The care of children with CHD is a challenging aspect of medicine in countries all over the world. There is no general consensus about how to organise the distribution of healthcare centres that are involved in this highly demanding type of care. Many different approaches have been used: regionalisation, “safari” missions, “travels of hope”, and twinning programmes.Reference Dearani, Neirotti and Kohnke 1 Many distinguished experts and politicians view regionalisation of paediatric cardiac services as an organised approach towards excellent hyper-specialised, high volume load services coupled with optimal management in developed countries.Reference Chang and Klitzner 2 – Reference Daenen, Lacour-Gayet and Aberg 4 These types of programmes may, in fact, represent an excellent opportunity for optimising outcomes for children with CHD. This may be particularly true when children with CHD and their families have easy, fast, and safe access to those excellent healthcare providers; however, what happens when a patient with CHD is located in an ultra-peripheral region that involves a flight of several hours to reach the nearest surgical cardiac centre on the mainland? We would like to present our unique experience of providing high-quality care to children with CHD in the Canary Islands, a peripheral region of Europe.
The Canary Islands archipelago, part of the Kingdom of Spain, is located in the Atlantic Ocean, 96 km off the north-west coast of Saharan Africa. In 2007, the Canary Islands Government decided to establish a new paediatric cardiac surgery programme with the support of a high-volume paediatric cardiac centre. An international partnership between the medical surgical unit of paediatric cardiology and heart abnormalities, Complejo Hospitalario Universitario Insular Materno Infantil, in Las Palmas de Gran Canaria, and the division of cardiac surgery, Policlinico San Donato (San Donato Milanese, Milan, Italy), was instituted. The goals of this unique European partnership were to provide surgical treatment in Las Palmas de Gran Canaria to all Canary Island children with CHD regardless of the complexity of the case and to train local staff by establishing a humanitarian cooperation for treating CHD that comes from underserved African regions. This article presents and discusses the results and strategies adopted by this partnership.
Materials and methods
From January, 2007 to April, 2013, the Medical Surgical Unit of Paediatric Cardiology and Heart Abnormalities within Complejo Hospitalario Universitario Insular Materno Infantil had three paediatric cardiac surgeons, where two of them had been on staff before 2007, three paediatric cardiologists, two interventional cardiologists, both trained in adult and paediatric CHD, two paediatric cardio-anaesthetists, two perfusionists, and one intensivist paediatric cardiologist. The technological facilities included one catheterisation laboratory for interventional cardiology, shared with the adult cardiology service, one operating theatre with two pumps for extracorporeal circulation, a general paediatric ICU with 10 beds, a general neonatal ICU with 20 beds, a dedicated ward with 11 beds, and three outpatient clinics with two echocardiography machines, and one treadmill in total. The medical surgical unit of paediatric cardiology and heart abnormalities established a protocol of assistance for mothers and their neonates who had CHD in cooperation with Complejo Hospitalario Universitario Insular Materno Infantil’s gynaecology, neonatology, and paediatric services.
As the only paediatric cardiac surgery service in the archipelago that was capable of handling heart abnormalities, no matter what their causes, the medical surgical unit of paediatric cardiology and heart abnormalities received referrals for all patients with CHD. Every patient who was admitted was given financial support by the Spanish social security system regardless of family income.
Every month a team that included a senior surgeon, a paediatric cardiologist, an anaesthesiologist, and a perfusionist from Policlinico San Donato was hosted in Las Palmas de Gran Canaria for a 5-day session of surgery and teaching. All patients who had CHD and were considered to be candidates for surgery were presented by their paediatric cardiologists from the Canary Islands in these monthly clinical meetings in Las Palmas de Gran Canaria. There was always an initial presentation 1 or 2 months before the surgical appointment in order to verify the surgical indication. A second presentation almost always occurred on the morning of the surgical intervention with the intent of defining the surgical strategy in the operating room. Complex cases were all scheduled to take place at the very beginning of the surgical week, so that the senior surgeon, paediatric cardiologist, and anaesthesiologist from Policlinico San Donato were able to follow-up these complex cases for 5 postoperative days.
