Introduction
Congenital heart disease (CHD) is one of the common forms of birth defects in newborn babies. Reference van der Linde, Konings and Slager1 CHDs with univentricular circulation are defined as lesions where one of the two ventricles are too small to sustain the pulmonary or systemic circulation. Reference Frescura and Thiene2 These occur at a prevalence of 4.4/10,000 live births. Reference Steinberger, Ferencz and Loffredo3,Reference O’Leary4 Outcomes for these complex CHDs have significantly improved in recent years, though these require multiple-staged palliative procedures in the initial years of life. Reference O’Leary4–Reference Raissadati, Nieminen, Jokinen and Sairanen6 Recent reports have indicated feasibility and good short-term outcomes with single ventricle palliation in low-and-middle-income countries. Reference Schidlow, Gauvreau and Cherian7 Lifelong specialist cardiac review is required for these patients and additional neurodevelopmental and psychological issues cause further concern for longer-term survivors. Reference Zentner, Celermajer and Gentles8,Reference Wernovsky9 The medical and socio-economic challenges involved in the care of these complex CHDs may be very challenging for patients and their families in the setting of low-and-middle-income countries. Reference Kumar and Shrivastava10,Reference Raj, Paul and Sudhakar11
Screening of the fetal heart is routinely offered as a part of the mid-trimester anomaly scan in all pregnancies in developed countries. Reference Carvalho, Allan and Chaoui12–Reference Donofrio, Moon-Grady and Hornberger14 Inclusion of the four-chamber view in screening programs has shown a high sensitivity for the detection of complex CHDs like the functionally univentricular hearts. Reference Copel, Pilu, Green, Hobbins and Kleinman15–Reference Sonek, Kagan and Nicolaides17 Early prenatal diagnosis of complex CHDs gives more options to expectant families including the option of termination of pregnancy, thereby potentially reducing the post-natal prevalence of these defects. Reference Bull18–Reference Levey, Glickstein and Kleinman20 Recent studies from developed countries reported longitudinal follow-up until Fontan operation after prenatal diagnosis of univentricular heart and identified risk factors for adverse perinatal outcomes in these patients. Reference Beroukhim, Gauvreau, Benavidez, Baird, LaFranchi and Tworetzky21,Reference Liu, Zielonka, Snarr, Zhang, Gaynor and Rychik22 However, despite the availability of guidelines for mid-trimester anomaly (18–20 weeks) scans in India, evaluation of the fetal heart is seldom performed in mass screening programs. Reference Khurana, Makhija and Deka23 The Medical termination of pregnancy act of India was introduced in 1971 before the era of routine fetal ultrasound and it provides guidelines for termination of pregnancy in India until the gestational age limit of 20 weeks. 24 However, since many complex fetal anomalies including CHD are detected in the later stages of pregnancy, an amendment for this act has been proposed recently to increase the upper gestational age limit for termination of pregnancy. 25 Considering the challenges involved in the care and follow-up for complex CHDs in low-and-middle-income countries, prenatal diagnosis can potentially enhance parental decision-making options and this can impact the perinatal outcomes for these defects.
In this retrospective 10-year study, we analysed pregnancy and early post-natal outcomes of fetuses diagnosed with functionally univentricular heart in the setting of a low-and-middle-income country.
Methods
Study setting and design
This hospital-based retrospective study was conducted in the setting of a tertiary paediatric cardiac centre. The centre offers high-quality cardiac care accessible by the general population of Kerala, South India amounting to around 35 million. The annual number of live births in Kerala is around 500,000. All pregnant women in Kerala have universal access to antenatal care and most patients are offered a minimum of two ultrasound evaluations, either free of cost or at nominal rates (including a mid-trimester anomaly scan). A dedicated Fetal Cardiology division was initiated in our centre in 2008 with the specific goal of improving the availability of prenatal diagnosis of CHD in Kerala and provide counselling and options for prenatal and perinatal care. All fetuses with a diagnosis of functionally univentricular heart during the period of January, 2008–October, 2019 from our database were included in the analysis.
