Turner syndrome is a clinical syndrome of congenital dysplasia caused by an autosomal abnormality. Due to the entire or partial loss of an X chromosome combined with abnormal growth and development and secondary sex characteristics, Turner syndrome is usually associated with congenital cardiovascular malformations. Reference Sachdev, Matura and Sidenko1 Pulmonary varix is a relatively rare type of pulmonary vein abnormality. Reference Batram and Strickland2,Reference Hyun, Do and Lim3 We report a very rare case of an adult with Turner syndrome with multiple types of pulmonary vein malformations. Computer tomography pulmonary angiography, cardiac catheterisation, and selective pulmonary angiography confirmed the presence of anomalous right upper pulmonary venous connection, left upper pulmonary vein obstruction, and varicose vein malformations of the left pulmonary veins. We present the following case in accordance with the CARE reporting checklist.
Case presentation
A 27-year-old woman underwent a plain CT of her chest at the time of a physical examination which revealed that there was an abnormal shadow in her left lung. She had no menstrual history to report and she underwent hysterectomy and bilateral adnexectomy 6 years prior due to the diagnosis of dysgerminoma of the ovary. At the time of admission, her vital signs were stable without symptoms. She was 145 cm tall and 70 kg in weight. Cardiopulmonary examination was unremarkable. Peripheral blood lymphocyte karyotype analysis confirmed a diagnosis of Turner syndrome with a 45,XO karyotype.
Echocardiographic examination revealed bicuspid aortic valve malformation, an anomalous connection of the right upper pulmonary vein with the superior vena cava, and slightly enlargement of the right ventricle (RV, 27 mm). The remaining atrium and ventricle were unremarkable and the left ventricular ejection fraction was 67%. Computer tomography pulmonary angiography was performed and showed a left pulmonary varix (Figs 1 and 2). The three-dimensional reconstruction confirmed the anomalous right upper pulmonary venous connected to the superior vena cava (Fig 2). However, it was difficult to determine the origin and type of this pulmonary vein malformation with CT reconstruction alone. Further cardiac catheterisation was done through the femoral vein. Selective left pulmonary arterial angiography showed a normal arterial phase, but a distorted, haemangioma-like dilated blood vessel in the left upper pulmonary vein drainage area in the venous phase. To further clarify its morphological characteristics and haemodynamic significance, we performed selective angiography through the anomalous pulmonary vein via atrial septal puncture. It showed there was a partial obstruction in the drainage area of the left upper pulmonary vein (Fig 3A), and partial blood returned into the proximal left upper pulmonary vein through this varicose malformed communicating branch (Fig 3B). The final diagnosis of this patient was partial anomalous pulmonary venous connection and pulmonary venous varix coexist with Turner syndrome. But according to cardiac catheterisation, there was no pulmonary hypertension and the calculated Qp:Qs was 1.26:1. So the patient was discharged without further surgical treatment. In our case, there were no complications during the procedure. On the latest follow-up, the patient was clinically stable without new symptoms.

Figure 1. Computer tomography pulmonary angiography showing a left pulmonary varix (white arrow).

Figure 2. The three-dimensional reconstruction of the computer tomography pulmonary angiography. It showed an anomalous right upper pulmonary venous connected to the superior vena cava (white arrow), and a twisted, haemangioma-like expansion of the communicating branch of the pulmonary vein that was connected to the proximal upper left pulmonary vein (yellow arrow).
