Introduction
The November, 2020 issue of Cardiology in the Young contains the inaugural five manuscripts from the Cardiac Neurodevelopmental Outcome Collaborative Reference Sood, Jacobs and Marino1–Reference Ilardi, Sanz, Cassidy, Sananes, Rollins, Ullman Shade, Carroll and Bellinger5 marking the beginning of the partnership between the Cardiac Neurodevelopmental Outcome Collaborative and Cardiology in the Young. In this issue of Cardiology in the Young, this article is part of the first set of three papers from the Cardiac Neurodevelopmental Outcome Collaborative R13 grant funded by the National Heart, Lung, and Blood Institute of the National Institutes of Health of the United States of America, which defines the research agenda for the next decade across seven domains of cardiac neurodevelopmental and psychosocial outcomes research Reference Sood, Jacobs and Marino6–Reference Cassidy, Butler, Briend, Calderon, Casey, Crosby, Fogel, Gauthier, Raimondi, Marino, Sood and Butcher8 :
Neurodevelopmental and psychological difficulties affect more than half the population of individuals with complex forms of CHD. Reference Mussatto, Hoffmann and Hoffman9–Reference Wernovsky and Licht12 Efforts over the past decade to identify modifiable factors that influence the neurodevelopmental and psychological sequelae of CHD have focused predominantly on surgical and perioperative variables; Reference Wernovsky and Licht12 however, individuals with CHD spend most of their developing years out of the hospital with their parents, caregivers, and other broader family and social networks. Parent mental health, parenting behaviours, and the family environment are known to exert a powerful influence on child neurodevelopment, behavior, and emotional well-being Reference Ramchandani, Stein, O’Connor, Heron, Murray and Evans13,14 and can exacerbate or mitigate the effects of medical experiences on child outcomes. Reference Bakula, Sharkey and Perez15
Given the demands of parenting a child with CHD and repeated exposure to potentially traumatic medical events, Reference Wray, Brown and Tregay16–Reference Gregory, Prouhet, Russell and Pfannenstiel18 it is not surprising that parent mental health can be substantially affected. CHD diagnosis and treatment often occur (or at least begin) during the prenatal and early postnatal periods, a time when mothers and fathers are at heightened risk for mental health difficulties, Reference Ramchandani, Stein, O’Connor, Heron, Murray and Evans13,Reference McDonald, Sherman and Kasparian19–Reference Kasparian21 and when the bond between infant and parent is in the formative stages of development. Reference Perry, Blair and Sullivan22 A systematic review of mental health symptoms in parents of children with CHD found that over 80% of parents report clinically significant symptoms of post-traumatic stress, 30–80% report severe psychological distress, and 25–50% report depression and/or anxiety. Reference Woolf-King, Anger, Arnold, Weiss and Teitel23 These rates of mental health symptoms far exceed what is reported in the general population and are similar to other trauma-exposed populations, including the military. Reference Richardson, Frueh and Acierno24 Fewer studies have focused on fathers specifically, but those that have suggest fathers may experience the stress of CHD differently from mothers and exhibit different mental health symptoms. Reference Gregory, Prouhet, Russell and Pfannenstiel18,Reference Sood, Karpyn and Demianczyk25,Reference Hoffman, Karpyn, Christofferson, Neely, McWhorter, Demianczyk, James, Hafer, Kazak and Sood26 A growing literature suggests that parent education level, household income, family structure, country of birth, and language may also influence parent mental health following diagnosis of CHD. Reference Lisanti27,Reference Franck, Mcquillan, Wray, Grocott and Goldman28 Elevated parent distress within and beyond the perinatal period is associated with an increased risk of emotional and behavioural difficulties and poorer health-related quality of life in children with CHD. Reference DeMaso, Labella and Taylor29–Reference McCusker, Armstrong, Mullen, Doherty and Casey33 Moreover, parent mental health is often a stronger predictor of child developmental outcomes than medical variables, including CHD severity and surgical factors. Reference DeMaso, Labella and Taylor29,Reference McCusker, Armstrong, Mullen, Doherty and Casey33 Psychosocial adaptation in the parents may reduce the risk for parent mental health difficulties and promote positive child neurodevelopmental and psychosocial outcomes.
Family functioning encompasses many facets of the family environment including relationships amongst family members, parent–child attachment, and levels of conflict, cohesion, adaptation, communication quality, and organisation. Reference Alderfer, Fiese and Gold34,Reference Lewandowski, Palermo, Stinson, Handley and Chambers35 CHD has been shown to influence family relationships, including parent–child, marital/partner, sibling, and extended family relationships, as well as parenting style/practices. Reference Gregory, Prouhet, Russell and Pfannenstiel18,Reference Sood, Karpyn and Demianczyk25,Reference Berant, Mikulincer and Florian36,Reference Dale, Solberg, Holmstrøm, Landolt, Eskedal and Vollrath37 While many families report increased family conflict, decreased communication, feelings of isolation, and difficulties with parent–infant bonding following a diagnosis of CHD, others report greater family cohesion and support. Reference Gregory, Prouhet, Russell and Pfannenstiel18,Reference Sood, Karpyn and Demianczyk25,Reference Jordan, Franich-Ray and Albert38 The financial burden of CHD and disruptions to employment and family routine associated with long hospital stays and frequent medical appointments likely influence family adaptation following CHD diagnosis as well. Reference Elhoff, McHugh, Buckley, Morris, Simpson and Scheurer39,Reference Connor, Kline, Mott, Harris and Jenkins40
Recognition of the need to proactively support parent mental health and family functioning to reduce suffering, promote psychosocial adaptation, and improve child neurodevelopmental and psychosocial outcomes has increased substantially over recent years. Reference Utens, Callus, Levert, Groote and Casey41–Reference Kasparian, Kan, Sood, Wray, Pincus and Newburger44 Published research does not, however, provide the necessary evidence to determine the type, timing, or delivery mode of interventions most likely to improve parent mental health and family functioning. Additionally, prior research has rarely focused on identifying which difficulties are of greatest concern to parent stakeholders or exert the strongest influence on child and family outcomes and are, therefore, of highest priority for intervention. Reference Tesson, Butow, Sholler, Sharpe, Kovacs and Kasparian45,Reference Gramszlo, Karpyn and Demianczyk46 Significant gaps in knowledge remain, and parents and families continue to report critical unmet psychosocial needs. Reference Gramszlo, Karpyn and Demianczyk46
The Parent Mental Health and Family Functioning Working Group of the Cardiac Neurodevelopmental Outcome Collaborative is comprised of multidisciplinary topic area experts (in psychology, cardiology, nursing, social work) from three continents (North America, Europe, Australia), a health disparities expert, and parent stakeholders (Table 1). This working group is one of the seven formed by the Cardiac Neurodevelopmental Outcome Collaborative in 2018 to identify significant gaps in knowledge and critical questions that must be answered to advance neurodevelopmental care and outcomes. The effort was supported by a National Heart, Lung, and Blood Institute R13 grant awarded to the Cardiac Neurodevelopmental Outcome Collaborative in collaboration with the Ann & Robert H. Lurie Children’s Hospital of Chicago, which funded a 2-day meeting of multidisciplinary, multinational experts, and patient/caregiver stakeholders in Kansas City, Missouri. The specific goals of the Parent Mental Health and Family Functioning Working Group were to identify: (1) significant knowledge gaps related to parent mental health and family functioning within the context of CHD; (2) critical questions that must be answered to further knowledge, policy, care, and outcomes; and (3) investigations needed to answer these critical questions. Although parents and families of children with complex forms of CHD requiring cardiac surgery during infancy were the primary focus of the working group, recommendations may also apply to parents/families of children with milder forms of CHD, as objective illness severity does not consistently predict mental health outcomes. Reference Franck, Mcquillan, Wray, Grocott and Goldman28,Reference DeMaso, Campis, Wypij, Bertram, Lipshitz and Freed47 The term “parent” in this context broadly refers to all primary caregivers including biological and adoptive and long-term foster parents, and other adults serving in a primary caregiving role. The term “family” includes both nuclear and extended family members. This paper presents the top five critical questions identified by the working group (Table 2) and provides specific recommendations for science and health policy to inform the next decade of research on parent mental health and family functioning in CHD.
