During pregnancy, cardiac disease is the leading cause of maternal mortality. Reference Knight, Bunch, Tuffnell, Shakespeare, Kotnis, Kenyon and Kurinczuk1 With advancements in diagnosis and treatment of congenital heart disease (CHD), more than 90% of these patients will reach childbearing age. Reference Buber and Valente2 There is an increase in maternal age at first pregnancy, and the prevalence of acquired cardiovascular disease and cardiovascular risk factors in women of childbearing age is increasing. 3,Reference Janion-Sadawska, Sadowski, Zandecki, Kurzawaski, Polewczyk and Janion4 This presents an ever-growing cohort of women with underlying cardiac disease that may wish to undertake pregnancy.
Pregnancy poses a physiological stress on the cardiovascular system required to sustain the growth and development of the fetus and successfully deliver the baby. Reference Lu, Wu and Wang5,Reference Sanghavi and Rutherford6 These haemodynamic alterations potentially increase the risk of adverse cardiovascular events and potential fetal complications for women with underlying cardiac disease. Reference Lu, Wu and Wang5,Reference Drenthen, Pieper and Roos-Hesselink7,Reference Drenthen, Boersma, Balci, Moons, Roos-Hesselink and Mulder8 These women are also at risk from potential medication exposure as prescribed cardiovascular medications such as warfarin, angiotensin-converting enzyme inhibitors, and beta blockers are known or suspected to have teratogenic or adverse fetal effects. Reference Rakusan9 The greatest risk for exposure and the potential development of birth defects is during the first trimester. Such risks can be minimised or avoided completely if medications are reviewed and changed as required prior to pregnancy or once pregnancy is confirmed, or where changes cannot be made, pre-conception counselling can enable discussions about possible screening and development of a management plan if fetal malformations occur. Reference Clapp and Bernstein10 Women should be advised to take vitamin supplementation including folic acid 3 months prior to conception and during the first trimester to reduce the risk of birth defects in the offspring with evidence to show it can also reduce the risk of fetal congenital heart defects. 11–Reference Liu, Joseph and Luo13 Accurate risk stratification and pre-conceptual counselling are imperative to enable patients with cardiac disease to make informed decisions about potentially undertaking a high-risk pregnancy, optimising cardiovascular status prior to conception, planning appropriate contraception to avoid a pregnancy, and preparation and guidance for possible fertility treatments.
The Royal College of Obstetricians and Gynaecologists recommends girls with CHD and women with a new diagnosis of cardiac disease should be referred to a joint cardiac obstetric clinic for pre-conceptual counselling when they reach puberty. Reference Roos-Hesselink, Budts and Walker14,15 In recent years, a number of risk stratification tools have been developed including CARPREG, Reference Silversides, Grewal and Mason16 ZAHARA, Reference Drenthen, Boersma, Balci, Moons, Roos-Hesselink and Mulder8 and the modified World Health Organization classification, Reference Thorne, MacGregor and Nelson-Piercy17 whereby the individual’s cardiac condition and their physiological state determine their level of risk of adverse cardiovascular events during pregnancy. The most widely used Modified WHO classification categorises patients as being at low, moderate, high risk, or pregnancy is contraindicated. While risk stratification tools are helpful to categorise underlying cardiac conditions, they cannot be used in isolation to predict outcomes for individuals and the impact of pregnancy. Thus risk assessment needs to be individualised taking into account relevant investigations and previous obstetric history. Reference Roos-Hesselink, Budts and Walker14 This is reflected in the recent European Society of Cardiology 3 and American Heart Association Reference Mehta, Warnes and Bradely18 guidelines that state pre-conceptual counselling is indicated in every woman with known or suspected cardiac disease and advise that risk estimation requires an electrocardiogram, echocardiography, and an exercise test as a minimum.
To evaluate the effectiveness of pre-conceptual counselling against the European Society of Cardiology guidelines, we audited the new referrals to the joint obstetric cardiology clinics at Birmingham Women’s Hospital and compared pre-conceptual counselling in patients referred in two separate 12-monthly time periods. Furthermore, we hoped to identify whether the implementation of a multidisciplinary meeting in 2017 improved our ability to effectively deliver pre-conceptual counselling and whether subsequent European Society of Cardiology guidelines were fulfilled.
