Truncus arteriosus is a CHD that is relatively rare counting for 2–4% of all CHDs. Reference Calder, Van Praagh and Van Praagh1 Because of the progressive nature of the disease and the inherent high mortality in untreated cases, truncus arteriosus warrants neonatal or early infancy surgical repair. Reference Bove, Lupinetti and Pridjian2,Reference Brizard, Cochrane, Austin, Nomura and Karl3,Reference Lacour-Gayet, Serraf and Komiya4 Delaying repair exposes patients to unpredictable episodes of cardio-pulmonary decompensation and increases the risk of pulmonary hypertensive disease. Reference Sinzobahamvya, Boscheinen and Blaschczok5 Previously published studies demonstrated that patients with truncus arteriosus presenting for repair beyond 3 months of age were having significant pulmonary hypertension in comparison to those who presented earlier. Reference Hanley, Heinemann and Jonas6,Reference Chen, Gao and Hua7 As such, we conducted our study aiming to evaluate in the current era our experience with truncus arteriosus repair and to investigate the differences in the early post-operative course, complications, reinterventions, and outcome between patients with late truncus arteriosus repair performed after 3 months of age and those who had an early repair within the first 3 months of life.
Material and methods
A retrospective database and chart review analysis of all patients who underwent truncus arteriosus repair at King Abdulaziz Cardiac Center , Riyadh, Saudi Arabia, during the period from February 2001 till June 2021 was conducted. The study was approved by the Institutional Review Board Committee of King Abdullah International Medical Research Center (KAIMRC), Riyadh, Saudi Arabia. All patients who underwent full repair including ventricular septal defect closure with right ventricle-pulmonary artery conduit placement in addition to pulmonary artery branches plasty or repair of associated anomalies as indicated were included. We conducted surgical repair for truncus arteriosus once diagnosis is confirmed during neonatal and early stage of infancy. However, some of our patients had late repair due to late referral, delayed diagnosis, or late presentation. As such, we divided our patients who had truncus arteriosus repair into two groups, early repair group included patients who underwent repair before 3 months of age and late repair group included patients who underwent repair at 3 months of age or later. Demographic data, associated syndromes, ICU parameters, complications, reintervention, short-term and long-term outcomes, and mortality of the two groups were compared. Echocardiographic findings at baseline, after surgery, and on the last follow-up visit were recorded, including truncal valve morphology as well as the presence of truncal valve stenosis and/or insufficiency, pulmonary hypertension assessment, pulmonary arteries stenosis, coronary artery abnormalities, atrioventricular valve abnormalities, left ventricle systolic function, and associated anomalies. Operative data, short-term, mid-term, and long-term outcomes in these patients were explored by looking for overall outcome, complications, requirement for surgical or cardiac catheterisation intervention and early or late mortality. Early mortality was defined as mortality within 30 days of operation while late mortality was defined as mortality more than 30 days after operation. Reference van Straten, Bramer and Soliman Hamad8 We included all truncus arteriosus patients who operated at King Abdulaziz Cardiac Center during the study period. We excluded patients operated outside our center and patients with hemitruncus from our study. Patients’ baseline data were taken from electronic digital records while echocardiography images and data were obtained from xcelera/Philips’s software system. Pulmonary hypertension assessment was done peri-operatively and during follow-up visits until the last recorded follow-up visit. Pulmonary hypertension assessment was done mainly using non-invasive echocardiographic criteria that include:
-
Estimation of systolic pulmonary artery pressure through the tricuspid regurgitation jet velocity measurement during continuous wave flow doppler.
-
Estimation of mean pulmonary artery pressure and end-diastolic pulmonary artery pressure through continuous wave flow doppler of the conduit regurgitation jet.
-
Pulmonary artery acceleration time.
-
Right ventricle to left ventricle diameter ratio.
-
Left ventricular eccentricity index.