The operative algorithm adopted by the joint programme was as follows (Tables 1 and 2):
-
∙ Elective surgeries were performed in Las Palmas de Gran Canaria by a surgical team with members from the two institutions and were always led by a senior surgeon from Policlinico San Donato. Before every surgical session, the surgical team including surgeons, nurses, and perfusionists reviewed the critical steps of the procedure, and the following criteria were used in order to achieve the best results for the patient:
-
o If the Aristotle Basic ScoreReference Lacour-Gayet, Clarke and Jacobs 5 was above 10, the surgery was performed by a Policlinico San Donato paediatric cardiac surgeon assisted by Complejo Hospitalario Universitario Insular Materno Infantil paediatric cardiac surgeons.
-
o If the Aristotle Basic Score was from 6 to 10, the surgery was performed by a Complejo Hospitalario Universitario Insular Materno Infantil paediatric cardiac surgeon assisted by a Policlinico San Donato paediatric cardiac surgeon.
-
o If the Aristotle Basic Score was from 1 to 5, the surgery was performed by Complejo Hospitalario Universitario Insular Materno Infantil paediatric cardiac surgeons supervised by a Policlinico San Donato paediatric cardiac surgeon.
-
o The individual skills of the Complejo Hospitalario Universitario Insular Materno Infantil paediatric cardiac surgeons were considered for each neonatal cardiac surgery with an Aristotle Basic Score below 10.
-
∙ Urgent cases were managed in three different ways:
-
o If the patient was clinically stable but required cardiac surgery and had an Aristotle Basic Score above 6, a surgical team composed of members of the two institutions was to perform the surgery within 72 hours in Las Palmas de Gran Canaria. Regardless of the complexity of the case, the operator surgeon was always a senior paediatric cardiac surgeon from Policlinico San Donato.
-
o If the patient was clinically unstable but required cardiac surgery and had an Aristotle Basic Score above 6, and there was also no possibility of performing the surgery within 72 hours in Las Palmas de Gran Canaria, a transfer was required to take the patient to a paediatric cardiac surgery centre on the mainland of Spain after a briefing with the senior paediatric cardiac surgeon on call in Milan.
-
o If the patient was clinically stable or unstable but required cardiac surgery and had an Aristotle Basic Score below 6, Complejo Hospitalario Universitario Insular Materno Infantil paediatric cardiac surgeons were to perform the surgery immediately after a teleconference briefing with the senior paediatric cardiac surgeon on call in Milan.
-
∙ Emergencies were always under the full responsibility of Complejo Hospitalario Universitario Insular Materno Infantil paediatric cardiac surgeons after a briefing with the senior paediatric cardiac surgeon on call in Milan.
Table 1 Joint programme operative algorithm for elective surgery 2007–2012.

CHUIMI=Complejo Hospitalario Universitario Insular Materno Infantil; PSD=Policlinico San Donato; ABS=Aristotle Basic Score
Table 2 Joint programme operative algorithm for urgent surgery 2007–2013.
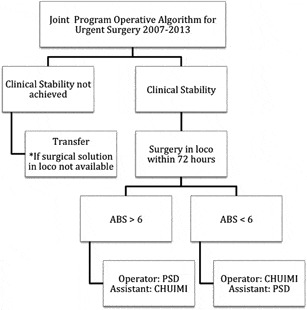
CHUIMI=Complejo Hospitalario Universitario Insular Materno Infantil; PSD=Policlinico San Donato; ABS=Aristotle Basic Score
This study included all patients who had undergone surgical interventions for CHD from January, 2009 to March, 2013 in Las Palmas de Gran Canaria. Demographic and in-hospital variables were collected, such as the surgical procedure, diagnosis, age and weight at operation, the intermittent positive pressure ventilation hours, and the length of hospital stay, from medical records by a single physician and were matched with the register of cardiac intervention, the ICU register, and the in-hospital administrative database. The same physician introduced all data and examined the congenital database of the European Congenital Heart Surgeons Association. Preterm infants with patent ductus arteriosus were not included in the statistical analysis unless otherwise specified.
