Background and justification
In 2012, the American Heart Association, in conjunction with the American Academy of Paediatrics, released a scientific statement with guidelines for the evaluation and management of the neurodevelopmental needs of children with CHD. Reference Marino, Lipkin and Newburger1 Following decades of tremendous advances in reducing CHD-related mortality, Reference Khairy, Ionescu-Ittu, Mackie, Abrahamowicz, Pilote and Marelli2–Reference Marelli, Miller, Marino, Jefferson and Newburger4 this milestone achievement marked a tidal shift in paediatric cardiology – a new era dedicated to understanding longer range outcomes and maximising the neurodevelopmental potential of millions of individuals affected by CHD.
Towards that ultimate goal, the 2012 American Heart Association and the American Academy of Paediatrics scientific statement Reference Marino, Lipkin and Newburger1 made two crucial steps. First, to more clearly delineate the developmental risks associated with CHD, they conducted a comprehensive review of the available literature. This review highlighted a range of cognitive, learning, motor, and psychosocial vulnerabilities affecting individuals with CHD across infancy, childhood, adolescence, and early adulthood. Second, they proposed management strategies, building upon the American Academy of Paediatrics “medical home” model, and provided guidance on periodic neurodevelopmental surveillance, screening, evaluation, and re-evaluation for the purposes of early identification and treatment. As a result, the number of institutions with cardiac neurodevelopmental Follow-Up Programmes and services for CHD is now growing worldwide.
With respect to the neurodevelopmental evaluation of school-age children with CHD, which is the focus of the current paper (also see infant-preschool recommendations in Ware and colleagues), the American Heart Association and the American Academy of Paediatrics scientific statement Reference Marino, Lipkin and Newburger1 recognised the importance of going beyond broad-based measures of general cognitive functioning (i.e., intelligence quotient) to gain an accurate understanding of an individual child’s ability profile. Developmentally appropriate evaluation of cognitive/intellectual, language/verbal, visual–spatial/perceptual, attention, executive function, speed of processing, memory, motor, academic, and adaptive skills, as well as psychosocial and behavioural adjustment, was recommended. A list of standardised rating scales, test batteries, and a few particular tests that had been used in research studies of children/adolescents with CHD was also provided; however, recommendations about specific evaluation strategies were not provided.
In this manuscript, we present an expanded set of neurodevelopmental evaluation strategies and considerations for professionals working with school-age children with CHD both in clinical and research capacities. These recommendations and associated assessment batteries are the product of many years of collaboration amongst clinicians and specialists from across North America and Europe, including experts in psychology, neuropsychology, cardiology, nursing, neurology, rehabilitation, and education. Many of these professionals are currently integral members of Cardiac Neurodevelopmental Follow-Up Programmes. The call for more specific neurodevelopmental evaluation strategies began in 2012 after the first annual Cardiac Neurodevelopmental Symposium. Following this symposium, separate working groups were developed to address needs specific to children such as ages birth – five years, school-age children, and to facilitate cross-site research collaborations. Working groups met subsequently via conference calls and in-person at annual Cardiac Neurodevelopmental Symposium meetings to update recommendations and goals.
Collaborations over time culminated with the formal incorporation of the Cardiac Neurodevelopmental Outcome Collaborative in 2016, and the continuation of an annual conference, now named as the Cardiac Neurodevelopmental Outcome Collaborative Annual Scientific Sessions. The Cardiac Neurodevelopmental Outcome Collaborative is a not-for-profit organisation created to determine and implement best practices of neurodevelopmental services for individuals with paediatric and CHD through clinical, quality improvement, and research initiatives. The proposal to publish assessment battery recommendations was in response to repeated requests for clinical guidance from a number of providers developing new programmes with the CHD population and coincident with the creation of the Cardiac Neurodevelopmental Outcome Collaborative. In addition to these recommendations regarding school-age neurodevelopmental evaluation strategies, a parallel statement is also available regarding evaluation strategies between infancy to age 5 years (Ware and colleagues, this journal edition). For the 5-year-old child specifically, the examiner should select either the 0–5 or 5–21 core assessment battery based on the timing of the child’s kindergarten enrolment and his/her overall developmental abilities. For additional background on CHD and implications for assessment, interested readers are encouraged to read a review about neuropsychological and outcomes in CHD. Reference Cassidy, Ilardi and Bowen5
Semantics surrounding neurodevelopmental care
A note on relevant terminology: as mentioned above, the American Heart Association and the American Academy of Paediatrics scientific statement Reference Marino, Lipkin and Newburger1 proposes a tiered model of surveillance, screening, and evaluation, as indicated by need/risk status, for individuals with CHD. The primary aim of the first tier, surveillance (i.e., “universal monitoring”, but also see the model of prevention-based care) Reference Hardy, Olson, Cox, Kennedy and Walsh6 , is to monitor developmental progress and document risk factors amongst all children with CHD. This is typically performed by the child’s primary care and cardiology team(s), often in conjunction with each office visit, and relies on clinical interview and perhaps some short, repeatable questionnaires to elicit information and concerns from parents. For those children identified as at-risk on account of either their specific cardiac diagnosis or concerns identified via surveillance, referral for screening is indicated. Screening (second tier) can include the administration of standardised, psychometrically sound rating scales and/or brief performance-based tests that may ultimately support the need for more comprehensive evaluation. In the case of parent rating scales or questionnaires, many can be administered and scored by a member of the medical team with minimal training in this area. Information from the screening instruments has the potential to provide stand-alone evidence to support the initiation of intervention in some cases. Evaluation is the highest tier in the model, and unlike surveillance and screening, must be performed by a professional – most often a psychologist or neuropsychologist – with specialised training that can be brought to bear in conceptualising the child’s full profile of strengths and weaknesses and, when appropriate, assigning a developmental and/or behavioural diagnosis to inform treatment and access to resources. A screening or evaluation should take place at specified ages or when concerns arise.
