Atrial septal defects are the third most common type of CHD.Reference Hoffman and Kaplan1 The defect can be located at different locations in the interatrial septum or as an interatrial communication, with secundum defects being the most frequent.Reference Mori, Nishii, Tretter, Spicer, Hirata and Anderson2 Most children with an isolated atrial septal defect are asymptomatic; however, signs of the adverse effects of an atrial septal defect increase with advancing age. Indeed, patients with an atrial septal defect have increased risk of developing heart failure, a higher risk of stroke, atrial fibrillation,Reference Nyboe, Olsen, Nielsen-Kudsk and Hjortdal3,Reference Karunanithi, Nyboe and Hjortdal4 pneumonia,Reference Nyboe, Olsen, Nielsen-Kudsk, Johnsen and Hjortdal5 and a reduced life expectancy regardless of closure in childhood or adulthood.Reference Nyboe, Karunanithi, Nielsen-Kudsk and Hjortdal6,Reference Udholm, Nyboe and Karunanithi7 Consequently, patients with a repaired atrial septal defect, who for a long time were perceived as completely healthy after correction of the defect, warrant renewed attention.
We have recently shown that patients with familial atrial septal defect are subject to an increased risk of sudden cardiac death.Reference Ellesoe, Johansen, Bjerre, Hjortdal, Brunak and Larsen8 Some patients with familial atrial septal defects are carriers of a mutation in the NKX2-5-gene which is essential for the cardiac development and maturation of the atrioventricular node.Reference Pashmforoush, Lu and Chen9 Impairments of this gene lead to conduction abnormalities, in particular atrioventricular block, which ultimately may have a fatal outcome.Reference Geva, Martins and Wald10 In addition, a shunt might over years lead to dilation of the right ventricle, reduced reservoir function,Reference Vitarelli, Mangieri, Gaudio, Tanzilli, Miraldi and Capotosto11 hypertrophy of the myocardial cell and fibrosis, as well as cellular injury.Reference Geva, Martins and Wald10 The dilation stretches the myocardial fibres, thereby potentially changing the conduction of electrical impulses within the myocardium ultimately leading to atrial tachyarrhythmia or bradyarrhythmia.Reference Nyboe, Olsen, Nielsen-Kudsk and Hjortdal3,Reference Webb and Gatzoulis12
Given the potential of altered conductance of electrical impulses in the myocardium and the association between atrial septal defects and mutations in NKX2-5, we undertook this present study to investigate the clinical prevalence of atrioventricular block, bundle branch block, fascicular block, bradycardia, and pacemaker in patients with an atrial septal defect. Our aim of this study was to determine the risk of conduction disturbances compared to a healthy population and compare prevalences of conduction disturbances, mortality, and pacemaker in patients with closed atrial septal defects to patients with open atrial septal defects.
Methods
Study design
We used The Danish National Patient Registry to identify all patients born before 1994 with an International Classification of Disease diagnosis code for atrial septal defect, who were either diagnosed or treated at Aarhus University Hospital between 1977 and 2009. Hospital records were collected through an electronic hospital record system with hospital records filed since 1988. Hospital records were tracked as paper versions if they were not available in the electronic hospital record system. Diagnoses of atrial septal defects were validated by reviewing medical records by two independent physicians, whereas electrocardiograms were analysed by one investigator. The most recent electrocardiograms were identified for all included patients, and age at time of the electrocardiograms was used at time of inclusion. Consequently, we have included electrocardiograms from both children and adults with atrial septal defects. Patients were only enrolled in the study if the atrial septal defect diagnosis was confirmed by review of the hospital record. Only patients with secundum defects were included. Patients with patent foramen ovale were not included. Basic information including date of birth, age, date of surgical treatment, symptoms, prescription drugs, presence of inflammatory or autoimmune diseases was also collected through the hospital records.
Electrocardiogram
As mentioned, the most recent electrocardiograms were collected through electronic patient registry or found in paper copy in the hospital record. We selected the following criteria for the primary outcomes of the main analysis:
(1) Bradycardia defined as a resting heart rate of under 50 beats per minute.Reference Kadish, Kennedy, Knight, Mason, Schuger and Tracy13
(2) Atrioventricular block:
a. First-degree atrioventricular block defined by PR intervals >230 msReference Ove, Schaffalitzky de Muckadell and Vilstrup14
b. Second-degree atrioventricular block showing intermittent atrioventricular conduction
c. Third-degree atrioventricular block in which there is no apparent relationship between P waves and QRS complexes.Reference Ove, Schaffalitzky de Muckadell and Vilstrup14
(3) Bundle branch block and fascicular block:
a. Incomplete right bundle branch block defined as the presence of an RSR’ pattern in V1–V3 with QRS duration <120 ms
b. Complete right bundle branch block defined as the presence of an RSR’ pattern in V1–V3 with QRS duration >120 ms
c. Left anterior fascicular block defined by left axis deviation, qR complexes in leads I and aVL, rS complexes in leads II, III, and AVF, prolonged R wave peak time in aVL >45 ms together with normal or slightly prolonged QRS duration.
d. Left posterior fascicular block defined by right axis deviation, rS complexes in leads I and aVL, qR complexes in leads II, III, and aVF, prolonged R wave peak time in aVF together with normal or slightly prolonged QRS duration.