Inclusion and exclusion criteria
All fetuses with a diagnosis of functionally univentricular heart diagnosed during the study period were included in the analysis. Fetuses with borderline ventricle size were classified as hypoplastic when the ventricle length (measured from atrioventricular valve annulus to endocardium at apex) z-score was less than −2 and asymmetric when the z-scores where >−2; those with asymmetric ventricles were excluded from the analysis. Reference Schneider, McCrindle, Carvalho, Hornberger, McCarthy and Daubeney26
Fetal echocardiography and counselling protocol
All patients underwent a detailed evaluation of fetal heart as per standard recommendations. Reference Carvalho, Allan and Chaoui12–Reference Donofrio, Moon-Grady and Hornberger14 This included the standard imaging protocols in the transverse and sagittal planes along with the additional views as per indications and evaluation of the fetal heart rate and rhythm. Following the fetal diagnosis, the attending fetal cardiologist provided detailed counselling to the family about management options, expected outcomes in our centre, long-term concerns and expected costs of treatment including the hospital expenses for multi-staged surgical procedures, outpatient clinic visits and long-term medications. Our centre routinely performs all surgical procedures involved in the multi-staged palliation of all forms of single ventricle hearts, from the inception of the period of this study. The final decision regarding the management of pregnancy was taken by the respective families and the referring obstetrician based on family’s preferences and the outcomes were reported retrospectively.
Study variables and groups
Since 2008, a dedicated fetal cardiology database was initiated including maternal variables, indication for referral, fetal variables, details of cardiac diagnosis, pregnancy outcomes and post-natal outcomes in the live-born fetuses. The maternal variables included in the analysis included maternal age, gravidity, gestational age at referral, indication for fetal echocardiography, associated comorbidities (diabetes mellitus, maternal infections like febrile illnesses in the first trimester, rubella and influenza, exposure to potential teratogenic drugs), mode of conception and consanguinity. Reference Jenkins, Correa and Feinstein27 Fetal variables included the presence of hydrops, extra-cardiac anomalies, nuchal translucency and family history of CHD in previous children. Nuchal translucency values > 95th centile was taken as abnormal. Reference Nicolaides, Heath and Cicero28 We included details about the socio-economic class by Modified Kuppuswamy Scale, type of family (nuclear or joint), religion and educational status of the parents in the prospective cohort subset of patients (January, 2017 onwards). Reference Sharma29
Fetuses with a diagnosis of functionally univentricular heart were further sub-classified into the following sub-groups for analysis:
-
Based on anatomical type – the anatomic cardiac diagnosis.
-
Based on ventricular morphology – dominant left or right ventricle.
-
Based on outflow tract anatomy – systemic outflow obstruction, pulmonary outflow obstruction or no outflow tract obstruction. The presence of obstruction was primarily assessed by the size of the respective outflow and calculation of the z-scores; values of < −2 were considered to be small and suggestive of obstruction. Reference Schneider, McCrindle, Carvalho, Hornberger, McCarthy and Daubeney26
Outcome variables
The perinatal outcomes analysed in this study included pregnancy outcomes and early post-natal outcomes.
Pregnancy outcomes included the following:
-
Non-continued pregnancies: This information was recorded as reported by the families by telephone enquiry. This included the termination of pregnancy and spontaneous intrauterine fetal death. Fetal autopsy for confirmation of the cardiac diagnosis was not performed.
-
Live births.
-
Lost to follow-up.
