In small children, the diameter of the vessels comprises a significant limitation for catheter interventions.Reference Vitiello, McCrindle, Nykanen, Freedom and Benson1 Introducing sheaths with inadequate French size can lead to serious complications, such as vessel scarring or occlusion.Reference Burrows, Benson and Williams2 The Glidesheath Slender (Terumo, Tokyo, Japan) is an innovative sheath initially developed for radial arterial access in adult patients scheduled for coronary interventionsReference Aminian, Dolatabadi and Lefebvre3 with a thinner wall and hydrophilic coating (Fig 1). As a consequence, the outer diameters are one French smaller than those of regular sheaths of corresponding inner diameter. For example, a 5F Glidesheath Slender has an inner lumen of 5F and an outer diameter of a 4F regular sheath. Hence, the vessel trauma (risk for tearing, scarring, and vessel occlusion) may be reduced with this innovative approach in small patients. Downsizing of the outer sheath diameter may extend percutaneous treatment possibilities in the field of paediatric interventional cardiology.
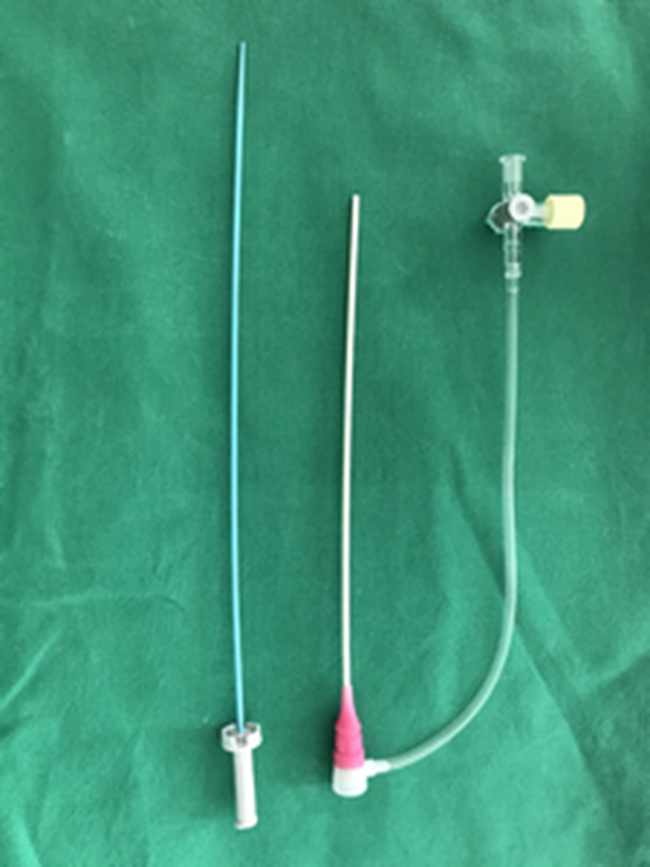
Figure 1. The Glidesheath Slender sheath (Terumo, Tokyo, Japan).
Aim
In this retrospective study, we present evaluation of the clinical safety and efficacy of the Glidesheath Slender for percutaneous interventions in small children with congenital heart diseases.
Methods
Patients
We present a group of 52 patients (male: n = 36; 69%) with a median age of 119 days (min. 3; max. 1302), median weight: 5.3 kg (min. 1.4; max. 14.0), median height: 61 cm (min. 39; max. 102), and median body surface area (BSA) 0.28 m2 (min. 0.12; max. 0.63) in whom percutaneous catheter interventions (n = 55) were performed via a Glidesheath Slender. In 49 (94%) children, the intervention was performed from femoral access (artery n = 35 (71%), vein n = 14 (29%)) in 2 (4%) from the axillary arterial access and in 1 (2%) from the jugular venous access. Five French (n = 44 (85%)) and 6F (n = 8 (15%)) Glidesheath Slender were used in our study group. The type of intervention: stenting of re-Coarctation of Aorta (re-CoA) (n = 11), ductus arteriosus stenting (n = 7), pulmonary arterial interventions (n = 9), and ventricular septal defect (VSD) occlusion (n = 7); other interventions (n = 21): Sano-Shunt stenting (n = 1), Blalock–Taussig (BT)-Shunt stenting (n = 2), Aortopulmonary (AP)-Shunt stenting (n = 1), Foramen ovale stenting (n = 1), right ventricular outflow tract (RVOT) stenting (n = 1), collateral vessels occlusion (n = 4), patient ductus arteriosus (PDA) occlusion (n = 2), Scimitar sequester artery occlusion (n = 1), Ductus arteriosus stent balloon dilatation (n = 2), re-Coarctation of Aorta balloon dilatation (n = 2), re-Coarctation of Aorta stent balloon dilatation (n = 2), balloon dilatation of the stent in the pulmonary venous collector in a patient with total anomalous pulmonary vein return (TAPVR) (n = 1), and Rashkind procedure (n = 1). The 6F Glidesheath Slender sheath was used for left pulmonary artery (LPA) stent implantation (n = 2), re-Coarctation of Aorta stent implantation (n = 2), right pulmonary artery (RPA) stent implantation (n = 1), re-Coarctation of Aorta balloon dilatation (n = 1), patient ductus arteriosus occlusion (n = 1), and Rashkind procedure (n = 1). Detailed patient characteristics are presented in Table 1. Informed consent was obtained from each patient.