Methods
In this comparative retrospective audit, data were collected via electronic patient records of women attending joint obstetric cardiology clinics at a single centre, tertiary maternity unit in Birmingham, United Kingdom. Data were collected for those patients attending clinics between 1 January, 2015 and 31 December, 2015 (group 1) and between 1 July, 2018 and 30 June, 2019 (group 2). In total, 56 and 79 patients were reviewed during the respective audit periods in these two groups. Twelve patients were excluded in group 2 due to incomplete records.
Electronic medical records were used to collate baseline characteristics including maternal age, ethnicity, cardiac diagnoses, past medical history, medications, echocardiogram findings, New York Heart Association (NYHA) functional class, investigations performed prior to the clinic, and previous obstetric history. Cardiac disease in this cohort was classified as congenital, arrhythmia, aortopathy, cardiomyopathy, and rheumatic valvular disease or miscellaneous. Those classified as miscellaneous included women with previous heart transplant, cardiac sarcoid, ischaemic heart disease, and postural orthostatic tachycardia syndrome. Patients were risk stratified in accordance with the modified World Health Organization classification as either I, II, II–III, III, or IV. Reference Thorne, MacGregor and Nelson-Piercy17 Medical records were reviewed to determine whether patients had received any pre-conceptual counselling or advice and whether any risks had been clearly and accurately documented prior to pregnancy clinic attendance. Of those who received pre-conceptual counselling, medical records were reviewed to identify whether the appropriate investigations had been performed in accordance with the European Society of Cardiology guidelines. 3 These were deemed to be an electrocardiograph and an echocardiogram within a year and a functional test, either an exercise tolerance test, stress echocardiogram, or cardiopulmonary exercise test, within 3 years prior to counselling.
The multidisciplinary meeting was introduced in 2017. It composed of cardiologists with a specialist interest in obstetric cardiology, fetal–maternal medicine obstetricians, obstetric anaesthetists, fellows, nurse specialists, and midwives who would meet prior to joint obstetric cardiology clinics to review referrals, investigations and formulate management plans. Prior to this, patients were referred to the clinic and reviewed jointly by a cardiologist and fetal–maternal medicine obstetrician at the consultation.
Data are expressed as the number of patients and percentage in brackets. Statistical analysis of data was measured using the unpaired Student’s t-test with p-values <0.05 considered significant.
Results
Group 1
Fifty-six patients were reviewed during the first audit period between 1 January, 2015 and 31 December, 2015. Patient demographics are shown in Table 1.
Table 1. Baseline characteristics.

Baseline patient characteristics. *p < 0.05, **p < 0.01
Percentages are rounded to nearest whole number. Some patients were on multiple cardiovascular medications
The mean age at delivery was 31 ± 6 years, range 20–41 years. According to their diagnosis, 25 (45%) had CHD, and most had previous surgical intervention during childhood. Ten (18%) were diagnosed with arrhythmias, nine (16%) aortopathy, six (11%) cardiomyopathy, and four (7%) rheumatic valvular disease. Two (3%) of the patients were classified as miscellaneous given their diagnoses of aortic regurgitation and post heart transplant.
Prior to pregnancy, 14 (25%) patients were taking beta blockers and 4 (7%) angiotensin inhibitors: two patients were on both beta blockers and angiotensin inhibitors. Five (9%) were anti-coagulated (two also on beta blockers and one on both beta blockers and angiotensin inhibitors in addition).
With respect to the modified World Health Organization classification, 28 (50%) of the patients were classified as WHO I, 12 (22%) WHO II, 8 (14%) WHO II–III, and 8 (14%) WHO III, (Table 2). No patients were classified as WHO IV, in whom pregnancy would be contraindicated.
Table 2. Modified WHO classification class for 2 groups.