For the live-born babies, the details of the mode of delivery, birth weight, sex and presence of comorbidities (extra-cardiac anomalies, genetic syndromes, birth-related complications and neonatal sepsis) were noted. The attending paediatric cardiologist confirmed the cardiac diagnosis and provided a detailed counselling about prognosis and management options to the patient’s families. Post-natal care was offered as per parental choices and was classified as intention-to-treat (if there was an intention to provide specialised cardiac care), comfort care (basic neonatal care with no specialised cardiac care) or no post-natal data. Decisions regarding comfort care were channelised through the palliative care services of our hospital after obtaining informed consent from the parents. In those with intention-to-treat, we recorded the details of the cardiac procedures performed (surgery or catheter-based) for initial palliation (Stage 1) as well as the subsequent stages in the single ventricle palliation (bidirectional Glenn shunt, one and a half ventricle repair and the Fontan procedure). The clinical status of the patient until the last available follow-up (alive, dead or lost to follow-up) was recorded.
The study was approved by the Institutional Review Board (date 18 February, 2020; IRB-AIMS-2020-095).
Statistical analysis
We summarised categorical variables as numbers (percentages) and continuous variables as mean, median (Interquartile range). Chi-square test was used to compare the categorical variables associated with pregnancy outcome and survival status on follow-up. Independent sample t-test was used to compare the continuous variables associated with pregnancy outcome and survival status. Multiple binary logistic (Forward conditional) regression analysis was used to estimate odds ratio with 95% CI of risk factor for non-continued pregnancy outcome and survival status on follow-up. Statistical analyses were conducted using SPSS Version 20.0 for Windows (IBM Corporation ARMONK, NY, United States of America).
Results
A total of 504 fetuses were diagnosed with functionally univentricular heart during the period of January, 2008–October, 2019. The mean maternal age was 27.5 ± 4.8 years. The mean gestational age at diagnosis was 25.6 ± 5.7 weeks. The most common reason for referral was suspicion of CHD in screening ultrasound (n = 485; 96.2%). Majority of the fetuses were singleton pregnancies (97.1%). Maternal risk factors included diabetes mellitus (46; 9.1%), exposure to teratogens (8; 1.6%) and intrauterine infections (12; 2.4%). Associated fetal anomalies included extra-cardiac anomalies (57; 11.3%) and hydrops fetalis (8; 1.6%). Nuchal translucency measurements were reported in 217 patients (43.1%) only; of these 38 fetuses (7.5%) had values > 95th centile. The baseline characteristics of the study patients are summarised in Table 1.
Table 1. Baseline characteristics of patients included in the study (n = 504)
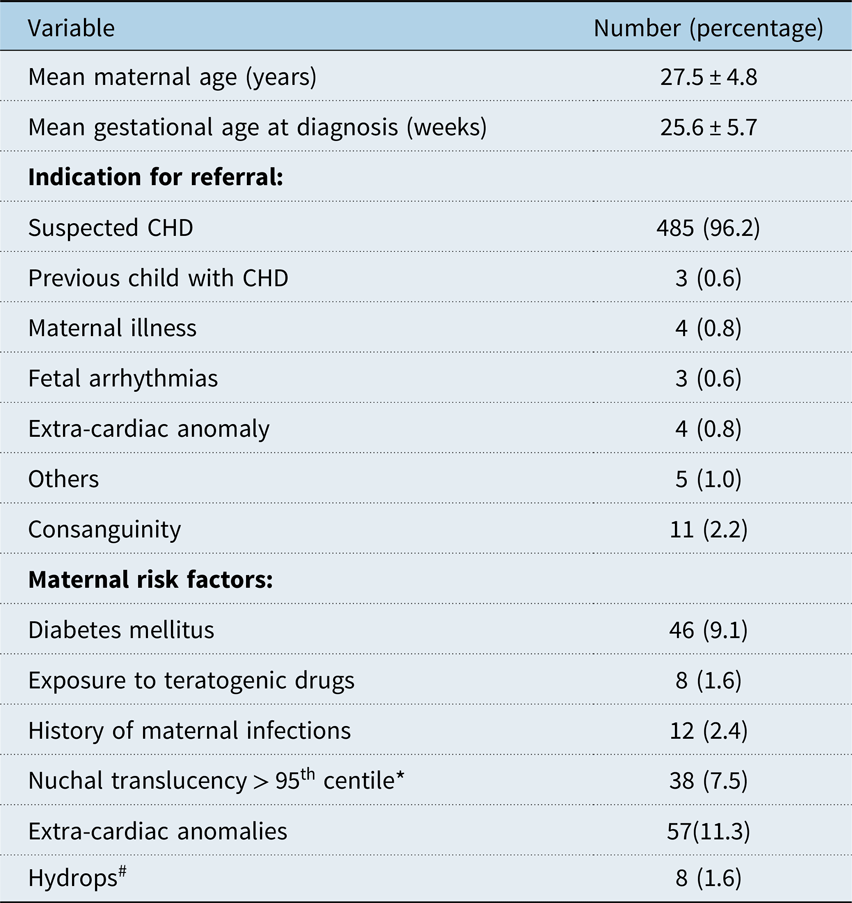
* Nuchal translucency measurements were reported in only 217 patients (43.1%).