Results
The results are presented according to the objectives of the joint programme.
To provide surgical treatment to all children with CHD in the Canary Island archipelago
From January, 2009 to March, 2013, 65 surgical missions were undertaken. The congenital database of the European Congenital Heart Surgeons Association documented 214 patients – cases of patent ductus arteriosus in preterm neonates were excluded – with a mean age at surgery of 36.45 months and a mean weight of 12.89 kg. There were 316 procedures with 198 cardiopulmonary bypass cases, 46 non-cardiopulmonary bypass cases, 26 cardiovascular cases without cardiopulmonary bypass, 22 miscellaneous other types of cases, 16 interventional cardiology cases, six thoracic cases, one non-cardiac, non-thoracic procedure on a cardiac patient with cardiac anaesthesia, and one extracorporeal membrane oxygenation case. The mean total cardiopulmonary bypass time was 99.55 minutes, the mean cross-clamping time was 50.91 minutes, the mean circulatory arrest time was 28.88 minutes (16 cases), the mean intermittent positive pressure ventilation time was 59.21 hours, the mean length of the hospital stay was 19.38 days, and the 30-day mortality was 6.07% (13 patients). The procedures are reported in Table 3.
Table 3 Paediatric cardiac surgery interventions 01/2009–03/2013.

ASD=atrial septal defect; AVC=atrioventricular canal; AVSD=atrioventricular septal defect; DORV=double outlet right ventricle; MAPCAs=major aortopulmonary collateral arteries; PA=pulmonary arterial; PAB=pulmonary artery banding; PAPVC=partial anomalous pulmonary venous connection; PVR=pulmonary vascular resistance; RV=right ventricular; RVOT=right ventricular outflow tract; TAPVC=total anomalous pulmonary venous connection; TOF=tetralogy of Fallot; VSD=ventricular septal defect
Information related to the patients’ ages:
-
∙ Neonates (0–30 days): there were 47 patients; the mean age at surgery was 0.39 months and the mean weight was 3.18 kg. There were 79 procedures with 30 cardiopulmonary bypass cases, 16 non-cardiopulmonary bypass cases, 15 cardiovascular cases without cardiopulmonary bypass, 10 interventional cardiology cases, six miscellaneous other types of cases, one non-cardiac, non-thoracic procedure on a cardiac patient with cardiac anaesthesia, and one thoracic case. The mean total cardiopulmonary bypass time was 143.90 minutes, the mean cross-clamping time was 61.23 minutes, the mean circulatory arrest time was 36.90 minutes (10 cases), the mean intermittent positive pressure ventilation time was 173.26 hours, the mean length of the hospital stay was 30.54 days, and the 30-day mortality rate was 12.77% (six patients).
-
∙ Infants (31–365 days): there were 65 patients; the mean age at surgery was 4.75 months and the mean weight was 5.40 kg. There were 74 procedures with 44 cardiopulmonary bypass cases, 17 non-cardiopulmonary bypass cases, two cardiovascular cases without cardiopulmonary bypass, one interventional cardiology case, seven miscellaneous other types of cases, and three thoracic cases. The mean total cardiopulmonary bypass time was 101.68 minutes, the mean cross-clamping time was 55.84 minutes, the mean circulatory arrest time was 11.33 minutes (three cases), the mean intermittent positive pressure ventilation time was 58.12 hours, the mean length of the hospital stay was 17.43 days, and the 30-day mortality rate was 4.62% (three patients).