Table 1. Parent Mental Health and Family Functioning Working Group Participants
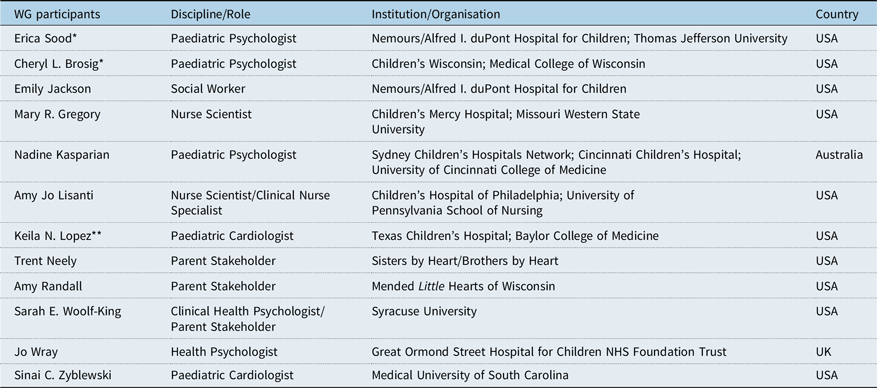
WG = Working Group. *Working Group Co-Lead. **Health Disparities Expert.
Table 2. Parent mental health and family functioning: critical questions, significant gaps in knowledge, and investigations needed
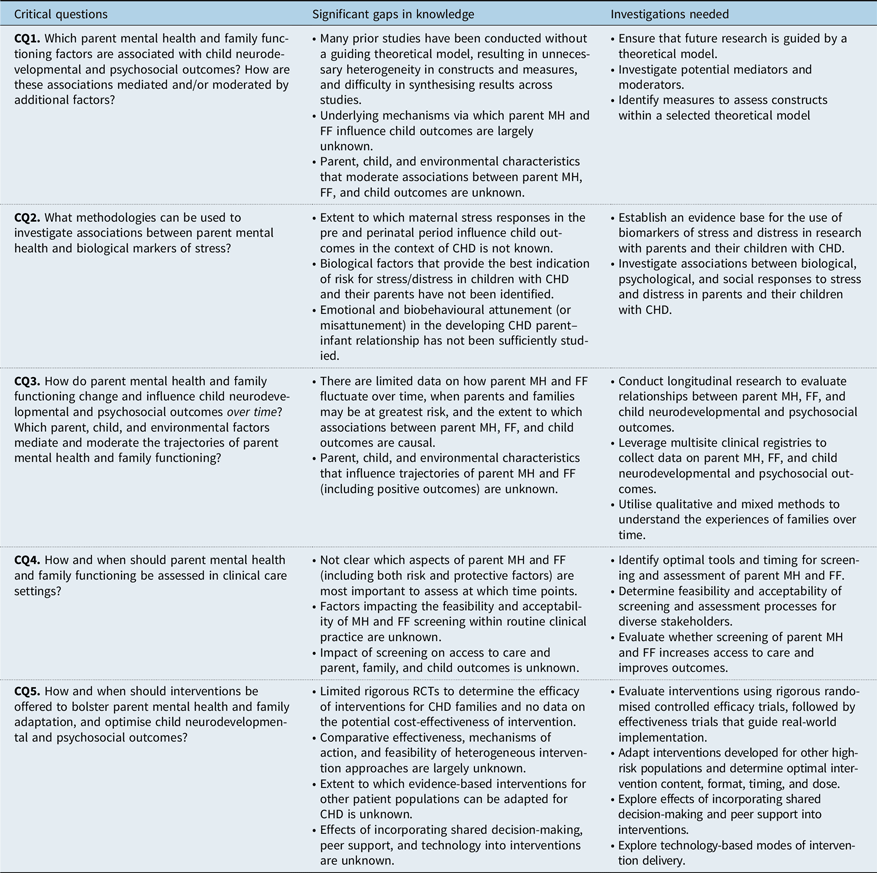
CHD = congenital heart disease; CQ = Critical Question; FF = family functioning; MH = mental health; RCT = randomised controlled trial.
Critical Question 1: Which parent mental health and family functioning factors are associated with child neurodevelopmental and psychosocial outcomes? How are these associations mediated and/or moderated by additional factors?