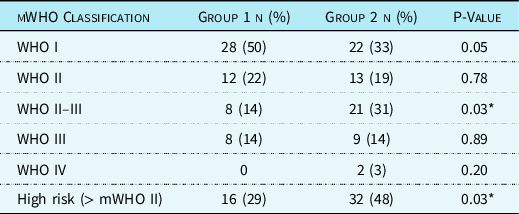
Number of patients and percentages stratified by modified World Health Organization (mWHO) classification for both group 1 and 2. *p < 0.05
Percentages are rounded to nearest whole number
Twenty-five (45%) of the patients with an underlying cardiac condition had received some pre-conceptual counselling but only 10 (40%) of these patients had specific maternal risks of pregnancy and potential fetal complications clearly documented in the electronic patient records (Table 3). Of those who received pre-conceptual counselling, 21 (84%) had an electrocardiograph and 22 (88%) had an echocardiogram performed within a year before counselling. Nine (36%) patients had an appropriate functional exercise test within 3 years prior to counselling.
Table 3. Pre-conceptual counselling documentation investigations.

Number of patients who received pre-conceptual counselling and those with accurate risk documentation for both group 1 and 2. Of those who received pre-conceptual counselling, the number of patients who had appropriate investigations prior to counselling is also given
When stratified according to cardiac diagnosis, there were significant differences between those with CHD and those with alternative diagnoses (Table 5). Sixteen (64%) of the women with CHD attending clinic had received pre-conceptual counselling compared with nine (29%) women with an alternative diagnosis (p < 0.01). Nine (36%) of the women with CHD compared with one (3%) woman with an alternative cardiac diagnosis had risks documented (p < 0.005).
There were significant differences in the delivery of pre-conceptual counselling when stratified according to modified World Health Organization classification as being at high risk, mWHO II–III, III, or IV. Eleven (69%) women classified as high-risk received documented pre-conceptual counselling compared with 14 (35%) women at low risk (p < 0.05). There were no significant differences in risk documentation. Five (31%) women at high risk and five (13%) women at low risk had risks accurately documented.
Group 2
Seventy-nine patients were reviewed during the second audit period between 1 July, 2018 and 30 June, 2019 (Table 1). Twelve patients were excluded due to incomplete patient records.
The mean age at delivery was 29 ± 6 years, range 17–43 years. Forty (60%) had a diagnosis of CHD with surgical intervention performed during childhood. Ten (15%) had arrhythmias, three (5%) aortopathy, five (7%) cardiomyopathy, and five (7%) rheumatic valvular disease. Four (6%) of the patients were classified as miscellaneous with diagnoses of ischaemic heart disease, cutaneous sarcoid, and postural orthostatic tachycardia syndrome.
Prior to pregnancy, 15 (22%) were taking beta blockers and 8 (12%) were anti-coagulated. One patient was taking both beta blockers and anticoagulation. No patients were taking an angiotensin inhibitor.
Classification according to the modified World Health Organization classification identified 22 (33%) patients assigned WHO I, 13 (19%) WHO II, 21 (31%) WHO II–III, and 9 (14%) WHO III (Table 2). Two (3%) of the women were classified as WHO IV in whom pregnancy would be contraindicated.
Thirty-one (46%) of the patients received some pre-conceptual counselling, but only 18 (58%) of these patients had the maternal and fetal risks accurately documented in the electronic patient records (Table 3). Of those who received pre-conceptual counselling, 28 (90%) patients had an electrocardiograph and 30 (97%) had an echocardiogram performed within a year before counselling. Sixteen (52%) patients had an appropriate functional exercise test within 3 years prior to counselling.
There were significant differences when patients were stratified according to cardiac diagnosis (Table 4). Twenty-seven (68%) of the women with CHD attending clinic had received pre-conceptual counselling compared with four (15%) women with an alternative diagnosis (p < 0.001). Sixteen (40%) of the women with CHD compared with two (7%) women with an alternative cardiac diagnosis had risks documented (p < 0.001).
Table 4. Congenital and non congenital heart diseases in 2 groups.

Number of patients who received pre-conceptual counselling and accurate documentation of risks stratified by cardiac diagnosis of congenital heart disease (CHD) for both group 1 and 2.