-
∙ Children (1–18 years): there were 129 patients; the mean age at surgery was 67.27 months and the mean weight was 20.75 kg. There were 162 procedures with 123 cardiopulmonary bypass cases, 13 non-cardiopulmonary bypass cases, nine cardiology cases without cardiopulmonary bypass, five interventional cardiology cases, nine miscellaneous other types of cases, two thoracic cases, and one extracorporeal membrane oxygenation. The mean total cardiopulmonary bypass time was 88.01 minutes, the mean cross-clamping time was 45.77 minutes, the mean circulatory arrest time was 19.67 minutes (three cases), the mean intermittent positive pressure ventilation time was 18.65 hours, the mean length of the hospital stay was 18.84 days, and the 30-day mortality rate was 2.33% (three patients).
-
∙ Adult (>18 years): there was one patient whose age at surgery was 237.67 months with a weight of 59 kg. The procedure involved one cardiopulmonary bypass. The total cardiopulmonary bypass time was 94 minutes, the cross-clamping time was 70 minutes, the mean intermittent positive pressure ventilation time was 18.65 hours, and the length of the hospital stay was 18 days. The patient unfortunately died.
In all, 10 patients with complex CHD were transferred to surgical centres on the mainland for surgery with extracorporeal membrane oxygenation backup or heart transplant facilities. Transferal mortality was 0%.
We analysed our results in further detail, benchmarking them against the European Congenital Heart Surgeons Association Congenital Database (Table 4). The following results are based on a smaller pool of patients because the database did not include the procedures that were more performed in less than 10 cases: there were 915 patients, the performance was 0.64, the mortality score was 0.67, the Aristotle Basic Score was 7.18, and the 30-day mortality rate was 4.10%.
Table 4 Benchmarking joint programme paediatric cardiac surgery – European Association for Cardio-Thoracic Surgery (EACTS) European centres.

CHUIMI=Complejo Hospitalario Universitario Insular Materno Infantil
Splitting those data by age group produced the following:
-
∙ Neonates (0–30 days): there were 35 patients; our mean performance was 1.14, with a mean mortality score of 1.33, a mean Aristotle Basic Score of 9.15, and a 30-day mortality rate of 14.29%.
-
∙ Infants (31–365 days): there were 47 patients; our mean performance was 0.65, with a mean mortality score of 0.68, a mean Aristotle Basic Score of 7.57, and a 30-day mortality rate of 4.26%.
-
∙ Children (1–18 years): there were 112 patients; our mean performance was 0.45, with a mean mortality score of 0.45, a mean Aristotle Basic Score of 6.38, and a 30-day mortality rate of 0.00%.
-
∙ Adult (>18 years): there was one patient; our mean performance was 0.00, with a mortality score of 1.30, an Aristotle Basic Score of 7.50, and a 30-day mortality rate of 100.00% (Fig 1).

Figure 1 Joint programme 2009–2013: activity by age.
The mean basic score was stable for each age group for the entire study period (Fig 2). Neonatal cardiac surgery represented the most challenging aspect of the joint programme because the neonate mean basic score was the highest and urgent surgery was performed in many cases. The mean performance was also stable from 2009 to 2013 (Fig 3). The 30-day mortality was not worse compared with the expected mortality (Fig 4).

Figure 2 Joint programme 2009–2013: mean basic score by age.

Figure 3 Joint programme 2009–2013: mean performance trend chart elaborated from the European Congenital Heart Surgeons Association Congenital Database.

Figure 4 Joint programme 2009–2013: expected mortality versus 30-day mortality elaborated from the European Congenital Heart Surgeons Association Congenital Database.
As this is a very small surgical service, meticulous attention was directed towards patient safety: seven different clinical protocols were edited and six out of seven were submitted and approved by the Complejo Hospitalario Universitario Insular Materno Infantil’s Quality Commission. Mortality and morbidity sessions were held periodically, and attendance by the Policlinico San Donato team was considered mandatory.