Existing knowledge
A growing body of research indicates that parent mental health symptoms are associated with poorer outcomes for children with CHD. Parent post-traumatic stress, referring to specific psychological and physiological symptoms (e.g., flashbacks, avoidance, hyperarousal) following exposure to a traumatic event (e.g., witnessing their child go into cardiac arrest), is associated with lower psychosocial functioning Reference DeMaso, Labella and Taylor29 and quality of life Reference Ernst, Marino and Cassedy30 for children and adolescents with CHD. Parenting stress, which refers to the magnitude of stress in the parent–child system, is associated with greater emotional and behavioural problems in children Reference Visconti, Saudino, Rappaport, Newburger and Bellinger32,Reference DeMaso, Campis, Wypij, Bertram, Lipshitz and Freed47,Reference Goldberg, Janus, Washington, Simmons, MacLusky and Fowler48 and lower psychosocial functioning in adolescents with CHD. Reference DeMaso, Labella and Taylor29 Parent mental health symptoms are stronger predictors of child psychosocial functioning than medical or surgical factors, Reference DeMaso, Labella and Taylor29,Reference McCusker, Armstrong, Mullen, Doherty and Casey33 and parent mental health can influence parent report of child health-related quality of life. Reference Denniss, Sholler, Costa, Winlaw and Kasparian31,Reference Marshall, d’Udekem and Sholler49 There is also preliminary evidence that untreated mental health symptoms may influence mother–child interactions (e.g., lower maternal responsivity, lower child positive interactivity) and increase the risk for child developmental delay, Reference Laing, McMahon, Ungerer, Taylor, Badawi and Spence50 consistent with the broader literature on maternal mental health in non-CHD populations Reference Kingston and Tough51–Reference Cook, Ayers and Horsch53 and highlighting the need for interventions targeting parent mental health symptoms.
Significant gaps in knowledge
While there is growing evidence that parent mental health and aspects of the parent–child relationship influence the outcomes of children with CHD, available studies have examined a range of parent mental health and family functioning factors using a variety of measures, often in the absence of a theoretical model to guide the selection of constructs and measures. Although a few researchers have proposed theoretical models for families of children with CHD that could guide the selection of constructs and measures, Reference Lisanti27,Reference Mussatto54–Reference Lisanti, Golfenshtein and Medoff-Cooper56 most studies do not select constructs or measures based on an underlying theoretical model. Post-traumatic stress symptoms, parenting stress, anxiety, and depression are distinct clinical problems that may influence child outcomes through different mechanisms (e.g., overprotective versus disengaged parenting; emotionally over-involved versus hostile family environment), 14,Reference Clarke, Cooper and Creswell57,Reference Christie, Hamilton-Giachritsis, Alves-Costa, Tomlinson and Halligan58 but more work is needed to understand these underlying mechanisms in families affected by CHD. Parent, child, and environmental characteristics, such as sex, race, ethnicity, socioeconomic status, language barriers, physical health, stigma, discrimination, social networks, and parental vulnerability, are likely to moderate associations between parent mental health and child outcomes, Reference Lisanti27 but these associations have not been adequately studied in families affected by CHD. Without the use of a theoretical model to guide hypothesis generation, research design, and outcomes measurement, the literature on parent mental and family functioning are unnecessarily heterogeneous, study findings are difficult to synthesise, and it is unclear which parent mental health or family factors are best to target in intervention design and clinical care. Reference Woolf-King, Anger, Arnold, Weiss and Teitel23,Reference Kasparian, Kan, Sood, Wray, Pincus and Newburger44,Reference Tesson, Butow, Sholler, Sharpe, Kovacs and Kasparian45
Investigations needed
-
(1) Ensure that future research is guided by a theoretical model.
Studies of parent mental health and family functioning should have a clear rationale for the selection of constructs based on a guiding theoretical model. Numerous existing models provide conceptual foundations for the influence of parent mental health, family functioning, and/or parenting on child outcomes (e.g., Double ABCX model, self-efficacy theory, parenting stress model, control theory, attachment theory). Reference McCubbin and Patterson59–Reference Goodman and Gotlib64 Investigators have adapted and tested these models with high-risk families, including families of children with disabilities, Reference McCubbin and Patterson59,Reference Saloviita, Italinna and Leinonen65–Reference Raina67 families of infants in the neonatal ICU, Reference Melnyk, Crean, Feinstein and Fairbanks68,Reference Lee, Garfield and Kim69 families impacted by other paediatric illnesses or developmental disorders, Reference Pakenham, Samios and Sofronoff70,Reference Hocking and Lochman71 and families exposed to trauma. Reference Scheeringa and Zeanah72,Reference Creech and Misca73 Researchers have also developed or adapted theoretical models specifically for families of children with CHD including the Family Adaptation to Child Chronic Illness Model, Reference Mussatto54 Parental Satisfaction and Wellness Model, Reference Lawoko55 Paediatric Cardiac ICU Parental Stress Model, Reference Lisanti, Golfenshtein and Medoff-Cooper56 and Parental Stress and Resilience Model for CHD. Reference Lisanti27 The latter is the only published model to provide a conceptual foundation for how parent mental health following CHD diagnosis influences child outcomes and includes environmental factors (e.g., neighbourhood, access to care) that may contribute to health disparities. The process of model selection for a particular study should be directly informed by study objectives and should include patient and parent involvement to ensure the model and included constructs are perceived as meaningful and relevant to those with lived experience. Reference Goodman and Sanders Thompson74 As studies incorporate theory-driven methodology, theoretical models can be adapted based on empirical evidence and ultimately validated for families of children with CHD.
-
(2) Investigate potential mediators and moderators.
Future research should directly examine potential mechanisms by which parent mental health and family functioning influence outcomes for children with CHD, including attachment, co-regulation of the physiological stress response, parent–child interaction, parenting style, and family environment. Research should also include parent, child, and environmental characteristics that may moderate associations amongst parent mental health, family functioning, and child outcomes, such as sex, race, ethnicity, cultural factors, socioeconomic status, language, physical health, discrimination, and social networks. Identification of mediators and moderators will inform theory development and adaptation, help to identify targets for intervention, and enhance our understanding of intervention effects. Reference Gómez, Schalock and Verdugo75
-
(3) Identify measures to assess constructs within a selected theoretical model.
Measures to assess constructs within a selected theoretical model should be identified and utilised consistently in research. Investigators have conducted systematic reviews summarising the psychometric properties of a wide range of measures (e.g., adult mental health, parent–child attachment and interaction, child social–emotional and behavioural outcomes) with expectant parents, families of young children, and families impacted by other chronic illnesses, Reference Gridley, Blower, Dunn, Bywater and Bryant76–Reference Hodes, Insel and Landis80 which can guide the selection of measures for families affected by CHD. Some measures may require psychometric adaptation and validation for use with families affected by CHD, such as those designed to capture responses to a specific experience or environment. For example, the Parental Stressor Scale: Neonatal ICU was adapted to measure stress resulting specifically from infant hospitalisation, Reference Miles, Funk and Parental Stressor Scale81 and the resulting measure (Parental Stressor Scale: Infant Hospitalisation) was psychometrically evaluated with the parents of medically fragile, hospitalised infants. Reference Miles and Brunssen82 Similar processes have been conducted with measures of post-traumatic stress symptoms resulting from specific types of trauma. Reference Weathers, Litz, Huska and Keane83 Parent and patient perspectives should be incorporated into the selection and/or adaptation of measures to ensure that they are clinically meaningful and acceptable to stakeholders. Reference Reader, Ruppe and Deatrick84 Measures should also be linguistically and culturally appropriate and accessible for diverse families (e.g., available in multiple languages, literacy levels, and modalities).