# In six cases, hydrops was related to the cardiac diagnosis (pulmonary atresia with intact ventricular septum with hypoplastic dysfunctional RV and severe tricuspid regurgitation in three, Heterotaxy in two and tricuspid atresia with restrictive foramen ovale in one). In two cases (complex double outlet RV with hypoplastic LV and Dextrocardia with double inlet LV), hydrops was due to non-cardiac reasons.
Types of single ventricle
The various types of functionally univentricular heart based on anatomical subtype are summarised in Table 2. Based on the ventricular anatomy, 281 fetuses (55.8%) had a dominant right ventricle while the rest (n = 223, 44.2%) had a dominant left ventricle. Pulmonary outflow obstruction was reported in 224 fetuses (44.4%), systemic outflow obstruction in 153 (30.4%) while 127 fetuses (25.2%) had no outflow obstruction.
Table 2. Types of single ventricle based on anatomy, ventricular morphology and outflow tracts

# Heterotaxy syndromes included complex CHD with unbalanced atrioventricular septal defect with associated intra-cardiac defects.
* Others – Left atrioventricular valve atresia with single ventricle – 30; Large ventricular septal defect amounting to single ventricle – 13, Hypoplastic right ventricle with VSD – 19.
Pregnancy outcomes
Of the total 504 fetuses, 272 (54%) had non-continued pregnancies including termination of pregnancy (n = 256, 50.8%) or intrauterine fetal death (n = 16; 3.2%). Live births were reported in 215 fetuses (42.7%) while 17 (3.3%) were lost to follow-up. On univariate analysis, gestational age at diagnosis, presence of hydrops and associated extra-cardiac anomalies impacted pregnancy outcomes (Table 3). However, on multivariate analysis, only gestational age at diagnosis had a significant association with the pregnancy outcomes. The mean gestational age at diagnosis was significantly lower in non-continued pregnancies compared with those with live births (22.5 ± 3.5 vs.29.7 ± 5.7; p < 0.001). Other factors like maternal age, cardiac diagnosis, type of ventricular morphology or outflow tract obstruction also did not influence the pregnancy outcomes.
Table 3. Univariate analysis of predictors of pregnancy outcome

DORV = double outlet RV; HLHS = hypoplastic left heart syndrome; LV = left ventricle; PA/IVS = pulmonary atresia with intact ventricular septum; RV = right ventricle.
* This data is available in a cohort of 57 patients who were prospectively enrolled into this study from January, 2017 onwards.
In a prospective cohort of 57 fetuses (12.9%) included in this study after January, 2017, we had included a socio-economic questionnaire including the socio-economic class, type of family, religious background and educational status of the parents. Of these 57 cases, 18 (31.6%) had live births and the remaining 39 (68.4%) had non-continued pregnancies. None of the socio-economic or cultural factors had an impact on pregnancy outcomes (Table 3).