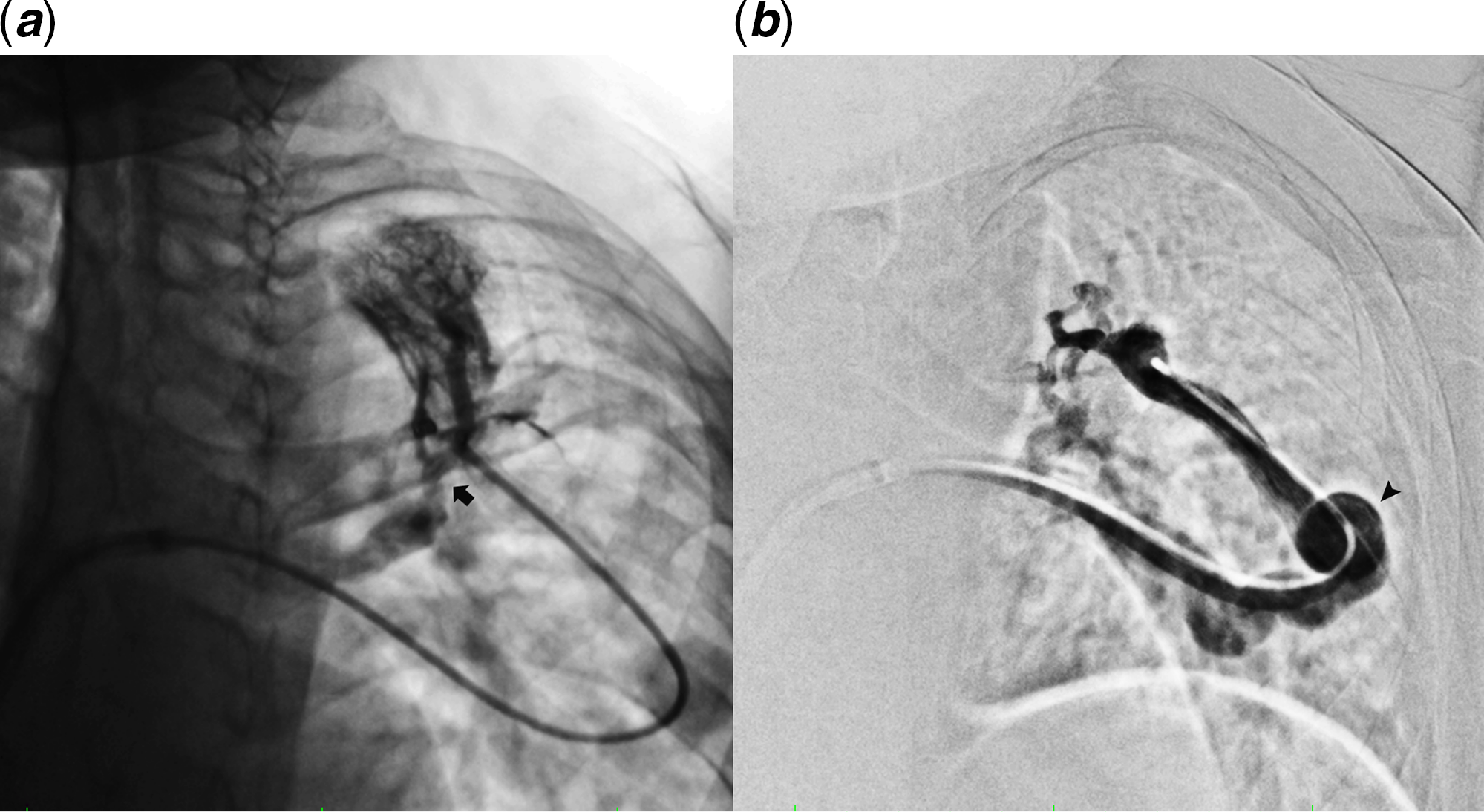
Figure 3. Selective pulmonary angiography findings. (A) Partial obstruction in the drainage area of the left upper pulmonary vein (black arrow). (B) Partial blood returned through the varicose malformed communicating branch (black arrow) of the pulmonary vein into the proximal left upper pulmonary vein and then returned to the left atrium.
The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient.
Discussion
Turner syndrome is a type of autosomal abnormality that affects women, with an incidence of approximately 1:2000. Its main clinical features include short stature, delayed puberty, and congenital cardiovascular malformations. Reference Dobrowolski, Klisiewicz and Michalowska4,Reference Silberbach, Roos-Hesselink and Andersen5 The common cardiovascular malformations in these patients include bicuspid aortic valve malformations, aortic contractions, and aortic dissections. Reference Sachdev, Matura and Sidenko1 The anomalous pulmonary venous connection accounted for only 2.9% of cardiovascular malformations in Turner syndrome. Reference Mazzanti and Cacciari6 This patient had the typical manifestations of Turner syndrome such as a short stature and no menses. She had bicuspid aortic valve malformations that are common in Turner syndrome, but these were accompanied by multiple types of pulmonary vein malformations, which were rare.