Critical Question 2: What methodologies can be used to investigate associations between parent mental health and biological markers of stress?
Existing knowledge
Exposure to stress elicits a cascade of physiological responses. The hypothalamic–pituitary–adrenal axis, for example, is particularly responsive to psychosocial stress, with dynamic interaction between the brain, autonomic nervous system, endocrine and immune systems, and the gut microbiome. Reference Corwin and Ferranti85 Persistent high levels of psychosocial stress can result in a state of allostatic load; a physiological accumulation of the effects of stress that may contribute to a range of adverse health outcomes, including cardiovascular disease, neurocognitive decline, mental illness, and mortality. Reference Corwin and Ferranti85–Reference Carazo, Kolodziej and DeWitt90
Up to 80% of parents of children with complex CHD report high levels of psychological stress and distress, Reference Woolf-King, Anger, Arnold, Weiss and Teitel23 potentially increasing the risk of developing allostatic load and its consequences. Reference Kasparian21,Reference Lisanti27 Biomarkers of HPA axis functioning (e.g., cortisol) can be measured by analysis of saliva, hair, skin, nail, stool, or blood samples, and have been used in studies investigating a range of psychological outcomes, including symptoms of stress, anxiety, and depression in children and adults. Reference El-Farhan, Rees and Evans91–Reference Iliadis, Comasco and Sylvén95 In CHD, preliminary research has found that prenatal exposure to maternal stress and anxiety is associated with differences in foetal brain growth, including smaller hippocampal and cerebellar volumes. Reference Wu, Kapse and Jacobs96
Significant gaps in knowledge
There is a dearth of data on biomarkers of parental psychological stress in CHD. The extent to which high levels of maternal prenatal and postnatal psychological stress may influence health outcomes for mothers and their children with CHD is an area of growing interest. Reference Kasparian21 In other populations, maternal biological stress responses, such as HPA axis functioning in the perinatal period, have been shown to influence offspring health outcomes across the lifespan, including the risk of neurodevelopmental delay, and emotional and behavioural disorders, such as anxiety, depression, and attention deficit hyperactivity disorder. Reference Butler and Randall97–Reference Gilles, Otto and Wolf101 There is, however, limited psychobiological research directly investigating these associations in the context of CHD and it is unclear which biomarkers, if any, may provide meaningful and reliable indications of future health risk. Reference Kasparian21
In addition to elucidating the effects of stress on individual health outcomes, this line of inquiry may also expand our understanding of the developing infant-parent relationship, particularly in terms of emotion regulation and biobehavioural attunement in the context of serious childhood illness. Reference Butler and Randall102 Oxytocin, for example, has been widely studied as a biomarker of emotional co-regulation in parent–child dyads without CHD and has been associated with child developmental disorders such as autism spectrum disorder. Reference Feldman, Golan, Hirschler-Guttenberg, Ostfeld-Etzion and Zagoory-Sharon103,Reference Feldman, Gordon and Zagoory-Sharon104 Higher maternal oxytocin levels have also been linked to more affectionate parenting behaviours, lower blood pressure, and lower stress; however, the role of oxytocin in the context of parent–child bonding and attachment, and the accuracy of measurements in mothers of infants with CHD, have yet to be determined. Reference Lisanti, Demianczyk and Costarino105 Interest in the potential role of the microbiome is also growing, but to our knowledge, no published studies have examined the link between parental psychological stress and the developing infant gut microbiome in CHD, though studies are underway and may potentially provide strategies to augment existing therapies, such as the use of probiotics. Reference Rogers, Keating, Young, Wong, Licinio and Wesselingh106,Reference Kan, Cowan, Ooi and Kasparian107
Investigations needed
-
(1) Establish an evidence base for the use of stress biomarkers in research with parents and their children with CHD.
While the association between maternal biomarkers of psychological stress and child neurodevelopment and mental health has been investigated in other populations, an evidence base in CHD has yet to be established. Factors such as cost, participant burden, scepticism about clinical usefulness, and limited expertise in the field contribute to slow progress. Studying the interplay between psychological responses and physiological processes in CHD may provide a more comprehensive understanding of the mediators and moderators of parent and child mental health outcomes, and support the design and implementation of timely, tailored interventions. Reference Kasparian21
-
(2) Investigate associations between biological, psychological, and social responses to stress and distress in parents and their children with CHD.
Aligned with the National Institutes of Health Symptom Science Model, Reference Cashion and Grady108 a comprehensive understanding of the underlying biological processes associated with psychological stress may yield improved diagnostic tools, prevention and intervention opportunities, and treatment approaches. To maximise impact, this work should also explore the potential differential effects of acute versus chronic stress (or allostatic load), and the existence of particularly “sensitive” periods when stress may have the strongest influence on health outcomes (e.g., during foetal development and early infancy). Reference Juster, McEwen and Lupien89 It is well established that exposure of an individual to a stressor elicits a physiologic stress response, and studies in mental health are revealing associations of stress biomarkers with mental health symptoms and diagnoses. For example, recent pilot studies suggest salivary cortisol and heart rate variability may serve as non-invasive biomarkers of stress in infants with CHD and their mothers. Reference Lisanti, Demianczyk and Costarino105,Reference Lisanti, Demianczyk and Costarino109–Reference Harrison, Chen and Stein111 Larger investigations of the associations of stress biomarkers with mental health symptoms within the context of CHD is an important next step.
Critical Question 3: How do parent mental health and family functioning change and influence child neurodevelopmental and psychosocial outcomes over time? Which parent, child, and environmental factors mediate and moderate the trajectories of parent mental health and family functioning?