In our experience, there can be confusion regarding the differentiation of psychological, neuropsychological, developmental/neurodevelopmental, and psychoeducational evaluation/assessment. Regarding the distinction between psychology and neuropsychology, a paediatric neuropsychologist is a clinical psychologist who has additional specialised training in brain development, structure, and function – particularly within the context of medical and other central nervous system-implicating conditions – which he or she then applies to understand how a child thinks, learns, and behaves. Psychologists and neuropsychologists may choose to administer the same tests in their respective evaluations. By virtue of their specialised training, neuropsychologists are able to make observations and interpret performance patterns through the lens of brain–behaviour relationships, which can be particularly helpful when working with individuals whose brain development has been affected by medical conditions such as CHD. Some psychologists also have training in brain–behaviour relationships. The term developmental (or neurodevelopmental) evaluation is used most often to describe the evaluation of early cognitive, language, motor, social, and self-regulatory capacities in an infant or preschool child who has not yet reached school age. This type of evaluation may be performed by a psychologist, neuropsychologist, or other appropriately trained clinicians such as a developmental paediatrician. However, in clinical settings (and research samples) working with paediatric CHD, the term “neurodevelopmental” is commonly used regardless of the age of the child. The prevalent use of this term is likely because the earliest outcome research in CHD was with infants and preschool children, which then influenced terminology used for follow-up studies with school-age children. In other cases, it could be used to describe an evaluation by a developmental paediatrician into the adolescent years. A psychoeducational evaluation is a targeted (i.e., not comprehensive) assessment, typically (although not exclusively) performed by the school or a (neuro)psychologist, that aims to establish a child’s intellectual ability and academic competencies. A neuropsychological evaluation is a more comprehensive evaluation of a variety of skills (including intellectual skills, attention/executive skills, learning and memory, language, visual–spatial/visual–motor, fine motor, emotional/behavioural functioning) that is then interpreted through the lens of brain–behaviour relationships, which can be particularly helpful when working with individuals whose brain development has been affected, such as in CHD. Reference Schmithorst, Panigrahy and Gaynor7–Reference McQuillen, Goff and Licht9 This type of evaluation is conducted by a paediatric neuropsychologist. For the purpose of consistency amongst the providers and researchers in the communities of those who work with paediatric CHD, “neurodevelopmental” evaluation will be used throughout the current paper.
Referral process and access to evaluations
There are several possible ways to access providers who can complete an evaluation of the school-age child with CHD. The first is through a formalised Cardiac Neurodevelopmental Follow-up Programme. Many institutions have developed a formal Cardiac Neurodevelopmental Follow-up Programme with more than three dozen around the world being members of the Cardiac Neurodevelopmental Outcome Collaborative at the time of this paper and many others having informally followed high-risk children with CHD for years. The pathways to refer children vary across centres based on resources. Some centres have protocols or specified referral criteria, such as for children with single-ventricle physiology. Some sites refer based on the criteria for risk outlined in the 2012 American Heart Association and the American Academy of Paediatrics scientific statement, including CHD severity but also medical comorbidities such as prematurity, neurological abnormalities, and genetic disorders. Reference Marino, Lipkin and Newburger1 Referrals can also be made based on suspected, observed, or parent/teacher-reported concerns about developmental, academic, or social/emotional concerns. Across Cardiac Neurodevelopmental Follow-up Programmes, the funding (grant and donor funds) and insurance coverage for evaluations vary widely and this also influences the types of referrals made, volume of patients, and length of evaluations. Cardiac Neurodevelopmental Follow-up Programme referrals are often made by the cardiologist, but they are also made by other physicians and providers within the child’s medical team. Parents or family members occasionally self-refer after learning about a Cardiac Neurodevelopmental Follow-up Programme through social media or parent networks. At some sites, patients are referred to neurodevelopmental programmes for other medical populations, such as a neonatal intensive care unit follow-up programme.