To train local staff and achieve scientific production
From 2007 to 2009, Policlinico San Donato always supported surgical missions to Complejo Hospitalario Universitario Insular Materno Infantil. Policlinico San Donato provided teams with a senior paediatric cardiac surgeon, a paediatric cardiologist, an anaesthesiologist, and a perfusionist on a monthly basis. During this time frame of the joint programme, all members of the Medical Surgical Unit of Paediatric Cardiology and Heart Abnormalities were required to retrain by attending the partner institution in Milan on a regular basis. Anaesthesiologists, perfusionists, paediatric cardiologists, paediatric intensivists, and paediatric cardiac surgeons were asked to perform clinical work under the strict surveillance of Policlinico San Donato resident staff. From 2009 until the end of the period, on-demand clinical rotation at Policlinico San Donato was offered to all Complejo Hospitalario Universitario Insular Materno Infantil professionals and residents who were working with CHD. Policlinico San Donato offered free attendance to its international meetings on CHD in Milan.
In early 2009, Policlinico San Donato and Complejo Hospitalario Universitario Insular Materno Infantil agreed on an acceptable level of competence in the perioperative management of simple cases and medium-complexity cases of CHD undertaken by the Medical Surgical Unit of Paediatric Cardiology and Heart Abnormalities. Policlinico San Donato then modified the composition of the surgical team sent from Italy: a senior paediatric cardiac surgeon and a paediatric cardiologist travelled to the Canary Islands every month. From 2009 to 2013, when the monthly surgical sessions were facing challenges because of high-complexity cases, the clinical coordinator of the Medical Surgical Unit of Paediatric Cardiology and Heart Abnormalities was allowed to call for a surgical team composed of four instead of two members, including a perfusionist, an anaesthesiologist, a senior paediatric cardiac surgeon, and a paediatric cardiologist. From 2009 to 2013, the paediatric cardiac surgeons from the Medical Surgical Unit of Paediatric Cardiology and Heart Abnormalities performed 85 surgical interventions either under supervision or independently: 11 neonates, 14 infants, 59 children, and one adult (Table 5).
Table 5 Surgical activity by group.

CHUIMI=Complejo Hospitalario Universitario Insular Materno Infantil; PSD=Policlinico San Donato
Working as a team under the supervision of an expert trainer, Complejo Hospitalario Universitario Insular Materno Infantil paediatric cardiac surgeons were finally able, by the second semester of 2012, to perform elective cases and some selected urgent cases of low and medium complexity (Figs 5 and 6). Complejo Hospitalario Universitario Insular Materno Infantil and Policlinico San Donato subsequently adopted new algorithm criteria (Table 6) and a new schedule for surgical activity:
-
∙ Interventions with an Aristotle Basic Score below 6 were always performed by Complejo Hospitalario Universitario Insular Materno Infantil paediatric cardiac surgeons and no longer included any supervision.
-
∙ Interventions with an Aristotle Basic Score from 6 to 10 were performed by Complejo Hospitalario Universitario Insular Materno Infantil paediatric cardiac surgeons under the supervision of the Policlinico San Donato senior paediatric cardiac surgeon who was always present in the operating room.
-
∙ Interventions with an Aristotle Basic Score above 10 were always performed by a Policlinico San Donato senior paediatric cardiac surgeon as the first operator and a Complejo Hospitalario Universitario Insular Materno Infantil paediatric cardiac surgeon as the first assistant.
-
∙ There were no other changes in the management of urgent and emergency cases.

Figure 5 Complejo Hospitalario Universitario Insular Materno Infantil (CHUIMI) 2009–2013: activity by age.

Figure 6 Complejo Hospitalario Universitario Insular Materno Infantil (CHUIMI) 2009–2013: mean basic score by year and surgeon.
Table 6 Joint programme operative algorithm for elective surgery 2012–2013.