****p < 0.001, ***p < 0.005, **p < 0.01, *p < 0.05.
Twenty-two (69%) of the women classified as high-risk (mWHO II–III, III, or IV) received pre-conceptual counselling compared with nine (26%) at low risk (p < 0.0001), Table 5. Risk documentation was significantly better in those at high risk, 14 (44%), compared with four (11%) at low risk (p < 0.005).
Table 5. Outcomes.

Number of patients receiving pre-conceptual counselling and accurate documentation of risks stratified by mWHO classification for both group 1 and 2. Low risk defined as mWHO I or II and high risk defined as mWHO II–III and above. ****p < 0.001, ***p < 0.005, **p < 0.01, *p < 0.05.
The baseline patient characteristics of group 1 and group 2 were not significantly different (Table 1). There was also a 15% increase in the proportion of patients with CHD in group 2 (p = 0.098). There was a significant increase in the proportion of patients in group 2 classified as high-risk, mWHO II–III, III, or IV (p < 0.05). There were no significant differences in the number of patients receiving pre-conceptual counselling between the two groups. Despite a modest increase in the documentation of the risks in group 2, this was not significant (p = 0.23).
Twenty-five patients (45%) in group 1 underwent a successful pregnancy following pre-pregnancy counselling prior to the introduction of the European Society of Cardiology Guidelines. Of these patients, 21 (84%) delivered at term with four (16%) premature deliveries: two for maternal cardiac reasons. In total, 44% had a spontaneous vaginal delivery. With regard to group 2 patients who have received pre-pregnancy counselling within the last 2 years, not all pregnancies have been undertaken or completed, and the full impact of these guidelines cannot be fully assessed yet.
Discussion
Our data show that many women with underlying cardiac conditions are not receiving documented pre-conceptual counselling prior to referral to the joint obstetric cardiology clinic as recommended by the European Society of Cardiology guidelines. Reference Janion-Sadawska, Sadowski, Zandecki, Kurzawaski, Polewczyk and Janion4 Fewer than half of the women with underlying cardiac conditions received pre-conceptual counselling. This is similar to Vigl et al’s Reference Vigl, Kaemmerer and Seifert-Klauss19 reported findings in women with CHD.
The majority of patients who received pre-conceptual counselling had prior electrocardiograph and echocardiograms performed. However, only a third in group 1 had an exercise test performed. While we noted a modest non-significant increase, only half of the patients in group 2 had received an appropriate functional test prior to clinic attendance. In group 2, there was a non-significant 15% increase in the proportion of patients with CHD attending clinic, reflecting an increase in survival of CHD into adulthood. Reference Khairy, Ionescu-Ittu, Mackie, Abrahamowicz, Pilote and Marelli20
Discussions surrounding pregnancy and contraception in adult CHD patients should begin before transition from paediatrics to adult services and with every encounter in the hospital and outpatient settings Reference Roos-Hesselink, Budts and Walker14,Reference James21 providing, in theory, multiple opportunities for pre-conceptual counselling, contraception, and fertility advice. This may account for the significantly higher proportion of patients with CHD attending clinic who had received prior pre-conceptual counselling compared with those with alternative diagnoses. However, there are still a number of patients with unplanned pregnancies or those who did not have timely pre-conception counselling.
A multidisciplinary meeting was introduced in 2017 with an aim of considering additional relevant investigations required for each patient to improve counselling. The multidisciplinary meeting may account for this modest increase in the number of appropriate investigations being performed in group 2, enabling individualised pre-conceptual counselling in accordance with the subsequent guidelines produced by European Society of Cardiology in 2018. 3 However, there is still a significant amount of work required to improve this. It is hoped the publication of these recommendations in September 2018 will continue to improve the proportion of patients having appropriate investigations performed to enable accurate pre-conceptual counselling, although the full impact of this guidance cannot be fully assessed in this study.
There was also an increase in complexity of cardiac disease over the time period as indicated by a significant increase in women classified as being high-risk, mWHO II–III, and above (p < 0.05), comparable to that found by Cauldwell et al, Reference Cauldwell, Steer and Swan22 reflecting a large proportion of women at increased risk that would benefit from specialist services. This increase in complexity could partially account for the increase in the relevant investigations as per European Society of Cardiology guidelines. While the delivery of pre-conceptual counselling is significantly better in women classified as high-risk and those with CHD, a number of these women did not receive documented pre-conceptual education, which requires improvement.