Neonatal and follow-up outcomes
Of the 215 live births, 98 (45.6 %) were delivered in tertiary cardiac centres, while the remaining (117; 54.4%) were delivered in non-cardiac units. The mean gestational age at delivery was 37.9 ± 1.2 weeks and the mean birth weight was 2.9 ± 0.3 kg; 113 (52.6%) babies were male. Twelve patients (5.6%) had associated comorbidities including genetic syndromes (n = 5), extra-cardiac anomalies (n = 4), prematurity or growth restriction (n = 2) or neonatal sepsis (n = 2).
Intention-to-treat and provision of cardiac care was the parental choice in 119 (55.3%) of the live-born babies. Eighty nine (74.8%) of these underwent surgical procedures; 14 (11.8%) required catheter-based interventions while the remaining 16 were continued on medications alone. Of these, 35 patients (16.2%) required Stage 1 palliative procedures (Table S1) in the neonatal period. Fifty-one patients (23.7%) underwent Stage 2 procedures including bidirectional Glenn shunt (n = 47; 21.9%) or “one and a half ventricle repair” for pulmonary atresia with intact septum (n = 4; 1.9%). Seventeen (7.9%) of the live-born infants completed Stage 3 Fontan procedure. In 79 patients (36.7%), the parents opted for comfort care, while in 17 infants (7.9%), no post-natal data was available. Cardiac diagnosis, ventricular morphology and type of outflow obstruction impacted the decision on the type of post-natal care offered (Table 4). Table S2 lists the cardiac diagnoses of patients undergoing staged procedures after birth.
Table 4. Comparison of variables between intention-to-treat and comfort care in live-born babies (n = 215)

DORV = double outlet right ventricle; HLHS = hypoplastic left heart syndrome; LV = left ventricle; PA/IVS = pulmonary atresia with intact septum; RV = right ventricle.
* Others – Left atrio-ventricular valve atresia with single ventricle 10; Large ventricular septal defect amounting to Single Ventricle – 10, Hypoplastic Right ventricle with VSD – 9.
On follow-up, median duration 10 (range 1–120) months, 106 (49.3%) of the 198 patients with post-natal data were alive; 85 (39.5%) died, while 7 (3.3%) were lost to follow-up. Ninety-five (79.8%) of the patients with intention-to-treat survived. Univariate analysis of predictors of survival on follow-up in live-born babies is summarised in Table 5. On multi-variate analysis, the only variable which impacted survival status on follow-up was intention-to-treat or comfort care (survival 79.8% in intention-to-treat vs. 12.9% in comfort care group; p < 0.001).
Table 5. Univariate analysis of variables impacting survival status on follow-up in live-born infants

DORV = double outlet right ventricle; HLHS = hypoplastic left heart syndrome; LV = left ventricle; PA/IVS = pulmonary atresia with intact septum; RV = right ventricle.
Figure 1 depicts the flowchart of the pregnancy and post-natal outcomes of the patients included in this study.

Figure 1. Flowchart describing study patients with pregnancy and post-natal outcomes.
Discussion
This retrospective study of 504 fetuses diagnosed with a functionally univentricular heart showed an overall low survival status of affected fetuses, both in pregnancy and in post-natal life. About half of the affected pregnancies were not continued to term and about a third of live-born babies did not have an intention-to-treat, resulting in an overall survival of about 20% on the last follow-up (Fig 1). Earlier gestational age at diagnosis significantly impacted pregnancy outcomes (Table 3). Amongst live births, cardiac diagnosis and ventricle morphology (systemic left ventricle) impacted parental decisions regarding intention-to-treat (Table 4). Most patients (>80%) with intention-to-treat underwent cardiac procedures (especially Stages 1 and 2); the final stage Fontan procedure was completed in 17 patients during the available follow-up period. Survival on follow-up was significantly impacted by parental decisions towards intention-to-treat or comfort care; about 80% of patients opting for specialised cardiac care were alive on the last follow-up (Table 5). Maternal or fetal comorbidities, socio-economic status, religion or educational status of the parents did not impact parental decision-making (Table 3).