CHUIMI=Complejo Hospitalario Universitario Insular Materno Infantil; PSD=Policlinico San Donato; ABS=Aristotle Basic Score
In the period that was analysed, clinical research produced four posters in national meetings, one oral presentation in an international congress, and two original articles were published in peer reviewed international journals.Reference Iacona, Giamberti and Abella 6 – Reference Iacona, Barber and Medina 8
To establish a humanitarian cooperation for treating CHD
In 2009, the Canary Health Service promoted its leadership support for defeating CHD in developing countries. During an international meeting held in Las Palmas de Gran Canaria, an alliance was established between different non-governmental organisations working with CHD in African territories. As a result, 10 African patients received cardiac surgery free of charge at Complejo Hospitalario Universitario Insular Materno Infantil with a 0% 30-day mortality rate. Several non-profit organisations such as Associazione Bambini Cardiopatici nel Mondo in Switzerland, the Spanish Red Cross, and AIDA, Spain, and Complejo Hospitalario Universitario Insular Materno Infant shared the costs of transportation and treatment for those patients.
Nurses and physicians from Complejo Hospitalario Universitario Insular Materno Infantil participated in many surgical missions abroad with the charitable organisation Associazione del Bambino Cardiopatico, Italy.
Discussion
The Canary Islands have been considered as a peripheral region of Europe. In 2011, the archipelago had a population of 2,082,655 citizens – 4.5% of the population of Spain – distributed among seven major islands (2011 population and housing census by Instituto Nacional de Estadística or INE). 9 After considering the health demands of the local population and the geographic situation, the Canary Islands Government decided in 2000 to establish a new paediatric cardiac surgery programme. The volume load of the paediatric cardiac surgical programme at the medical surgical unit of paediatric cardiology and heart abnormalities had been low from the time that it was founded (unpublished data). In 2007, considering the need to pursue high standards of surgical care for patients with CHD and to avoid lengthy trips to the mainland of Spain, the Canary Islands Government decided to institute a joint programme between Complejo Hospitalario Universitario Insular Materno Infantil and a high-volume paediatric cardiac centre. It was clear at that time that, in the absence of official data on the prevalence of CHD in the Canary Islands, the average load for the medical surgical unit of paediatric cardiology and heart abnormalities was 130–140 children with CHD/year. In all, 100 of these patients required cardiac surgery (15–20% with an Aristotle Basic Score ⩾3). 10 On the basis of the evidence of an inverse relationship between overall surgical volume and mortality, decision makers arbitrarily chose a threshold of more than 400 cases of paediatric cardiac procedures/year for electing a partner centre.Reference Welke, O’Brien, Peterson, Ungerleider, Jacobs and Jacobs 11 They also analysed the published outcomes of data for specific types of surgery or catheterisation laboratory procedures as well as the unpublished data of previous experiences. A new era began for the medical surgical unit of paediatric cardiology and heart abnormalities when Policlinico San Donato was chosen as a new partner in treating all children with CHD regardless of the complexity. We will present and discuss the results of this international paediatric cardiac partnership with respect to the goals of this joint programme.
To provide surgical treatment to all children with CHD in the Canary Islands archipelago
The care of children with CHD is a challenging aspect of medicine in countries all over the world. Many distinguished experts and politicians view regionalisation of paediatric cardiac services in developed countries as an organised approach towards excellent hyper-specialised high volume load services coupled with optimal management and the containment of costs.Reference Chang and Klitzner 12 , Reference Lundstrom, Berggren, Bjorkhem, Jogi and Sunnegardh 13 Nevertheless, what happens when a patient with CHD is located in a peripheral region that involves a flight of several hours to reach the nearest surgical cardiac centre?Reference Hellstrom-Westas, Hanseus, Jogi, Lundstrom and Svenningsen 14 , Reference Pinto, Lasa, Dominguez, Wernovsky, Tabbutt and Cohen 15 When access to the provider requires a long journey and when safe transportation of a “susceptible” patient is not always feasible, families may choose not to travel even when they have been informed about the higher risk of mortality.Reference Finlayson, Birkmeyer, Tosteson and Nease 16 , Reference Chang, Joyce, Castillo, Ceja, Quan and Klitzner 17 A joint programme can, then, be considered as an alternative approach to regionalisation, especially in the presence of geographical limitations.