Comparison cohort
Our results were compared to two historic cohorts of healthy Belgians and Japanese. De Bacquer et al observed atrioventricular block in 0.1% healthy Belgians aged 25–54 years. Complete right bundle branch blocks were observed in 0.4% and 0.9% healthy Belgians aged 25–34 and 35–54 years, respectively.Reference De Bacquer, De Backer and Kornitzer15 Niwa et al assessed the prevalence of 1st, 2nd, and 3rd degree atrioventricular block, incomplete right bundle branch block, and complete right bundle branch block in a Japanese group of healthy children aged 5–6 and 12–13 years, respectively.Reference Niwa, Warita, Sunami, Shimura, Tateno and Sugita16 Data from these studies are shown in Tables 3 and 4.
Statistical analysis
Data were stored using REDCap™. Normally distributed, continuous results are reported as mean ± standard deviation and were compared using unpaired Student’s t-tests. Binomial data are presented as percentages and were evaluated applying χ2-test or Fisher’s exact test, if appropriate. The prevalence of all outcomes was given as numbers and percentages. A p-value < 0.05 was considered as statistically significant. All calculations were performed using STATA 15 (StataCorp LP, Texas).
Ethics
This study was approved by the Danish Data Protection Agency (j.nr. 1-16-02-633-15) and complies with the ethical standards of The Regional Committee on Biomedical Research Ethics of the Central Denmark Region.
Results
Patient characteristics
The inclusion criteria were met by 819 patients. The patients were arranged by date of birth (in date/month/year) and afterwards systematically analysed in order of this date until 412 patients were analysed. Due to missing electrocardiograms, 51 patients were excluded. Totally, 44 patients were excluded due to concomitant CHD. Further, 20 patients with sinus venosus, primum, or unknown atrial septal defect type were excluded, providing a final patient group of 297 patients (see Fig 1).

Figure 1. Flowchart detailing inclusion and exclusion selection criteria.
A total of 141 patients had an unclosed atrial septal defect (mean age: 26 years, 57% female) that was deemed haemodynamically unimportant at the time of diagnosis, and 156 patients had an atrial septal defect closed by surgery or transcatheter (mean age: 25 years, 62% female). Patient characteristics are summarised in Table 1. The majority of patients who had closure (n=156) had it performed surgically (n = 133), leaving 23 patients with catheter closure (20 Amplatzer Occluder and 3 Helex Septal Occluder).
Table 1. Baseline characteristics for population with atrial septal defect
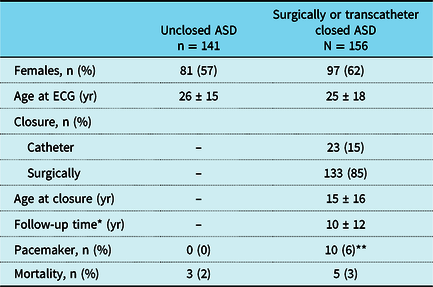
Values are presented as percentage or mean value ± standard deviation
ASD, atrial septal defects; ECG, electrocardiogram; yr, year
* Time from closure to ECG
** p-value < 0.05
Ten (3.4%) of the 297 patients with an atrial septal defect had a pacemaker. All patients with a pacemaker had received surgical correction of the defect (7 patients at an age < 16 years). All but one patient received their pacemaker years after correction of the defect. Average age at pacemaker implantation was 32 years, ranging from 5 to 70 years. Reasons for implantation were atrioventricular block (n = 6) and dysfunction of the sinoatrial node (n = 4).
Eight (2.7%) of the 297 patients with an atrial septal defect were deceased. Five of them had been through a surgical correction of the defect. All the deceased were females dying after the age of 18 years. Cause of death was obtainable for six patients with the following reasons registered: cardiac arrest (n = 2), arrythmia (n = 1), and cancer (n = 3). The patient dying from arrhythmia had a pacemaker implanted. None of the patients dying from cardiac arrest had a pacemaker implanted.