Patients outside of this cohort, particularly those with valvular problems, cardiomyopathy, or pre-existing coronary artery disease, are often looked after by various cardiologists. Morgan et al 2019 Reference Morgan, Nana and Kinnaird23 identified a large proportion of women of childbearing age post coronary intervention who were discharged on cardiac medications (anti-platelet agents and statins for example) with known or unknown teratogenic effects without documented evidence of a discussion surrounding safety during pregnancy. A subsequent focus group demonstrated a failure to prioritise pre-conceptual counselling in secondary care and a lack of awareness of safety data. Reference Morgan, Nana and Kinnaird23 This is particularly significant considering cardiomyopathy, ischaemic and valvular heart disease collectively contribute to more than half of maternal mortality attributable to cardiac disease, and almost a quarter of the women who died were known to have a pre-existing cardiac problem. Reference Knight, Bunch, Tuffnell, Shakespeare, Kotnis, Kenyon and Kurinczuk1 Lack of detailed knowledge and awareness of the guidelines are frequently identified as barriers to general practitioners providing pre-conceptual care to women, Reference Ojukwu, Patel, Stephenson, Howden and Shawe24,Reference Kizirian, Black, Musgrave, Hespe and Gordon25 and while many paediatric cardiologists discuss pregnancy with their patients, up to a third were not comfortable in recommending contraception in women with CHD. Reference Cribbs, Briston and Zaidi26 It is evident that there is a real need for an increase in awareness, knowledge, and education regarding pre-conceptual counselling for all clinicians.
Around a quarter of women attending clinic were of non-Caucasian ethnicity. Ethnicity disproportionately affects maternal mortality with black women five times and Asian women two times more likely to die during pregnancy or in the early post-partum period compared with Caucasian women. Reference Knight, Bunch, Tuffnell, Shakespeare, Kotnis, Kenyon and Kurinczuk1 Some women born outside of the United Kingdom may present with undiagnosed CHD in early adulthood or with the complications of rheumatic heart disease both of which are not often encountered in the United Kingdom. Reference Zuhlke and Acquah27 Underlying medical comorbidities, previous pregnancy complications, and inadequate use of antenatal care are more prevalent in ethnic minority groups, Reference Nair, Kurinczuk and Knight28,Reference Nair, Knight and Kurinczuk29 and such women are high risk during pregnancy, and subsequently specialist pre-conceptual counselling is crucial. Lack of information, differences in cultural practices, and language barriers have been suggested to influence access to antenatal care, and subsequent work to better understand these differences will help to identify ways to reduce this disparity. Reference Nair, Kurinczuk and Knight28,Reference Higginbottom, Evans, Morgan, Bharj, Eldridge and Hussain30 We need to continue to improve the accessibility of our service to all cardiac women of reproductive age.
In both cohorts of patients, approximately a third were taking cardiovascular medications during pregnancy, similar to findings of the Registry of Pregnancy and Cardiac Disease report. Reference Ruys, Maggioni and Johnson31 A prospective study of women with cardiac disease attending pre-conceptual counselling clinic identified that 8 out of 10 patients taking cardiovascular medications were unaware if their current medication was safe in pregnancy, Reference Cauldwell, Steer and Swan22 leaving a cohort of patients that were unsure.