-
Right ventricle and right atrium RA enlargement and inferior vena cava dilation. Reference Jone and Ivy9,Reference Augustine, Coates-Bradshaw and Willis10
Echo definition of pulmonary hypertension relied on one of the following 2 criteria; the first is estimation of systolic pulmonary artery pressure or right ventricle systolic pressure through tricuspid regurgitation velocity with measurement more than 40 mmHg in the absence of right ventricle-pulmonary artery conduit stenosis and pulmonary branches stenosis; the second is pulmonary artery pressure estimation using peak early diastolic right ventricle-pulmonary artery conduit regurgitation velocity more than 25 mmHg. Reference Jone and Ivy9,Reference Mourani, Sontag, Younoszai, Ivy and Abman11,Reference Parasuraman, Walker and Loudon12 In case of poor spectral doppler envelope to assess right ventricle systolic pressure or mean pulmonary artery pressure, we used other listed echocardiography parameters to assess pulmonary hypertension. Z score of pulmonary artery branches was obtained using previously published criteria by Cantinotti et al. Reference Cantinotti, Giordano and Scalese13
Results
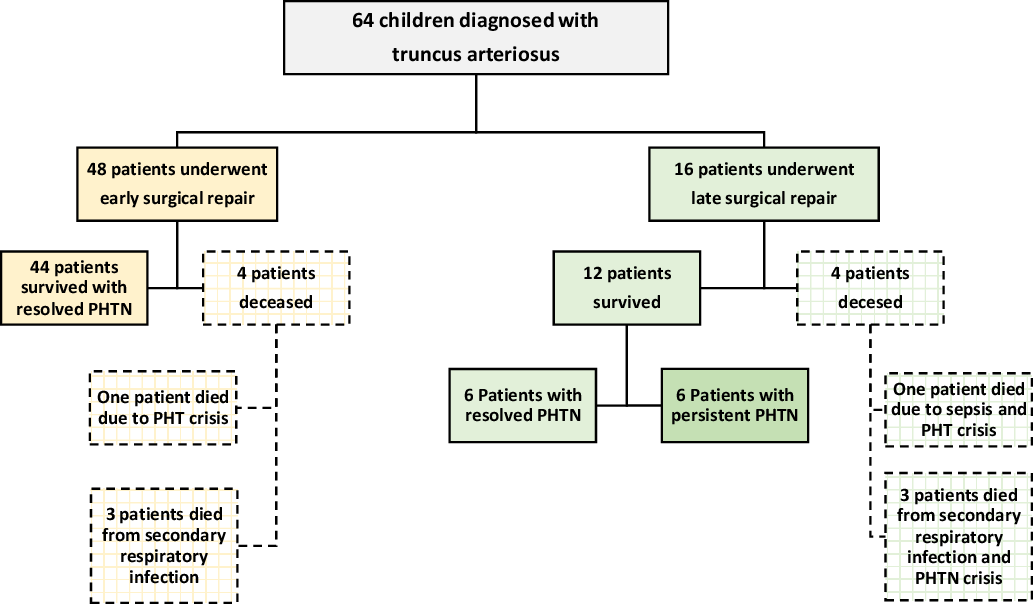
Sixty-four patients fulfilled the inclusion criteria. All of them were diagnosed by echocardiography and underwent cardiac surgery at King Abdulaziz Cardiac Center. Thirty-four (53%) were females. Early repair group included 48(75%) patients while late repair group included 16(25%) patients. Table 1 demonstrates demographic data and associated cardiac lesions. Echocardiographic data showed that 44(69%) patients had truncus arteriosus type 1, 18(28%) patients had truncus arteriosus type 2, and only 2(3%) patients had truncus arteriosus type 3 according to the classification of Collett and Edwards. Reference Collett and Edwards14 Significant truncal valve regurgitation was found in 23(36%) patients while significant truncal valve stenosis was found in 6(9%) patients. Other echocardiographic data including pulmonary hypertension assessment parameters during period of follow-up till last visit are shown in Table 2. The average age and weight at surgery in early repair group were 1.3 ± 0.9 months and 3 ± 0.5 kg, respectively, while the average age and weight at surgery in late repair group were 4.3 ± 1.4 months and 5.4 ± 2.3 kg, respectively. There was no difference in pre-operative variables in both groups as seen in Table 3. Early operative outcome demonstrated a significant pulmonary hypertension in 6(12%) patients in early repair group in comparison to 11(69%) patients in late repair group (p = 0.0001). The differences in peri-operation data for patients in with post-operation pulmonary hypertension from two groups are shown in Table 4. None of patients diagnosed with pulmonary hypertension post-surgery had anatomical obstruction such as right ventricle-pulmonary artery conduit or pulmonary artery stenosis. They were discharged with monotherapy “sildenafil” for management of pulmonary hypertension. During an average period of 61.8 ± 58 months of follow-up, all patients in early repair group had complete resolution of their pulmonary hypertension and pulmonary hypertension medications were discontinued. On the other hand, 6/16(37%) patients in late repair group continued to have evidence of persistent pulmonary hypertension during an average follow-up time of 41.5 ± 68.2 months (p = 0.0001), and hence they continue to receive mainly sildenafil for pulmonary hypertension management, Figure 1. A total of 23(36%) patients required reintervention including 22(48%) in early repair group versus 1 (6%) in late repair group (p < 0.01) as demonstrated in Table 5. These interventions were surgical in 18 patients and cardiac catheterisation interventions in 21 patients. Conduit replacement was the most frequent surgical reintervention while right pulmonary artery angioplasty was the most frequent catheterisation procedure. The average time for first reintervention was 38 ± 38.4 months in early repair group and 24 months for single patient in late repair group. 56/64(87.5%) patients survived during an average time of 56.7 ± 61 months of study follow-up. Overall mortality rate of truncus arteriosus repair was 8(12.5%) including 4(8%) patients in early repair group and 4(25%) patients in late repair group with no significant statistical difference (p = 0.19). Mortality was mainly due to pulmonary hypertension complications. All expired patients had significant pulmonary hypertension post-surgery. In early repair group, one patient died post-surgery due to pulmonary hypertension crisis, and 3 patients due to secondary respiratory infection later. In late repair group, 1 patient died due to sepsis with pulmonary hypertension crisis, and 3 patients died due to secondary respiratory infection (Fig 2).