Outcome for patients with closed atrial septal defects compared to patients with open atrial septal defects
Twelve-lead electrocardiographic data for both groups are displayed in Table 2. The percentage of patients with atrioventricular block, incomplete right bundle branch block, and left anterior fascicular block was significantly higher in patients with a surgically or transcatheter closed atrial septal defect compared with patients with unclosed atrial septal defect. All patients with atrioventricular block had been through closure of their atrial septal defect. Seven patients were treated surgically while three were closed by catheter. Left anterior fascicular block occurred in nine patients with surgically or transcatheter closed atrial septal defect but only in one with an unclosed atrial septal defect. All nine patients were treated surgically. The proportion of patients with complete right bundle branch block were comparable between the two groups.
Table 2. Prevalence of rhythm disturbances in patients with atrial septal defect

ASD, atrial septal defect; AV-Block, atrioventricular block; CRBBB, complete right bundle branch block; IRBBB, incomplete right bundle branch block; LAH, left anterior fascicular block; LPH, left posterior fascicular block
Risk of conduction disturbances compared to a healthy population
In order to compare our data to already existing data, our population was stratified by age. These results are shown in Tables 3 and 4. The prevalence of different conduction disturbances varies in different age groups. In the youngest age group (5–6 years), the prevalence of 1st degree atrioventricular block, 2nd degree atrioventricular block, and incomplete right bundle branch block is higher in the group of patients with atrial septal defect compared to a healthy background population. We only had a small group of patients with an atrial septal defect in the age group 12–13 years; however, incomplete right bundle branch block still occurred in two out of five patients. Patients aged >25 years had higher prevalence of both atrioventricular block and complete right bundle branch block. The frequency of atrioventricular block was more than 60-fold increased in patients with atrial septal defect aged >25 years. In the same group, complete right bundle branch block was fourfold increased. Interestingly, the prevalence of complete right bundle branch block grew larger with age in both the background population and population with atrial septal defects.
Table 3. Age-stratified prevalence of atrioventricular block, incomplete right bundle branch block, and complete right bundle branch block, compared to prevalence in a Japanese background population. Data from background population are extracted from Niwa et al.Reference Niwa, Warita, Sunami, Shimura, Tateno and Sugita16

1-AVB, 1st degree atrioventricular block; 2-AVB, 2nd degree atrioventricular block; 3-AVB, 3rd degree atrioventricular block; ASD, atrial septal defect; CRBBB, complete right bundle branch block; IRBBB, incomplete right bundle branch block
Table 4. Age-stratified prevalence of atrioventricular block and complete right bundle branch block, compared to prevalence in a Belgian background population. Data from background population are extracted from De Bacquer et al’s study, published in 2000.Reference De Bacquer, De Backer and Kornitzer15

ASD, atrial septal defect; AVB, atrioventricular block; CRBBB, complete right bundle branch block
Discussion
In this study, we demonstrate a high prevalence of late conduction abnormalities in patients with atrial septal defect compared to a background population. Patients with surgically as well as catheter closed atrial septal defect have a higher demand for pacemaker at a later stage, a higher prevalence of atrioventricular block, incomplete right bundle branch block, and left anterior fascicular block compared to patients with small non-treated atrial septal defects.
The primary indication for closure of an atrial septal defect is symptoms and right heart volume overload. The dilation of the atrial and ventricular tissues may influence the conductive properties. Surgical incisions and inserted devices may add to the disturbances, causing a higher prevalence of conduction abnormalities. In this study, nine patients had an atrioventricular block late after closure. Whereas seven (5%) of the 133 patients with a surgically closed atrial septal defect experienced atrioventricular block and three (13%) of the 23 patients with catheter-based closure developed atrioventricular block. The higher incidence of atrioventricular block among patients with catheter closure might be due to impingement of the conductions system by the device or older age at time of closure when compared to surgically closed patients. Indeed, the prolonged timespan with an open defect and volume overload of the right heart might cause more pronounced right ventricular dilation and, potentially, a greater impact on myocardial and electrical tissue. Supportive of this finding, Asakai et alReference Asakai, Weskamp, Eastaugh, d’Udekem and Pflaumer17 found in a well-conducted retrospective study that more patients with atrial septal defects developed atrioventricular block late following catheter-based closure (4.5%) when compared to surgical closure (2.2%). It must, however, be noted that only 23 patients of our patients had catheter closure compared to 153 who underwent surgery, making any comparative conclusions difficult. Our results do, however, somewhat differ from the study by Asakai et al, as they found that only 2.2% of patients with surgical closure developed atrioventricular block. This is fewer than what was found in our study, which might reflect their shorter follow-up period and younger age at follow-up.