Up to 30% of UK pregnancies are unplanned, Reference James21 and women with cardiac disease have high rates of unplanned pregnancies which may reflect access and acceptability of pre-conceptual counselling, contraception, and fertility guidance. Reference Chor, Rankin, Harwood and Handler32,Reference Lindley, Madden, Cahill, Ludbrook and Billadello33 While attitudes towards pre-conceptual counselling are largely positive, many women are hesitant to seek pre-conception care themselves. Reference van der Zee, de Beaufort, Steegers and Denktas34 Clinicians should be proactive in discussing pregnancy with each consultation and not rely on the patient to raise the issue Reference Silversides, Grewal and Mason16,Reference Allen, Hunter, Wood and Beeson35 particularly given it is well documented that there is a lack of awareness amongst women with cardiac conditions of their potential increased risk during pregnancy. Reference Vigl, Kaemmerer and Seifert-Klauss19,Reference Chor, Oswald, Briller, Cowett, Peacock and Harwood36–Reference Miner, Canobbio and Pearson39 Cauldwell et al Reference Cauldwell, Steer and Swan22 identified that prior to preconceptual counselling, fewer than half of women with cardiac disease felt they were well informed about the risks of future pregnancy despite discussions with other healthcare professionals prior to referral to the specialist maternal cardiac clinic. It has also been documented that women with CHD are more likely to downplay the severity of their cardiac disease, Reference Ngu, Hay and Menahem40 highlighting the need for specialist and individualised pre-conceptual counselling in this population of women.
All women benefit from pre-conceptual counselling, providing an opportunity for health promotion including diet, exercise, smoking cessation, optimising cardiovascular haemodynamics to optimise a woman’s health prior to conception, with the aim of improving both maternal and child health outcomes. Reference Mason, Chandra-Mouli, Baltag, Christiansen, Lassi and Bhutta41,42 Therefore, all clinicians providing care to women of childbearing age should consider the possibility of future pregnancy. Simply asking whether the woman is considering pregnancy in the coming months, as encouraged with the “One Key Question ®” tool 11,Reference Allen, Hunter, Wood and Beeson35,Reference Bellanca and Hunter43 at each contact may be an effective method to increase the delivery of pre-conceptual counselling and contraceptive advice that is not just limited to a high-risk cohort of patients as was highlighted in CHD group.
There is a need for improvement to increase the delivery of pre-conceptual counselling to women with cardiac disease. We have shown that there is an increase in demand for specialist pre-conceptual counselling for women with cardiac disease. Reference Cauldwell, Steer and Swan22 While more studies to determine the efficacy and address any barriers or areas for improvement in this service are required, women who received pre-conceptual counselling were largely highly satisfied with their experience, and it enabled them to make an informed decision regarding pregnancy. Reference Cauldwell, Steer and Swan22 Additional improvements for patients are still required, and incorporation of a specialist midwife and psychologist to the multidisciplinary meeting and clinic process would further improve the overall experience and provide a point of contact and well-being support. Implementing an education programme for all multidisciplinary staff within cardiology to increase awareness of the risks of pregnancy in women with cardiac disease and encourage discussions surrounding future pregnancies in women of childbearing age should improve the delivery of pre-conceptual counselling in this cohort of women.
Limitations
This audit contains retrospective data from a small cohort of patients at a single centre. There are some incomplete patient records. Furthermore, some women were referred from other Trusts once already pregnant meaning possible pre-conceptual counselling provided elsewhere was not fully captured. The European Society of Cardiology guidelines were published in September 2018, and hence the full impact of these recommendations is not completely identified. Pregnancy outcome in group 2 patients could not be undertaken because of the shorter duration since their pre-conception counselling.
Conclusion
Many patients with cardiac disease are not receiving the pre-conceptual counselling and lifestyle advice that they deserve and are recommended by the European Society of Cardiology, American Heart Association, and Royal College of Obstetricians and Gynaecologists, with less than half of the women receiving pre-conceptual counselling and even fewer having such risks documented clearly in the patient records. Over 3 years there was a significant increase in the number of high-risk pregnancies, but only a modest increase in the number receiving pre-conceptual counselling and appropriate investigations.
There is a great need for improvement in the availability and delivery of pre-conceptual counselling throughout the growing cohort of women with cardiac disease wishing to undertake pregnancy. We need to provide all women with the opportunity to make an informed decision about their fertility. Each medical interaction from the teenage years provides a potential opportunity and at present is a “missed opportunity”.
Acknowledgements
Cardiac investigation unit – Queen Elizabeth Hospital Birmingham
Medical records – Birmingham Women’s Hospital
Financial support
None.
Conflict of interest
None.