Existing knowledge
The small number of studies examining parent mental health across multiple time points after CHD diagnosis suggest psychological symptoms and physical manifestations change over time Reference Solberg, Dale, Holmstrøm, Eskedal, Landolt and Vollrath112–Reference Brosig, Whitstone, Frommelt, Frisbee and Leuthner115 and predict future child neurodevelopmental and psychosocial outcomes. Reference DeMaso, Labella and Taylor29,Reference Visconti, Saudino, Rappaport, Newburger and Bellinger32,Reference Goldberg, Janus, Washington, Simmons, MacLusky and Fowler48 Studies have not longitudinally studied family functioning in CHD samples, but research with other patient populations suggests that changes in parental roles and responsibilities, in the quality and/or status of the relationship between parents, financial strain, and child medical care needs may influence family functioning. Reference Streisand, Kazak and Tercyak116,Reference Cousino and Hazen117 Qualitative and survey-based research with parents of children with CHD has identified unique stressors specific to different phases of care (e.g., alterations in parental role within the ICU; difficulties with feeding and weight gain after hospital discharge; balancing protection with independence during the transition to school; navigating neurodevelopmental and learning challenges during school age; redefining the parental role during transition to adult care), and these may correlate with fluctuations in parent mental health, parenting behaviours, and family functioning. Reference Wray, Brown and Tregay16,Reference Sood, Karpyn and Demianczyk25,Reference Lisanti, Allen, Kelly and Medoff-Cooper118–Reference Kaugars, Shields and Brosig123 However, not all parents and families exhibit long-term problems. Reference Wray, Cassedy, Ernst, Franklin, Brown and Marino124 Preliminary research has begun to identify protective parent, child, and environmental resilience factors that moderate parent mental health effects and promote psychosocial adaptation and quality of life. Reference Gregory, Prouhet, Russell and Pfannenstiel18,Reference Lisanti27,Reference Ernst, Marino and Cassedy30,Reference Kaugars, Shields and Brosig123,Reference Wray, Cassedy, Ernst, Franklin, Brown and Marino124 In general, research indicates that parent perceptions of child illness, coping strategies, perceived social support, and socioeconomic status are stronger predictors of parent mental health outcomes than objective illness characteristics. Reference Visconti, Saudino, Rappaport, Newburger and Bellinger32,Reference Doherty, McCusker and Molloy125,Reference Davis, Brown, Bakeman and Campbell126
Significant gaps in knowledge
Investigators have predominantly assessed parent mental health and family functioning following diagnosis of CHD through cross-sectional studies and there remains much to be learned regarding how experiences fluctuate over time, when parents and families may be at greatest risk, and to what extent the associations between parent mental health and child outcomes are causal. Given that CHD is a lifelong condition, a snapshot of parent mental health and family functioning at one point in time (e.g., pregnancy) and in one setting (e.g., intensive care) may not accurately represent a family’s holistic experience over time, nor the full range of outcomes for a child. While cross-sectional studies have begun to identify parent, child, and environmental factors that may moderate parent mental health and quality of life outcomes, Reference Gregory, Prouhet, Russell and Pfannenstiel18,Reference Lisanti27 how they interact synergistically and their relative weights are still not entirely understood. Additionally, very few studies have examined protective factors or psychosocial adaptation over time in families affected by CHD. Reference Li, Cao, Cao, Wang and Cui127
Investigations needed
-
(1) Conduct longitudinal research to evaluate relationships between parent mental health, family functioning, and child neurodevelopmental and psychosocial outcomes.
To better inform intervention, we recommend assessment of parent mental health, family functioning, and child neurodevelopmental and psychosocial outcomes over time within longitudinal cohort studies. Measures of parent mental health and family functioning should be included as early as the prenatal/postnatal periods and throughout childhood and adolescence. Inclusion of standardised measures assessing early effects will yield immediate clinical value and also provide longitudinal data for understanding lifespan trajectories. Cohort studies should include diverse and representative samples (including fathers, families with a lower socioeconomic status or non-traditional family structures, diverse racial and ethnic populations, rural populations) across multiple regions to ensure generalisability of results to diverse populations and identification of sociodemographic moderators that influence trajectories of parent mental health and family functioning. Reference Sorlie and Wei128
-
(2) Leverage multisite clinical registries to collect data on parent mental health, family functioning, and child neurodevelopmental and psychosocial outcomes.
Given the extensive resources required to conduct longitudinal cohort studies and the value of secondary data collected as part of routine care, Reference Forrest, Margolis and Bailey129–Reference Schilling, Dalziel and Nunn132 we recommend that multisite clinical registries be leveraged whenever possible to collect data on parent mental health, family functioning, and child neurodevelopmental and psychosocial outcomes. An increasing number of paediatric cardiac centres provide neurodevelopmental and psychosocial assessments as part of routine care for children with CHD and their families, Reference Miller, Sadhwani, Sanz, Sood, Ilardi, Newburger, Goldberg, Wypij, Gaynor and Marino3,Reference Kasparian, Winlaw and Sholler42 and clinical registries in North America, Europe, Australia, and New Zealand have recently been developed or expanded to include these data. Reference Marino, Sood, Cassidy, Miller, Sanz, Bellinger, Newburger and Goldberg2,Reference Strange, Stewart and Farthing130,Reference Celermajer, Strange and Cordina131,Reference Schilling, Dalziel and Nunn132–Reference Anderson, Brown and Lihn134 As an example, the Cardiac Neurodevelopmental Outcome Collaborative clinical registry launched in 2019 as a module of the Pediatric Cardiac Critical Care Consortium and Pediatric Acute Care Cardiology Collaborative registries and may serve as a valuable resource for researchers interested in studying parent mental health and family functioning in relation to child neurodevelopmental and psychosocial outcomes over time. Reference Marino, Sood, Cassidy, Miller, Sanz, Bellinger, Newburger and Goldberg2 However, disparities in access to neurodevelopmental and psychosocial services must be addressed to ensure equitable healthcare and diverse samples. Reference Loccoh, Yu, Donohue and Lowery135,Reference Gonzalez, Kimbro and Cutitta136
-
(3) Utilise qualitative and mixed methods to understand the experiences of families over time.
Qualitative and mixed methods (i.e., integrating quantitative and qualitative) are recommended to obtain a comprehensive understanding of parent and family lived experiences over time, as well as the range of responses elicited by stress, life events, transitions in care, or discrimination. Reference Alderfer and Sood137 These approaches may be particularly helpful for better understanding the experiences of groups previously under-represented in research (e.g., fathers, families with a lower socioeconomic status, diverse racial and ethnic populations, LGBTQ communities, rural populations), and may also further our knowledge of understudied constructs and outcomes, such as which family functioning factors are likely to be protective, or how parents define and experience resilience, post-traumatic growth, and psychosocial adaptation.
Critical Question 4: How and when should parent mental health and family functioning be assessed in clinical care settings?