Previous studies have reported higher prevalence of termination of pregnancy when the prenatal diagnosis of complex CHD is made in early gestation. Reference Jicinska, Vlasin and Jicinsky16–Reference Levey, Glickstein and Kleinman20 The first-trimester screening resulted in a lower prevalence of complex CHDs during the second trimester as well as post-natal period. Reference Jicinska, Vlasin and Jicinsky16 In a population-based analysis, Bull et al reported termination rates of 70 and 61% when a diagnosis of CHD was made before 19 and 23 weeks, respectively. Reference Bull18 Beroukhim et al reported a higher rate of termination for fetuses with univentricular hearts when the diagnosis was made before 24 weeks. Reference Beroukhim, Gauvreau, Benavidez, Baird, LaFranchi and Tworetzky21 Tararbit et al reported that of the 703 fetuses diagnosed with CHD, 46% were terminated, with 3.2 times higher odds of termination in those diagnosed before 22 weeks. Reference Tararbit, Bui, Lelong, Thieulin, Goffinet and Khoshnood30 Other studies also have reported the lack of impact of factors like ventricular morphology, maternal age or other fetal comorbidities on pregnancy outcomes. Reference Bull18–Reference Beroukhim, Gauvreau, Benavidez, Baird, LaFranchi and Tworetzky21 In the setting of a low-and-middle-income country, besides the gestational age at diagnosis, factors like economic burden, concerns about the long-term health and quality of life of a child with complex CHD and the potential impact of the affected child on the future of the family and other children might have influenced the pregnancy outcomes reported in this study. Reference d’Udekum, Iyengar, Galati, Forsdick, Weintraub and Wheaton5,Reference Raissadati, Nieminen, Jokinen and Sairanen6,Reference Zentner, Celermajer and Gentles8,Reference Wernovsky9
The overall low utilisation of cardiac care in the live-born babies in this study is different from reports from the developed world where the majority receive specialised cardiac care. Reference Beroukhim, Gauvreau, Benavidez, Baird, LaFranchi and Tworetzky21,Reference Liu, Zielonka, Snarr, Zhang, Gaynor and Rychik22 This is despite the fact that all palliative surgeries for univentricular heart were being performed in our centre from the inception of the study. A recent report had highlighted the feasibility of single ventricle palliations in the setting of low-and-middle-income countries with encouraging early outcomes. Reference Schidlow, Gauvreau and Cherian7 We observed that intention-to-treat and cardiac procedures were more common in patients with systemic left ventricle, which has been shown to be associated with better long-term Fontan outcomes. Reference Beroukhim, Gauvreau, Benavidez, Baird, LaFranchi and Tworetzky21,Reference Liu, Zielonka, Snarr, Zhang, Gaynor and Rychik22 The medical costs of the staged single ventricle palliation pathway will consume about 5 times the average per capita annual income of a family in Kerala. 31 In addition, the annual clinic visits, evaluation and medications will exceed an average monthly income. Though government-funded schemes have been initiated for the care of children with CHD in Kerala and other states of India, the actual costs of care far exceed the support provided. Reference Kumar and Shrivastava10,32 In the setting of a univentricular heart, where the threat of a failing Fontan pathway looms large with advancing years after the surgery, the overall impact on an average family can be devastating in most healthcare systems of the world, especially those in the low-and-middle-income countries. Reference Deal and Jacobs33,Reference Rychik34 The challenges of providing long-term care for the survivors of these complex CHDs may prove overwhelming for low-and-middle-income countries with an ever-increasing number of patients surviving tertiary cardiac care into adult life. Reference Zentner, Celermajer and Gentles8–Reference Raj, Paul and Sudhakar11,Reference Deal and Jacobs33–Reference Raj, Sudhakar, Roy, Champaneri, Joy and Kumar35 Policymakers and funding agencies need to develop strategies for providing extended support for follow-up care of these patients and not merely fund the cost of the surgical procedures in order to take care of complex CHDs feasible for affected families. Reference Musa, Hjortdal and Zheleva36