Table 1. Detailed patients characteristics

Re-CoA = re-Coarctation of Aorta; VSD = ventricular septal defect.
Procedure
All interventions (n = 55) were performed under general anaesthesia or conscious sedation. In all patients, vessel access was obtained under ultrasound guidance. In each case, the adequate sheath size was chosen based on the attempted procedure and adapted to the BSA of the patient. We always attempted to perform the intervention via the sheath with the smallest possible outer diameter. Heparin (100 IU/kg) was administered in all children just after gaining vascular access.
Hemostasis
Hemostasis after catheterization was achieved with manual compression in all patients. Care was taken to maintain distal limb perfusion (manual compression under peripheral arterial pulse control, inspection of the extremity colouration). After obtaining hemostasis, an elastic, not tight dressing, was left for 24 hours. Peripheral pulse inspection was continued after discharging the patient from the catheterization laboratory to the ward. In patients with arterial access and a body weight less than 10 kg and in all patients in whom peripheral pulses were not palpable or in whom the pulse was only weak after catheterization, a body surface adapted (10,000 IU/m2 KOF/24 h) intravenous constant infusion of high-molecular heparin was applied.
Follow-up
In the follow-up, all patients were routinely scheduled for out-patient controls, and during clinical examinations, peripheral pulses were documented. In patients, in whom the venous access was used, the clinical signs of the vene occlusion were carefully examined after the procedure. Some of the patients in our study group received repeated catheterization in the follow-up. Gaining venous access on the side of previous catheterization was possible.
Results
No serious complications associated with vessel cannulation occurred. Kinking while introducing the Glidesheath Slender was not an issue in our study group. In two patients due to weak peripheral pulses just after catheterization, an intravenous heparin infusion was applied. None of those patients required fibrinolytic therapy, and the peripheral pulse was palpable shortly after introducing heparin therapy in both cases. None of the children presented symptoms of the vessel narrowing or occlusion (median follow-up time: 99 days (min. 1, max. 608)). In all patients in whom the procedure was performed from the arterial access, the pulse on the peripheral arteries (posterior tibial artery or radial artery, respectively) was palpable. No signs of vein occlusion were noticed in patients in whom venous access was used.
Discussion
Our study shows that performing percutaneous interventions in small children with the use of the Glidesheath Slender is safe, feasible, and effective. It enables downsizing of the outer sheath diameter by one French, which is significant in this patient group. Therefore, with this approach, it is possible to extend percutaneous treatment possibilities.
The vessel diameter comprises a significant limitation for catheter interventions in small children with congenital heart disease. Large sheaths, which are required for implantation of some devices (stent, occluder) or balloons, proved to be, among others, a risk factor for vascular complications.Reference Vitiello, McCrindle, Nykanen, Freedom and Benson1 Although the range of various interventions performed via Glidesheath Slender among patients from our study group is very heterogeneous, no vascular complications were recorded in any patient.
In the past, when only the large size (8F or 9F) angioplasty catheters were available, the ileofemoral arterial complications rate in small children was very high.Reference Burrows, Benson and Williams2,Reference Burrows, Benson, Babyn and MacDonald4 Injury or occlusion of the access vessel is one of the possible complications after percutaneous interventions in paediatric patients. Among our patients, treatment of re-coarctation of the aorta was the most common procedure. Especially for these patients, the potential need for stent re-expansion limits the use of stent implantation,Reference Feltes, Bacha and Beekman5 because a larger sheath is needed for stents that can address the demands of a growing vessel. The Slender sheath offers the possibility to use an arterial 5F sheath even in patients with a median weight of 5.3 kg with less danger of vessel damage after the procedure.