Existing knowledge
The need for routine assessment of parent mental health and family functioning to identify at-risk families who may benefit from increased support to promote psychosocial adaptation is well described in the literature, Reference Woolf-King, Anger, Arnold, Weiss and Teitel23,Reference Denniss, Sholler, Costa, Winlaw and Kasparian31,Reference Kasparian, Winlaw and Sholler42,Reference Demianczyk, Behere and Thacker140,Reference Earls, Yogman, Mattson and Rafferty141 and formal recommendations from the Association for European Pediatric and Congenital Cardiology Psychosocial Working Group, Reference Utens, Callus, Levert, Groote and Casey41 Australian National Strategic Action Plan for Childhood Heart Disease, 142 and American Board of Pediatrics 43 include screening and assessment of parent mental health as crucial components of CHD care. There is an extensive literature on models of screening and assessment for family psychosocial risk and psychological distress within other paediatric illness populations, Reference Kazak, Schneider, Didonato and Pai143,Reference Haverman, van Oers and Limperg144 and recent papers provide preliminary support for their applicability to parents of newborns with prenatally diagnosed birth defects in the early post-partum period, Reference Cole, Olkkola, Zarrin, Berger and Moldenhauer145 parents of children with CHD following cardiac surgery, Reference Hearps, McCarthy and Muscara146–Reference McCarthy, Hearps and Muscara147 and parents of children who underwent heart transplantation. Reference Cousino, Schumacher and Rea148 In addition, a trial evaluating a family-based mental health screening and stepped care model within paediatric cardiology is underway in Australia. Reference Kasparian, Winlaw and Sholler42,Reference Tesson, Butow, Sholler, Sharpe, Kovacs and Kasparian45
Significant gaps in knowledge
Although the importance of routinely assessing parent mental health and family functioning within the context of CHD is well understood, existing research has not defined which specific aspects of mental health and family functioning should be assessed at which time points. Screening efforts to date have focused primarily on parent and family risk factors, with less emphasis on protective factors to promote psychosocial adaptation and positive child neurodevelopmental and psychosocial outcomes. Additionally, factors impacting the feasibility and acceptability of screening parents of children with CHD within routine clinical practice, and facilitating access to mental health services following a positive screen, have not been adequately explored. Finally, it is not known whether screening results in improved outcomes for families of children with CHD, and whether these outcomes are similar across diverse groups.
Investigations needed
-
(1) Identify the optimal tools and timing for routine screening and assessment of parent mental health and family functioning in clinical care settings.
Informed by theoretical models and psychometric studies (Critical Question 1) and by widespread efforts to promote mental health screening in health care settings, Reference Earls, Yogman, Mattson and Rafferty141,Reference Kazak, Schneider, Didonato and Pai143,Reference Austin, Highet and Expert149–Reference Cella, Riley and Stone151 research must identify the optimal tools for routine screening and assessment of important parent and family risk and resilience factors within the CHD population. Screening and assessment tools should screen for constructs that are clinically meaningful to parents and families, Reference Batalden, Batalden, Margolis, Seid, Armstrong, Opipari-Arrigan and Hartung138 gather information from multiple members in the family system, Reference Van Schoors, Caes, Verhofstadt, Goubert and Alderfer152 emphasise building a family resilience framework, Reference Faccio, Renzi, Giudice and Pravettoni153 consider potential financial burden and opportunity costs, Reference Elhoff, McHugh, Buckley, Morris, Simpson and Scheurer39,Reference Connor, Kline, Mott, Harris and Jenkins40 and be available and provide accommodations for use across languages, cultures, and ability levels. Building on knowledge regarding longitudinal trajectories of parent mental health and family functioning (Critical Question 3), research must also identify optimal time points for routine screening and assessment, such as times when families are likely to be at greatest risk or during windows of opportunity for promoting psychosocial adaptation.
-
(2) Determine the feasibility and acceptability of screening and assessment processes for diverse stakeholders.
Qualitative and mixed methods approaches may be helpful for obtaining the perspectives of diverse stakeholder groups (e.g., parents, physicians, social workers, clinic staff) regarding screening/assessment processes and strategies for connecting families with the appropriate supports following a positive screen. Reference Reader, Ruppe and Deatrick84,Reference Alderfer and Sood137 Evidence-based online or mobile screening applications have demonstrated feasibility and acceptability in other high-risk populations such as military veterans, Reference Pittman, Floto, Lindamer, Baker, Lohr and Afari154 children affected by war, Reference Hashemi, Ali, Awaad, Soudi, Housel and Sosebee155 and patients with cancer, Reference Schepers, Sint Nicolaas and Haverman156 and could be adapted and tested with families of children with CHD.
-
(3) Evaluate whether routine screening of parent mental health and family functioning increases access to care and improves outcomes.
Rigorous studies are needed to evaluate the clinical efficacy and cost-effectiveness of routine screening of parent mental health and family functioning in both the short- and long term. Barriers to disclosing mental health need to medical providers Reference Wissow, Anthony and Brown157 and to accessing mental health assessment and intervention services following a positive screen are common Reference Shemesh, Lewis and Rubes158,Reference Struemph, Barhight, Thacker and Sood159 and must be identified and addressed for diverse families impacted by CHD. In particular, studies should evaluate whether routine screening processes reduce existing ethnic, racial, and socioeconomic disparities in identifying risks and accessing services within the CHD population. Reference Loccoh, Yu, Donohue and Lowery135,Reference Gonzalez, Kimbro and Cutitta136 Research should also identify the resources necessary to implement family psychosocial screening within paediatric cardiology. Based on studies evaluating mental health screening in perinatal settings, Reference Cole, Olkkola, Zarrin, Berger and Moldenhauer145,Reference Gordon, Cardone, Kim, Gordon and Silver160 mental health providers embedded within the health care practice and staff trained to respond to urgent mental health needs seem to be critical components of an efficacious screening process.
Critical Question 5: How and when should interventions be offered to bolster parent mental health and family adaptation, and optimise child neurodevelopmental and psychosocial outcomes?