For families of patients who do not have access to a Cardiac Neurodevelopmental Follow-up Programme, there are also providers in the communities or schools who can complete an evaluation. One option is for the family to request an evaluation through the school system. In the United States, families have a legal right to request an evaluation through the school at any time if there are academic problems. However, a school-based evaluation may be associated with time delays, may include only a limited number of testing instruments, and are typically limited only to those concerns that directly impact a child’s ability to access their curriculum. Reference Resch, Mireles, Benz, Grenwelge, Peterson and Zhang10–Reference Silver, Tröster and Reynolds12 Alternatively, a referral to a community-based child psychologist who completes psychological testing for learning problems can be made. In such cases, it is essential that the family work closely with their insurance company to ensure they are aware of their benefits and how to decrease any financial burden. It is also important to note that, depending on the psychologist’s expertise, this evaluation may be limited with respect to the testing measures and interpretation of the findings in the context of the child’s medical history. In other words, this psychologist may not have neuropsychological training to recognise specific patterns of strengths and weaknesses that are not typically seen in non-medical populations, for example, constellations of deficits that are consistent with a history of stroke.
For school-age children with CHD, referral to a Cardiac Neurodevelopmental Follow-up Programme is preferred over referrals in the community for a number of reasons. Multidisciplinary collaborations that are common amongst Cardiac Neurodevelopmental Follow-up Programme sites can help support collaborative care and access to resources. The providers within a Cardiac Neurodevelopmental Follow-up Programme are trained to understand neurocognitive and psychosocial issues common in the CHD population specifically and are often involved in research with the CHD population. This allows for interpretation of findings within the context of any risk factors in the child’s history (e.g., long hospital stays, type of CHD, and sub-threshold symptoms of a diagnosis that needs an intervention). Many Cardiac Neurodevelopmental Follow-up Programme sites have had successful experiences with insurance coverage or funding for evaluations, which reduces the financial burden on the family.
Evaluating the school-age child
The evaluation of the school-age child with CHD includes multiple sources of information and careful clinical considerations, all of which are described in detail below. Sources of information include a detailed history and background that is gathered from medical records, school records, and family. A recent medical and/or neurological evaluation is critical. Behaviour rating scales are obtained from parents, teachers, and the child/adolescent, and these ratings are compared to what is typical in the normative population. In addition, behavioural observations of the child are collected during structured (i.e., testing activities) and unstructured contexts (e.g., waiting room, information conversation, and rarely in classroom/therapy settings). Finally, the child participates in the objective, standardised testing that is interactive, highly structured, and psychometrically sound. Scores are compared to those of typically developing children the same age (i.e., age-based normative data) and gender (i.e., for behaviours that vary by gender, such as anxiety and hyperactivity). These sources of data are integrated to evaluate an overall profile of strengths and weaknesses that can be explained by risk (e.g., prematurity, severe heart disease, history of stroke) and protective factors (e.g., parental employment/education, absences of surgical complications), to provide diagnoses as appropriate, and to develop a treatment plan and specific recommendations for the family and school professionals. Families may also be provided with information about long-term prognosis (e.g., intellectual disability) or possible problems to monitor in the coming years (e.g., early signs of a learning disability, attention disorder, or anxiety symptoms prior to critical transition points in typical child development). As appropriate, feedback about test results and recommendations are shared directly with the child or adolescent as well.