The results of this study highlight the importance of early pregnancy screening of the fetal heart, especially in the low-and-middle-income countries. Most of the complex forms of CHD of the univentricular type can be suspected using the four-chamber view with a high degree of sensitivity. Reference Copel, Pilu, Green, Hobbins and Kleinman15 In Kerala, the cost of an anomaly scan is very nominal in government hospitals (less than 500 Indian Rupees or approximately 7 US Dollars), especially for patients in the low-income groups. Fetal echocardiography in advanced centres cost around 3000 Indian Rupees (approximately 40 US Dollars). Compared to the long-term costs of care of a child with univentricular heart, the costs of prenatal diagnosis are thus quite nominal. Suspicion of a complex CHD on screening should initiate a downstream process of referral, detailed evaluation by a fetal cardiologist, counselling and enhanced parental options for decision-making. Early prenatal diagnosis by implementing a mandatory screening policy may a very cost-effective strategy for the care of children with CHD in low-and-middle-income countries by reducing the burden of complex CHDs, permitting more efficient utilisation of resources towards the care of more correctable CHDs. Reference Vijayaraghavan, Sudhakar, Sundaram, Kumar and Vaidyanathan37
The strengths of the study include the large number of patients including the different anatomic subsets of functionally univentricular hearts and a near-complete pregnancy and early post-natal follow-up data. However, the limitations include inclusion of retrospective data and possibility of referral bias. Gestational age was calculated on the basis of the date of the last menstrual period alone and not based on ultrasound parameters. The role of socio-economic factors in deciding pregnancy outcomes and type of post-natal care was not comprehensively studied. A longer-term follow-up is needed to determine the further course of patients surviving in the intention-to-treat group until the completion of all stages of the single ventricle pathway and post-Fontan clinical outcomes.
In conclusion, prenatal diagnosis of functionally univentricular hearts was associated with an overall low survival status on follow-up. Early detection of these complex lesions by improved prenatal screening can enhance parental options and reduce resource impact in low-and-middle-income countries.
Supplementary material
To view supplementary material for this article, please visit https://doi.org/10.1017/S1047951120002929
Acknowledgements
The authors would like to acknowledge the contribution of Dr John Simpson MD, FRCP, Professor of Paediatric and Fetal Cardiology, Evelina London Children’s Hospital. London, United Kingdom for critically reviewing the manuscript.
Financial disclosure
The authors have no financial relationships relevant to this article to disclose.
Funding sources
There were no funding sources relevant to this article to disclose.
Potential conflicts of interest
The authors have no conflicts of interest relevant to this article to disclose.
Contributors’ statement
Balu Vaidyanathan conceptualised and designed the study, carried out the data analysis, drafted and edited initial manuscript, reviewed and revised the final manuscript and shall act as the guarantor and corresponding author for the manuscript.
Aparna Vijayaraghavan conceptualised the study, collected and analysed the data, drafted the initial manuscript and revised the manuscript.
Stephy Thomas collected data, carried out the initial analyses and reviewed the manuscript.
Abish Sudhakar designed the data collection instruments, collected data, carried out the initial analyses and reviewed and revised the manuscript.
All the authors approved the final manuscript as submitted and agreed to be accountable for all aspects of the work.
What’s already known about this topic?
Prenatal diagnosis of univentricular heart is associated with the overall high utilisation of post-natal specialised cardiac care in live-born infants in developed countries.
What does this study add?
In the setting of low-and-middle-income countries, prenatal diagnosis of functionally univentricular heart is associated with overall high rates of non-continued pregnancies and low utilisation of specialised cardiac care in live-born babies, despite the availability of tertiary paediatric cardiac services.