Existing knowledge
Two recent systematic reviews synthesised and critically appraised evidence on the efficacy of psychological interventions for parents and families of children with CHD. Reference Kasparian, Kan, Sood, Wray, Pincus and Newburger44,Reference Tesson, Butow, Sholler, Sharpe, Kovacs and Kasparian45 Interventions vary widely in terms of therapeutic approach (e.g., education and parenting skills training, promoting parent–infant interaction and bonding, early paediatric palliative care). Tested interventions demonstrated reductions in maternal anxiety, with mixed evidence of efficacy for other parent (e.g., depression) and child (e.g., neurodevelopment, feeding) outcomes. Notably, very few studies included fathers or racial and ethnic minorities. Research examining parent preferences indicates that parents want interventions focused on direct management of parent mental health symptoms. Reference Gramszlo, Karpyn and Demianczyk46 In addition, parents want peer support provided by other experienced parents as well as education on how to effectively communicate with medical teams, advocate for their child’s needs, and partner in their child’s medical and developmental care during hospitalisation. Reference Gramszlo, Karpyn and Demianczyk46 Studies on parent preferences for communication and decision-making suggest that candid medical information delivered over time, sensitivity to cultural and linguistic diversity, provider validation of emotional responses and needs, and acknowledgement of the impact of medical care on the family can be helpful for mitigating parent stress. Reference Gramszlo, Karpyn and Demianczyk46,Reference Neubauer, Williams, Donohue and Boss161,Reference Pagel, Bull and Utley162
Significant gaps in knowledge
Literature on the development, adaptation, and implementation of interventions targeting parent mental health and family functioning in CHD is still in its infancy and many knowledge gaps remain. Existing interventions for this population are heterogeneous in terms of content, dose, timing, delivery format, and target outcomes, and the comparative effectiveness, feasibility, and cost-effectiveness of various intervention approaches and mechanisms of action are unknown. The needs of fathers, racial and ethnic minorities, and LGBTQ communities have not been specifically targeted, and strategies to increase the participation of under-represented groups in CHD intervention research have not been well-defined. Numerous family-based interventions have been developed and tested for other high-risk populations, Reference Law, Fisher, Fales, Noel and Eccleston163 yet few studies have examined the extent to which these interventions can be successfully adapted and delivered to families affected by CHD. Despite the growing literature on parent preferences for intervention, support, and communication, Reference Woolf-King, Arnold, Weiss and Teitel17,Reference Sood, Karpyn and Demianczyk25,Reference Gramszlo, Karpyn and Demianczyk46,Reference Neubauer, Williams, Donohue and Boss161,Reference Pagel, Bull and Utley162,Reference Blankenship, Harrison, Brandt, Joy and Simsic164 formalised peer support interventions have not been developed or evaluated for their impact on parent mental health, and studies exploring effective models of parent–provider communication and shared decision-making are very limited in CHD. Reference Neubauer, Williams, Donohue and Boss161 Cultural nuances regarding parent preferences for support and communication have also not been adequately explored. Reference Zurca, Wang, Cheng, Dizon and October165 Importantly, there is an absence of rigorous randomised controlled trials designed to determine the efficacy of family-based interventions for improving parent mental health, family functioning, and ultimately child neurodevelopmental and psychosocial outcomes in CHD. Reference Kasparian, Kan, Sood, Wray, Pincus and Newburger44,Reference Tesson, Butow, Sholler, Sharpe, Kovacs and Kasparian45
Investigations needed
-
(1) Evaluate interventions using rigorous randomised controlled efficacy trials, followed by effectiveness trials that guide real-world implementation.
A recent systematic review and best practice statement strongly endorses the provision of mental health interventions for parents of infants with CHD during ICU admission. Reference Kasparian, Kan, Sood, Wray, Pincus and Newburger44 In order to implement evidence-based interventions in clinical care settings, this recommendation first requires the establishment of efficacy through use of tightly controlled randomised clinical efficacy trials using validated and theory-based outcome measures. Once efficacy is established, effectiveness trials that are designed to answer questions about real-world implementation and inclusive of economic evaluation are an essential next step. It is important to note here that while efficacy and effectiveness trials are distinct and equally important steps in the development of evidence-based behavioural treatments, efficacy trials can be designed with effectiveness in mind by considering the setting to which the intervention will be eventually delivered. Reference Czajkowski, Powell and Adler166–Reference Carroll and Rounsaville167 For example, evaluating a mode of delivery (e.g., telehealth) that is likely to be both cost-effective and implementable. Reference Tesson, Swinsburg and Kasparian168 Multicentre studies are required to ensure adequate population diversity and adequate sample sizes. The “trial within a registry” method, which uses clinical registries as data platforms for randomised clinical trials, has been proposed as a way to leverage existing data, decrease research study costs, and enhance generalisability across settings. Reference Lauer and D’Agostino169
-
(2) Adapt interventions developed for other high-risk populations and determine optimal intervention content, format, timing, and dose.
Using the literature with perinatal and neonatal ICU populations as a foundation may expedite the development of interventions in CHD. Reference Jotzo and Poets170–Reference Shaw, St John and Lilo172 Cognitive-behavioural approaches have demonstrated efficacy for these high-risk populations and warrant adaptation to and testing with parents of children with CHD. Reference Mendelson, Cluxton-Keller, Vullo, Tandon and Noazin171,Reference Sockol173 Transdiagnostic interventions, referring to those treatments that target the core maladaptive processes underlying many mental health disorders (e.g., mindfulness-based interventions, acceptance and commitment therapy), Reference Newby, McKinnon, Kuyken, Gilbody and Dalgleish174 have also shown promise for reducing depression, anxiety, and trauma for mothers of infants in the neonatal ICU Reference Mendelson, McAfee, Damian, Brar, Donohue and Sibinga175 and could be adapted and tested for parents of children with CHD during the prenatal period, during hospitalisation, and after hospital discharge. Reference Golfenshtein, Deatrick, Lisanti and Medoff-Cooper176,Reference Cassidy177 Family integrated care, which enables parents to become primary caregivers in the neonatal ICU, has been found to decrease parent stress and anxiety and could be adapted for cardiac inpatient settings. Reference O’Brien, Robson, Bracht, Cruz, Lui, Alvaro, da Silva, Monterrosa, Narvey, Ng, Soraisham, Ye, Mirea, Tarnow-Mordi and Lee178 Interventions that have been shown to improve parent mental health, family functioning, and child outcomes by teaching parents skills to manage child emotional and behavioural problems may warrant adaptation for families of preschool and school-age children with CHD. Reference Lebowitz, Marin, Martino, Shimshoni and Silverman179–Reference McEachern, Fosco, Dishion, Shaw, Wilson and Gardner181 The process of adapting existing interventions and determining optimal content, format, timing, and frequency should be conducted in accordance with established guidelines Reference Czajkowski, Powell and Adler166,Reference Craig, Dieppe, Macintyre, Michie, Nazareth and Petticrew182,183 and cultural and linguistic competencies Reference Marsiglia and Booth184 and in partnership with parent and clinician stakeholders to ensure that the resulting intervention is acceptable and feasible and targets meaningful outcomes. Reference Goodman and Sanders Thompson74 The adaptation process should conclude with full-scale efficacy trials followed by effectiveness trials as described above.
-
(3) Explore the effects of incorporating shared decision-making and peer support into interventions.