Pulmonary vein abnormalities can be divided into two categories, namely, structural abnormalities with normal drainage and combined structural and drainage abnormalities. The former includes pulmonary varicose veins, but because there is no right-to-left or left-to-right shunt, these abnormalities can be asymptomatic. Reference Hyun, Do and Lim3 The latter can cause cardiovascular damage due to a right-to-left shunt. This type of malformation is most commonly diagnosed by chest imaging examination. Further selective pulmonary angiography is very important when there is difficulty in distinguishing anomalous unilateral single pulmonary vein, pulmonary arteriovenous malformation, pulmonary vein atresia, and pulmonary vein stenosis. Reference Engelke, Brown and Sabharwal7 In this case, echocardiography, computer tomography pulmonary angiography, cardiac catheterisation, and selective pulmonary angiography via atrial septal puncture confirmed the presence of both types of pulmonary vein abnormalities and ruled out arteriovenous malformation. The structural and morphological characteristics of the left pulmonary varicose veins of this patient fully met the conditions for the diagnosis of pulmonary varicose veins reported by Bartram. Reference Batram and Strickland2
Possible causes of pulmonary vein abnormalities may be congenital and acquired. Partial anomalous pulmonary venous connection is a congenital abnormality in most cases. In this case, the anomalous right upper pulmonary venous connection to the superior vena cava was most likely due to congenital dysplasia and may be related to Turner syndrome. Pulmonary vein stenosis can be very rarely occurs secondary to the formation of communicating branches of the pulmonary vein with pulmonary varices. Reference Tajiri, Koizumi and Hara8 This patient had no history of cardiopulmonary surgery or trauma. Therefore, her malformation of upper left pulmonary vein was considered to be due to congenital abnormalities. Since a similar case has rarely been reported, Reference Maillard, Cottin and Etienne-Mastroianni9,Reference Nasser, Revel and Thibault10 it is not clear whether these findings were related to Turner syndrome. And also in this patient, we innovatively performed an atrial septal puncture and performed a proposed angiogram of the malformed pulmonary veins through a catheter to further confirm the characteristics of the pulmonary venous varices, and according to the imaging characteristics of the left upper pulmonary vein in this patient, the formation of pulmonary varices was considered to be due to local obstruction of pulmonary venous return and the formation of traffic branch circulation.
The need for further invasive treatment of pulmonary venous abnormalities depends on the type of malformation and associated complications and risks. Reference Hyun, Do and Lim3,Reference Tajiri, Koizumi and Hara8 Surgical correction is needed in patients with partial anomalous pulmonary venous connection if this abnormality is associated with a right-to-left shunt causing hypoxemia and related symptoms. Reference Hyun, Do and Lim3 Few studies have reported that the complications of pulmonary varices include symptoms and complications. Reference Perret and Fortelius11 In this case, the patient had no related symptoms. Cardiac catheterisation showed the left-to-right shunt was small. The blood flow in the varicose, twisted, haemangioma-like expanded communicating branch of the pulmonary vein was fast without signs of thrombus. The communicating branch of the upper left pulmonary vein was considered a returning path for blood flow. Therefore, no further intervention or surgery was performed. Eventually, we chose to discharge the patient from the hospital for follow-up and observation.
Conclusion
In conclusion, we have diagnosed and evaluated a very rare case of Turner syndrome with multiple types of pulmonary vein malformations. In the course of diagnosis, echocardiography and computer tomography pulmonary angiography are very important for screening patients with pulmonary vein malformations, and cardiac catheterisation and selective pulmonary angiography can further confirm the diagnosis, morphological characteristics, and haemodynamic significance and provide a reference for the next step of treatment.
Financial support
None.
Conflicts of interest
All authors have completed the ICMJE uniform disclosure form. The authors have no conflicts of interest to declare.
Ethical standards
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. This article does not contain any studies with animals performed by any of the authors. Informed consent was obtained from all individual participants included in the study.