The 4-year analysis of our joint programme shows a total of 316 interventions with a mean volume load of 70–80 interventions/year. The volume load was lower than expected for a number of reasons, but the most reasonable explanation was the decreasing natality between 2007 and 2012 that was related to the serious economic crisis. 18 Our opinion is that families who were already experiencing challenges in their daily lives were less disposed to undertake difficult pregnancies. We also believe that during our partnership a small number of patients with CHD were, in fact, referred to other surgical centres on the mainland (no available data).
Hospital surgical volumes and in-hospital mortality rates have been considered to be the most important parameters in evaluating a surgical programme;Reference Sollano, Gelijns and Moskowitz 19 public reports, politicians, and public opinion rely on this type of data. We share the opinion of many authors that volume load and raw mortality appear to be unsuitable for quality judgement.Reference Welke, Karamlou, Ungerleider and Diggs 20 – Reference Pasquali, He and Jacobs 22 Therefore, in 2009, we adopted the Aristotle Basic Score and the congenital database of the European Congenital Heart Surgeons Association to evaluate surgical results.Reference Lacour-Gayet, Clarke and Jacobs 5 This activity was considered mandatory as it has provided us with a rough idea about our performance considering the risk adjustment and the surgical case mix. Our joint programme had a 30-day mortality of 6% and a surgical performance (Aristotle Basic Score X survival) in all three classes of age, which is well above the acceptable value for a referral centre according to the Spanish Ministry of Health guidelines. 10 Our programme treated a small number of neonates – most of them were complex cases with high Aristotle Basic Scores. The surgical performance of the European Congenital Heart Surgeons Association in this population can also be considered as acceptable.
In our experience, a joint paediatric cardiac surgery programme between a peripheral low-volume centre and a high-volume centre can be successful, but it should work under the following requirements:
-
∙ that the peripheral health service is able to provide excellent general paediatric healthcare
-
∙ that infrastructures and new technologies are readily available
-
∙ that surgical teams from the two centres are strongly motivated and are not operating in conflict with each other
-
∙ that politicians/managers work in perfect harmony with the providers.
To train local staff and achieve scientific production
A vast amount of scientific literature exists to support the relationship between the volume load of a single surgeon and his or her results in cardiac surgery, vascular surgery, and general surgery.Reference Birkmeyer, Stukel, Siewers, Goodney, Wennberg and Lucas 23 In order to provide the best possible care and to avoid exposure to unsafe surgical procedures, we created an algorithm for treatment based on the complexity of the surgical procedure and the clinical stability of the patient (Tables 1 and 2). The 6% 30-day mortality rate in our joint programme is the result of two factors: supervision and constant training. The joint programme also permitted intensive retraining as well as training for all members of the medical surgical unit of paediatric cardiology and heart abnormalities. It is interesting to note that the burden of the retraining was covered by the financial agreement between the two institutions – Complejo Hospitalario Universitario Insular Materno Infantil and Policlinico San Donato.
There are many legitimate questions that remain unanswered by this empiric approach as the numbers of surgeries performed by each surgeon continue to be below the suggested numbers.Reference Daenen, Lacour-Gayet and Aberg 4 This was completely true for Complejo Hospitalario Universitario Insular Materno Infantil paediatric cardiac surgeons but not for Policlinico San Donato paediatric cardiac surgeons, who were performing many more surgeries in their own primary-care centre.
A drawback to this model of collaboration that has not been completely solved by our programme is the dependency of the staff from the medical surgical unit of paediatric cardiology and heart abnormalities on the attending Policlinico San Donato team in responding to the most complicated urgent surgical patients.