A clinical report from the American Academy of Pediatrics describes a systematic approach to the implementation of shared decision-making for children with disabilities, which includes involving children in decisions about their care and developing decision-support tools and technologies. Reference Adams and Levy185 This may be a useful framework from which to develop, adapt, and evaluate communication and shared decision-making resources for children with CHD and their parents. Importantly, preferences for shared decision-making are likely to differ across cultural, racial, and ethnic groups, Reference Perez Jolles, Richmond and Thomas186 and the concept may be incongruent with some cultural values. The process of shared decision-making is also likely to change throughout phases of care and with increased child age. Reference Jordan, Wood, Edwards, Shepherd and Joseph-Williams187 Studies should evaluate the impact of shared decision-making on parent, family, and child outcomes at key transition points, from the time of initial diagnosis through the transition to adulthood. Additionally, those designing or adapting interventions should consider incorporating formalised peer support, with a focus on diversity and representation, to enhance parent outcomes including perceived social support, confidence, and empowerment. Reference Hall, Ryan, Beatty and Grubbs188 Hospital–community partnership activities, such as patient/family advocacy groups, summer camps, and family education days, are promising methods for the delivery of peer support, Reference Hall, Ryan, Beatty and Grubbs188,Reference Moola, Faulkner, White and Kirsh189 but require further evaluation with diverse peer mentors/mentees, including long-term follow-up Reference Moola, Faulkner, White and Kirsh189 and examination of sex and cultural differences regarding preferences for peer support. Reference Sood, Karpyn and Demianczyk25
-
(4) Explore technology-based modes of intervention delivery.
Behavioural intervention technologies, such as mental health and wellness interventions using web-based programmes and videoconferencing techniques, should be considered given the potential of new technology to increase access and reduce barriers to behavioural healthcare for families. Reference Mohr, Burns, Schueller, Clarke and Klinkman190 Interventions demonstrated to be efficacious and effective with families of children with CHD could be translated into technology-based interventions. Reference Canter, Deatrick and Hilgart191–Reference Mohr, Hart and Julian195 Alternatively, behavioural intervention technologies could be incorporated in the early stages of intervention development. Reference Swallow, Carolan and Smith196,Reference Wysocki, Pierce and Caldwell197 The extent to which technology-based interventions can reduce disparities in access to behavioural healthcare for under-represented groups should be specifically evaluated.
Cross-cutting themes
Several themes cut across the five critical questions outlined above. Representation of patients, parents, and families from diverse backgrounds is critical to understanding how race, ethnicity, culture, sex, socioeconomic status, LGBTQ identity, implicit bias, discrimination, and other factors influence and potentially contribute to health disparities in parent mental health, family functioning, parenting and child outcomes in CHD. The feasibility, acceptability, efficacy, and effectiveness of mental health screening, assessment, and intervention strategies are likely to differ across diverse populations, and appropriate tailoring and adaptation are essential. Strategies that have been effective in increasing sample diversity (including non-English-speaking participants) for other populations should be utilised or adapted for studies of parent mental health and family functioning in CHD. Reference Otado, Kwagyan, Edwards, Ukaegbu, Rockcliffe and Osafo198–Reference Ejiogu, Norbeck, Mason, Cromwell, Zonderman and Evans201 Health system diversity with regard to structure, financing, and policy (both within and across nations) and disparities in access to health insurance also influence how physical and mental health services are delivered to children and families, and which barriers to care are likely to be most salient. Reference Macinko, Starfield and Shi202–Reference Levesque, Harris and Russell204 These issues must be considered when designing and implementing efficacy and effectiveness trials and quality improvement initiatives related to parent mental health and family functioning. Despite the critical need for increased knowledge of parent mental health and family functioning following CHD diagnosis, much of the prior research on this topic represents cross-sectional, survey-based studies, single-centre qualitative investigations, secondary analysis of existing data, and/or controlled trials with high risk of bias, and primarily with English-speaking White mothers. Reference Woolf-King, Anger, Arnold, Weiss and Teitel23,Reference Kasparian, Kan, Sood, Wray, Pincus and Newburger44,Reference Tesson, Butow, Sholler, Sharpe, Kovacs and Kasparian45 Innovative methodological approaches and technological advances in electronic data capture, biomarker-based approaches, screening and assessment processes, tightly controlled efficacy trials, and implementable intervention strategies must be applied to advance knowledge, clinical care, and outcomes for families of children with CHD.
Conclusions
Neurodevelopmental and psychological difficulties are amongst the most common comorbidities of individuals with CHD. While a complex constellation of factors contributes to individual outcomes, parent psychosocial factors are foundational elements contributing to child health and well-being. Caring for a child with complex forms of CHD places significant demands on parents with strong evidence for parent vulnerability to high levels of acute and persistent psychological stress. The limited number of published mental health interventions for parents of children with CHD provide preliminary evidence of efficacy in reducing maternal distress and improving coping and psychosocial adaptation, but there remain substantial knowledge gaps, particularly in terms of the efficacy and effectiveness of interventions in improving paternal and child mental health, or outcomes for families from culturally- or linguistically diverse backgrounds, LGBTQ communities, or low-resource settings.
After a comprehensive review of the literature and extensive stakeholder engagement, the Parent Mental Health and Family Functioning Working Group identified five priorities to guide the advancement of research, clinical practice, and health policy:
(1) Conceptually driven investigations using reliable and validated measures to identify parent mental health and family functioning factors with the strongest influence on child neurodevelopmental and psychosocial outcomes and health-related quality of life;
(2) Interdisciplinary collaborations to elucidate the psychobiological underpinnings of neurodevelopmental and psychosocial deficits in children with CHD, including a deeper understanding of the biomarkers associated with these outcomes;
(3) Trajectories of child, parent, and family mental health, and the individual and environmental factors that may influence pathways to both risk and resilience, as well as identification of “sensitive” or “critical” periods when intervention may be of greatest benefit;
(4) Development, trial, and implementation of sustainable models of mental health screening and assessment with capacity for tailoring to a range of settings and cultures; and
(5) Establishment of a suite of efficacious and effective interventions to optimise parent mental health and family functioning in order to promote psychosocial adaptation to achieve the best possible neurodevelopmental and psychosocial outcomes for children with CHD.
These ambitious priorities highlight the diverse and often unmet mental health needs of families of children with CHD and provide a roadmap for the future of our field. With patients, families, researchers, clinicians, policymakers, and industry leaders working in strong partnership, we are set to change the landscape of mental healthcare – and outcomes – for people of all ages with CHD and their families.
Acknowledgements
The members of the Parent Mental Health and Family Functioning Working Group would like to thank Dawn Ilardi, Wendy Nembhard, Jacqueline Sanz, Catherine Ullman Shade, Janice Ware, and the Publications Committee of the Cardiac Neurodevelopmental Outcome Collaborative for their thoughtful review of this manuscript.
Financial support
This work was supported by the National Heart, Lung, and Blood Institute (grant number 1R13HL142298-01).
Conflicts of interest
None.