Ten patients needed pacemaker during follow-up, and the average age at pacemaker implantation was 32 years. Implantation of the pacemaker was, in most cases, performed several years after treatment of their atrial septal defect. Sick sinus node was the reason for pacemaker in four patients, whereas six patients had atrioventricular block as the indication. Both the sinus node and the atrioventricular bundle are anatomically at a distance from the surgical incisions, suture lines and catheter devices, and a direct trauma to the sinus node and atrioventricular bundle seems unlikely. Seven of the patients with an atrial septal defect needed a pacemaker before the age of 47 years which is remarkable as the average age at first pacemaker implantation in Denmark is 76 years.Reference Kirkfeldt, Johansen, Nohr, Jorgensen and Nielsen18 This finding might indicate an undiscovered need for follow-up in patients with atrial septal defects, as more patients may develop a atrioventricular block and pacemaker need with time.
Interestingly, our data suggest that different age groups present with different types of conduction problems. Complete atrioventricular block and complete right bundle branch block were more frequent in adults, whereas incomplete right bundle branch block was mainly present in the preschool age. This may indicate that incomplete right bundle branch block may regress or evolve into a complete right bundle branch block over time. This theory is supported by a previous study showing that people with incomplete right bundle branch block have a considerably higher likelihood of developing complete right bundle branch block.Reference Bussink, Holst, Jespersen, Deckers, Jensen and Prescott19 It must, however, be noted that the presence of an incomplete right bundle block in children is considered a normal finding and not an abnormality.
The mortality in this study (2.7%) is in accordance with other concurrent studies showing mortality at 4% after surgical closure of atrial septal defect in childhood.Reference Cuypers, Opic and Menting20 Three-quarters of our patients with repaired atrial septal defect were treated before the age of 18 years. The mortality in our study was based on the entire patient population, both those with a repaired and an unrepaired defect. However, novel studies have shown reduced life expectancy regardless of closure in childhood or adulthood.Reference Nyboe, Karunanithi, Nielsen-Kudsk and Hjortdal6,Reference Udholm, Nyboe and Karunanithi7
Study limitations
First, asymptomatic and paroxysmal conduction disturbances could be missed, leading to an underestimation of the prevalence of these disorders. A 7-day Holter recording would have provided more accurate and precise data. Second, inaccessible electrocardiograms for 51 patients could potentially bias the results. We only analysed half the patients who met the inclusion criteria. Given the random selection of these patients, we believe that this half is representative of the whole group. Further, we do not have any information on additional surgical procedures that may explain a part of the high prevalence of conduction abnormalities.
Lastly, data concerning the prevalence of conduction disturbances in a healthy paediatric background population are limited, and there is no accessible paper with data from the Danish background population, nor from an adult population. For this reason, the data used to represent a comparable background population were based on a Belgian and a Japanese study. Whether it is fair to compare to a Japanese background population is questionable as there could be some genetic or environmental variations between Danish and Japanese children, affecting the prevalence of conduction disturbances. The prevalence in a Belgian background population is stated to be as expected for a typical western European population, and therefore, most likely similar to a Danish background population.Reference De Bacquer, De Backer and Kornitzer15
Conclusion
Our results demonstrated a greater need for pacemaker implantation in patients with surgically and catheter closed atrial septal defects when compared to patients with small atrial septal defects left untreated. Further, patients with a repaired defect had a higher prevalence of atrioventricular block, incomplete right bundle branch block, and left anterior fascicular block. We have found a considerably higher prevalence of conduction abnormalities in patients with atrial septal defects compared to data from different background populations. Interestingly, our data suggest that different ages contain different types of conduction problems which may indicate that incomplete right bundle branch blocks can regress to normal or evolve into a complete right bundle branch block with time. We suggest that follow-up recommendations should not only provide information about late occurrence of tachyarrhythmias but also about increased occurrence of late bradyarrhythmias.
Acknowledgements
The authors greatly acknowledge research secretary Jette Breiner for her highly valuable contributions.
Financial support
This research received no specific grant from any funding agency, commercial, or not-for-profit sectors.
Conflicts of interest
None.
Authors’ contribution
VH, CN, and DA designed the study. ZK helped DA setting up the REDCAP database. DA analysed all patients except 80 patients, who were analysed by AO and SU. AO and SU made the statistical calculations, and tables comparing open atrial septal defects with closed atrial septal defects. DA took the lead in writing the manuscript. SU and VH aided in interpreting the results and worked on the manuscript. All authors discussed the results and commented on the manuscript.