To establish a humanitarian cooperation for treating CHD
We believed that a surgical centre for CHD that achieved a European standard of quality in its care could have become the hub for providing care to children with CHD coming essentially from northern Africa – Morocco and Libya – and Guinea Bissau.Reference Nguyen, Jacobs and Dearani 24 We intended to treat children who would have normal life expectancies after cardiac surgery and would require minimal follow-up in their countries. We selected patients from countries where local non-profit organisations would have contact with the medical surgical unit of paediatric cardiology and heart abnormalities before and after the surgeries performed on their children. Unfortunately, the Eurozone crisis affected Spain and Italy, among others, in 2009, and we were not able to find resources for any long-term projects after 2012.
Study limitations
We are aware of some weaknesses in our study. The interpretation of the data comes from analysis of the activity from 2009 to 2013 and is largely based on 214 patients. The partnership was established in early 2007 and, for administrative reasons, the data from 2007 until 2008 are unavailable. These data represent a large population of patients, and including their outcomes could have modified the interpretation of the surgical results. The congenital database of the European Congenital Heart Surgeons Association captures only surgical patients; the more reliable successes of our joint programme should have been considered in evaluating the care devoted to the entire CHD population that attended Complejo Hospitalario Universitario Insular Materno Infantil, regardless of the treatment they received.
We did not know how well we were performing because our volume was too low for mortality with a narrow 95% confidence interval. Unfortunately, in 2013, the partnership was interrupted; a new partner was selected, and it was not possible for the authors to undertake further analysis of the collaboration.
We did not evaluate the economic impact of the new paediatric cardiac surgery programme either on the community resources or on the family resources. In contrast to past studies, when only the resulting benchmarking and quality monitoring of healthcare were considered mandatory, a cost-effectiveness analysis should also be considered for selecting the optimal solution for children who undergo cardiac surgery.
Long-term follow-up in terms of morbidity, neurological development, functional status, and long-term mortality are not available. In other words, the quality of life of the patients after surgery is unknown.
In conclusion a joint programme between a small-volume centre and a large-volume centre may represent a valid and reproducible model for safe paediatric cardiac surgery in the complex context of a peripheral region. This type of programme may remove some major quality issues related to the small-volume workload and complex surgical case mix inherent in paediatric cardiac surgery.
Acknowledgements
G.M.I., J.A.M., S.G.M., R.G., and P.S. were physicians at the medical surgical unit of paediatric cardiology and heart abnormalities, Complejo Hospitalario Universitario Insular Materno Infantil, Las Palmas de Gran Canaria, Spain, at the time that this article was written. C.P., C.R., J.F., were paediatric cardiologists at Hospital Universitario de Canarias, San Cristóbal de La Laguna, Santa Cruz de Tenerife, Spain, at the time that this article was written. The authors thank the medical, nursing, and administrative staff members who were working in the medical surgical unit of paediatric cardiology and heart abnormalities, Complejo Hospitalario Universitario Insular Materno Infantil, Las Palmas de Gran Canaria, Spain. Without the efforts and the patience of these wonderful people the authors results would not be the same. The authors thank the visiting anaesthesiologists, perfusionists, paediatric cardiologists, paediatric intensivists, and paediatric cardiac surgeons from Italian and European Institutions. Their clinical knowledge and friendship are really much appreciated. G.M.I. thanks Dr D. Yuh, Professor and Chief of Cardiac Surgery, Yale University School of Medicine, Yale New Haven Hospital, for his valuable suggestions in preparing the manuscript.
Financial Support
This research received no specific grant from any funding agency, commercial, or not-for-profit sectors.
Conflicts of Interest
None.
Ethical Standards
All patients gave informed consent to surgical procedures and the anonymous treatment of their data for scientific purposes.