For percutaneous ventricular septal defect occlusion, a weight of less than 5 kg was significantly correlated with procedure-related complications.Reference Holzer, Balzer and Cao6 Using the Slender sheath allows the introduction of a 6F guiding catheter into an arterial system in small children with an outer diameter of a 5F regular sheath, with the possibility to introduce larger devices from a retrograde access, thereby shortening and simplifying the procedure.
Although the venous system generally tolerates larger sheaths, pulmonary arterial interventions can be performed with the Slender sheath in smaller children with less risk of vessel compromise. Although even stents delivered through a 6F coronary guiding catheter may not be dilatable to adult size, they may be very well cracked later in life to achieve adult-sized vessel or valve dimensions.Reference Gendera, Ewert and Tanase7
Arterial duct stenting aims to establish a reliable source of pulmonary blood flow. According to current indications for cardiac catheterisation in paediatric patients,Reference Feltes, Bacha and Beekman5 access vessel injury or obstruction is particularly mentioned as potential risks or complication of the procedure. As the procedure is performed mostly in newborns, the advantages of a smaller sized sheath are obvious.
We are convinced that downsizing the outer sheath French-size to the smallest commercially available values may result in significant decrement of the incidence of vascular complications in miscellaneous interventions like collateral vessel closure or Blalock–Taussig shunt stenting as it was shown in our patient group.
In our study group, an intravenous high-molecular-weight heparin infusion was applied due to weak peripheral pulses just after catheterization only in two patients. None of them required fibrinolytic therapy, which in our centre is initiated in patients in whom intravenous heparin infusion is not effective within the first 4 hours after cardiac catheterization.
The absence of peripheral pulses within the first 3–6 hours after arterial access for cardiac catheterization is a reliable predictor for arterial thrombosis.Reference Hurwitz, Franken, Girod, Smith and Smith8 After this time, the predictive value of peripheral pulse presence in paediatric patients is significantly decreased, due to the high incidence of false negative results due to early collateralization.Reference Flanigan, Keifer, Schuler, Ryan and Castronuovo9 Therefore, repeated pulse control within the first hours after cardiac catheterization was considered as a reliable tool to detect arterial thrombosis.
However, performing percutaneous interventions via Glidesheath Slender may be associated with some procedural limitations. The short length of the sheath does not enable angiography during device implantation (for example, in case of re-Coarctation of Aorta stenting), so reliable landmarks are needed, or a second catheter needs to be placed for angiographic depiction during device deployment. For the same reason, a stent cannot be advanced to the landing zone, protected by the sheath. Hence, it must be possible to deliver the stent in the correct position without stent dislodgement. Although the Glidesheath Slender enables device introduction and implantation, device retrieval may be difficult (snaring of embolised stents and removal through the sheath) due to significantly thinner walls of the sheath and, hence, less mechanical stability at withdrawal of embolised metallic material. Finally, due to the hydrophilic coating, the sheath has the tendency to dislodge during an intervention. We learnt to fix the sheath with strips to avoid this annoying feature.
The initial experience with Glidesheath Slender in adults with radial access is promising.Reference Aminian, Dolatabadi and Lefebvre3 So far, there is only one case report presenting results of Glidesheath Slender in small children.Reference Gendera, Cleuziou and Tanase10 In our experience with a larger cohort of patients, all patients showed vessel patency by clinical means, and hence, the results are very promising.
Limitations
This is a retrospective study without a control group, so one can only assume that the lack of acute vascular complications was due to the use of the Glisesheath Slender.
Conclusion
The Glidesheath Slender effectively reduces the outer sheath diameter by one French. This is a potential advantage for various types of interventions in small children, reducing the risk of vessel complications (stenosis, occlusion). Interventions via Glidesheath Slender in small patients were safe and feasible and extend the transcatheter possibilities for small children with congenital heart diseases.
Acknowledgements
None.
Financial support
This research received no specific grant from any funding agency, commercial or not-for-profit sectors.
Conflicts of interest
None.
Ethical standards
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national guidelines on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008, and has been approved by the institutional committees.