Figure 1. Distribution of 64 paediatric children who had truncus arteriosus repiar. Comparison of pulmonary hypertension fequency between early repair and late repair groups post-truncus arteriosus repair. PHTN = pulmonary hypertension.
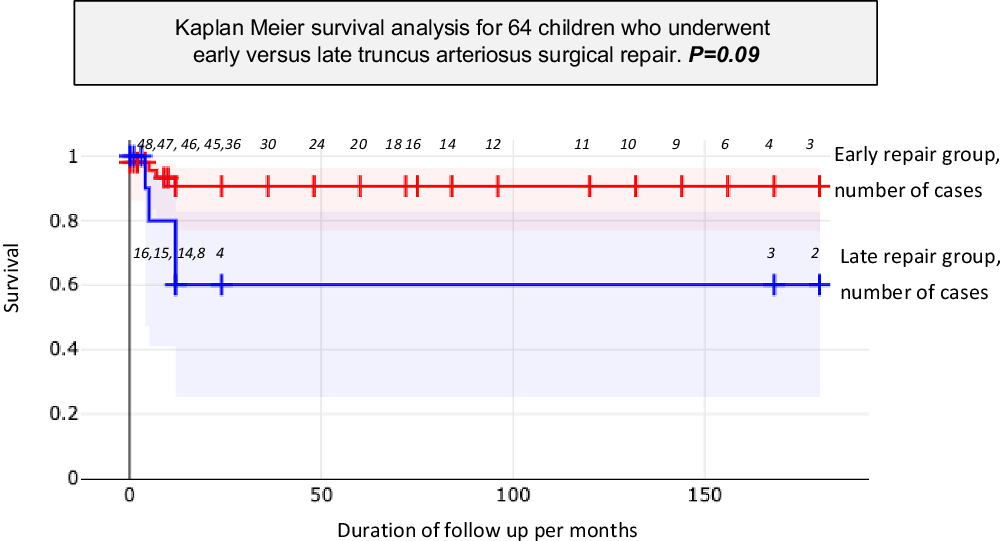
Figure 2. Kaplan–Meier survival analysis comparing 48 children who had early truncus arteriosus surgical repair versus 16 children who had late repair.
Table 1. Characteristics, associated anomalies, intraoperative, and postoperative data of 64 children who underwent truncus arteriosus repair. Continuous variables are presented as mean ± standard deviation and categorical data as number and percent

Table 2. Echocardiography data at baseline and at last follow-up visit of 64 children who underwent truncus arteriosus repair

Table 3. Post-operative outcomes of 64 children who underwent truncus arteriosus repair

Table 4. Characteristics, associated anomalies, intraoperative and postoperative data for patients who underwent truncus arteriosus repair and had post-operation pulmonary hypertension. Continuous variables are presented as mean ± standard deviation and categorical data as number and percent

Table 5. Details of catheter and surgical interventions performed in 64 children who had truncus arteriosus repair with comparison between early repair group versus late repair group

LPA = left pulmonary artery; LV = left ventricle; PAs = pulmonary arteries; RPA = right pulmonary artery; RVOT = right ventricle outflow.
