. Subacute thyroiditis is diagnosed on the basis of goiter tenderness and pain, increased serum thyroid hormone levels, suppressed throtropin level, markedly increased systemic inflammatory signs – C-reactive protein and erythrocyte sedimentation rate – and decreased uptake of 99m technetium–pertechnetate on the thyroid scan.Reference Szabo and Allen 5 , Reference Ogawa, Katsushima, Fujiwara and Iinuma 6 Various clinical representations of subacute thyroiditis have been reported.Reference Daniels 7 – Reference Nishihara, Ohye and Amino 9
Myocarditis is an insidious disease, which is usually asymptomatic, and thus important clues to its epidemiology come from postmortem studies. Recent prospective postmortem data have implicated myocarditis in sudden cardiac death of young adults at rates of 8.6–12%.Reference Fabre and Sheppard 10 , Reference Doolan, Langlois and Semsarian 11 Myocarditis is far more common in children than in adults. The World Health Organization reports that the incidence of cardiovascular involvement after enteroviral infection is 1–4%, depending on the causative organism. Most often, myocarditis is a result of various viral infections. Myocarditis may present with a wide range of symptoms, ranging from mild dyspnoea, palpitation, or chest pain, which resolves without specific therapy, to cardiogenic shock and death.
The symptoms of this patient may lead to confusion between thyroid storm and subacute thyroiditis. Thyroid storm is a life-threatening syndrome characterised by exaggerated clinical manifestation of thyrotoxicosis, including fever, tachycardia, hypertension, mental confusion, gastrointestinal disorders, and heart failure, supported by an extremely elevated thyroid hormone parameter. In this patient, the myocarditis was unlikely to have been caused by the thyroid dysfunction induced by subacute thyroiditis, as the myocarditis recovered before the thyrotoxic states. Furthermore, the cardiovasular deficits were improved not for management of thyrotoxicosis during the thyrotoxic phase. Another differential diagnosis is painful Hashimoto's thyroiditis, which is an atypical variant of Hashimoto's thyroiditis characterised by thyroid pain, fever, goiter, hypothyroidism, and antibodies titre are not always elevated. Pathologic characteristics include advanced fibrosis and destructive thyroid architecture. In front of a clinical picture of subacute thyroiditis with no or little response to, painful Hashimoto's thyroiditis must be considered. In this case, as pharyngalgia of the patient was relieved without anti-inflammatory treatment, painful Hashimoto's thyroiditis is not supported.
Immune mechanisms have been implicated in the pathogenesis of both thyroid and myocardial disease. Therefore, we should not ignore the potential autoimmunity in the development of the cardiac damage as in our case. In the present case, the electrocardiographic findings shifted quickly from sinus tachycardia and ST elevation to global T-wave inversion in a short period of time, and echocardiographic findings favored the diagnosis of acute myocarditis, instead of autoimmunity.
To our knowledge, a few similar case reports have been reported. Yet this is the first reported case of quick recovery of myocardium damage associated with subacute thyroiditis. As subacute thyroiditis most probably represents a viral disease, a common underlying pathomechanism such as common virus to thyroid and myocardium is the possible explanation of our case, although we did not detect any abnormal virus antibody levels and deoxyribonucleic acid in the patient's serum.