Discussion
truncus arteriosus is a complex congenital cardiovascular malformation. Patients with associated anomalies such as interrupted aortic arch, truncal valve incompetency, or single pulmonary artery are particularly at high risk for early death. Even without additional lesions, patients with unrepair truncus arteriosus can still have poor prognosis due to progressive pulmonary vascular disease or left ventricular failure. Reference Mair, Sim, Danielson and Puga15 The current trend is toward decreased palliative procedures accompanied by a younger age at truncus arteriosus repair. Reference Swanson, Selamet Tierney, Tworetzky, Pigula and McElhinney16,Reference Hoashi, Kagisaki, Oda and Ichikawa17 Operative correction of truncus arteriosus is now possible with low mortality during neonatal and early stage of infancy. The corrective surgery to repair truncus arteriosus is now the standard approach to relieve the large left ventricular volume load and its bad effects on the left ventricular function, as well as to minimise the risk of irreversible pulmonary vascular obstructive disease. Reference Mair, Sim, Danielson and Puga15 Reviewing the literature, Chen et al conducted a retrospective study included 50 patients with truncus arteriosus, 20 of them underwent early surgical repair below 1 year of age compared to 30 patients who underwent late surgical repair beyond 1 year of age. Reference Chen, Gao and Hua7 Invasive assessment of pulmonary hypertension and pulmonary vascular resistance were done for all patients before surgery, they found that mean pressure was higher in truncus arteriosus patient presented beyond 3 months of age compared to those presented before 3 months of age. However, there was no statistically significant changes in pulmonary vascular resistance between both groups and comparable post-operative outcome variables between two studied groups. In our study, we reviewed 64 patients and found a significant pulmonary hypertension in late repair group post-surgery in comparison to early repair group. Like Chen et al study, we observed no statistical difference in post-operative variables and mortality rate between early and late repair groups except for presence of pulmonary hypertension. Furthermore, Hanley et al conducted a study that included 63 children with truncus arteriosus. They described 41/63 patients who had simple truncus arteriosus without associated lesions. They reported 33/41 patients who underwent early repair before age of 100 days and 8 /41 patients who underwent late repair beyond age of 100 days. The authors reported 2(25%) patients died in late repair group due to unresolved pulmonary hypertension with nil mortality in early repair group. Reference Hanley, Heinemann and Jonas6 In our study 25% of our patients had late repair with an overall mortality of 12.5% including 4/48(8%) patients in early repair group and 4/16(25%) in late repair. The main causes for mortality post-repair were related to pulmonary hypertension. Hanley and his colleagues found in their study that pulmonary hypertension was statistically higher in patient with truncus arteriosus who had correction at 30 days of age or later compared to those who had correction before 30 days of age. Similarly, we found in our study that pulmonary hypertension was higher in patients who had late repair with p value of 0.0001. In another published study, the authors reported 33 patients with late truncus arteriosus presentations with mean age of 3 years at surgery. 30% of patients had significant post-operative pulmonary hypertension with one early mortality (3%) and one late mortality (3%) 6 months post-repair. Reference Gouton, Lucet, Bical and Leca18 In our study, 16 patients with late truncus arteriosus presentation underwent surgery at mean age of 5 months, 11(69%) of patients had significant pulmonary hypertension while no patients died within 30 days post-surgery. However, late mortality happened in 25% of patients due to unresolved pulmonary hypertension. Arslan and his colleagues reported 7 patients with truncus arteriosus who underwent repair beyond 1 year of age with no early or late mortality. They reported two patients (28%) complicated with pulmonary hypertension and no patients required reintervention during an average of 214 ± 59 days of follow-up. Reference Arslan, Ugurlucan and Yildiz19 In our study 22 patients (34%) in early repair group required reintervention and one from late group (3%) needed reinterventions twice, first reintervention was pulmonary arteries balloon dilatation and the second one was right ventricle-pulmonary artery conduit replacement with pulmonary arteries plasty. It is possible that the larger population group and longer follow-up time contribute to high percentage of patients requiring reinterventions in our study.
Limitations
Our study is an observational study which reflects a single-center experience. It includes a small number of cases with late truncus arteriosus repair, that needs to be generalised to a larger population. Birth weight and gestational age were missing from our patient records, and hence, their effects on development of persistent pulmonary hypertension after truncus repair should be further evaluated in future studies. Pulmonary hypertension assessment done by echocardiographic which is less accurate than invasive methods. Furthermore, late repair group had higher number of patients with truncus arteriosus and associated cardiac anomalies in comparison to early repair group (p = 0.0001) that may be an association rather than causation. In the management of long-term pulmonary hypertension after repair, only monotherapy was used for pulmonary hypertension management. It is possible that combination therapy may have different result. The use of multiple drugs to treat persistent pulmonary hypertension requires further study and evaluation.
Conclusion
Early repair of truncus arteriosus is a standard approach with a good outcome. For late-presenting cases, truncus arteriosus repair can be carried out in late infancy with some risk of complications. Most of patients who underwent their first surgery at age more than 3 months were complicated with pulmonary hypertension comparing to those who were operated at age less than 3 months. Careful follow-up is essential as patients with truncus arteriosus may experience persistence of pulmonary hypertension or right ventricle-pulmonary artery conduit stenosis requiring reintervention. Almost one-third of the patient will require reintervention within 3 years after repair.
Acknowledgements
None.
Financial support
None.
Conflict of interest
None.
Ethical standards
The study was approved by King Abdullah International Medical Research Center (KAIMRC) with IRB NCBE registration no. H-01-R-005.