Medical factors
A medical evaluation is a key component of the neurodevelopmental assessment in this population. Multiple medical risk factors begin in utero and accumulate over the lifespan to influence neurodevelopment in children with CHD. These factors are well described in the 2012 American Heart Association and the American Academy of Paediatrics scientific statement Reference Marino, Lipkin and Newburger1 and elsewhere, Reference Volpe13 thus only briefly updated herein. The increasing availability of next-generation genetic sequencing has led to greater recognition of the role of genetics in neurodevelopmental outcomes. Genetic abnormalities are found in up to 50% of children with syndromic CHD, and even in those with isolated, sporadic CHD, whole-exome sequencing reveals de novo deleterious mutations in 10% of children. Reference Zaidi, Choi and Wakimoto14,Reference Homsy, Zaidi and Shen15 Children with CHD and genetic or extracardiac anomalies consistently score lower on neurodevelopmental assessments than those without. Reference Gaynor, Stopp and Wypij16–Reference Bellinger, Watson and Rivkin18
Foetal haemodynamic influences have also garnered increasing attention, with recent foetal MRI studies indicating smaller brain volumes and dysmature cortical folding as early as 30 weeks gestation, particularly in those foetuses with reduced cerebral oxygen/nutrient delivery such as those with reduced or lacking antegrade aortic arch flow. Reference Limperopoulos, Tworetzky and McElhinney19–Reference Kelly, Makropoulos and Cordero-Grande23 Brain dysmaturity increases the risk of white matter injury, which is known to occur in about 15–40% of children with CHD even prior to surgery. Reference Beca, Gunn and Coleman24 Stroke or haemorrhage may also occur, either in the perinatal, preoperative, or post-operative period. Reference Dehaes, Cheng and Buckley25–Reference Birca, Vakorin and Porayette27 Even in children who do not have any overt evidence of brain injury, smaller brain volumes, abnormal white matter microstructure, and differences in cerebral connectivity Reference Schmithorst, Panigrahy and Gaynor7 are seen in adolescence. These abnormalities have all been linked to neurodevelopmental outcome. Reference Schmithorst, Panigrahy and Gaynor7,Reference von Rhein, Buchmann and Hagmann8,Reference Rollins, Watson and Asaro28,Reference Rollins, Asaro and Akhondi-Asl29
Medical evaluation of children with CHD depends upon the presenting symptoms but should always include: (1) a detailed history including medical, developmental, family history, and psychosocial concerns; (2) assessment of dysmorphology that may be associated with underlying genetic conditions; (3) a neurological examination to identify subtle signs of brain injury or abnormality; and (4) neuroimaging where appropriate. In obtaining the history, particular attention should be paid to issues such as early developmental delays that may increase the risk of subsequent learning difficulties, medical factors such as cardiac complexity, complications, and length of stay, and family history of learning difficulties. Attention, anxiety, and behavioural regulation should be considered as they are common concerns in the CHD population which may merit medication management in conjunction with psychological treatment strategies. Genetic evaluation may include targeted testing based on a child’s phenotype, a chromosomal microarray, or whole-exome sequencing. While performing a complete neurological examination, particular attention should be directed to the motor exam including subtle neurological signs that may be associated with learning disabilities and behavioural problems in school-age children and adolescents, such as motor planning difficulty. Reference Liamlahi, von Rhein and Buhrer30 Examination may include timed motor testing, gestural imitation, and stress gait manoeuvres. Some centres routinely perform neonatal preoperative and/or post-operative brain MRI, which may demonstrate overt signs of injury or more subtle abnormalities and have implications for medical evaluation and treatment. In those children who do not receive a routine neonatal brain MRI, seizure history or overt abnormal findings on the neurological examination should prompt consideration of possible brain MRI. However, the challenges of obtaining a brain MRI for some children (e.g., anxiety, hyperactivity, and possible need for sedation) also need to be considered. In those children where brain MRI could be obtained, findings may indicate the need for a change in clinical management, provide prognostic information for families, or allow insight into potential cognitive vulnerabilities that may need to be assessed in greater detail in the neuropsychological evaluation.
While the medical evaluation may be completed by a variety of professionals, it is most often conducted by a developmental–behavioural paediatrician, neurologist, or specially trained nurse practitioner. A team-based approach is essential to ensure that all providers are fully aware of the presenting concerns and psychosocial contributors, to contextualise these concerns within the child’s medical history, and to support effective communication with families and schools including coherent and integrated treatment recommendations. The medical evaluator also collaborates closely with a child’s cardiologist and medical home provider. Findings from the most recent medical examination and neurological report should be incorporated into the conceptualisation and recommendations of the neurodevelopmental evaluation.
Clinical interview with the family
The clinical interview with the family is a critical source of information. An interview provides information that can be used to plan the upcoming evaluation of the child, namely the symptoms of concern, reason for referral, and background information (e.g., pregnancy/birth issues, developmental milestones, medical history, and educational history). Information should be obtained about access to resources and services, obstacles to obtaining these, and consideration should be made for the impact of socio-economic factors. The interview is also an opportunity to begin to provide education to the family about current outcome research in children with CHD and how it may help explain concerns. Review of school records can help the examiner see what and how current services are implemented, and how the child is performing in the classroom. The findings of recent psychoeducational testing reports can be compared to those from the current assessment. Similarly, the review of clinical therapy notes can help identify goals related to areas of impairment and consultation with any outside psychologists or counsellors who can identify relevant questions or concerns as well. The clinical interview is typically conducted as an integrated part of the evaluation with a psychologist, but in some multi-disciplinary clinics, the information could be gathered by an interview from multiple healthcare providers (e.g., social worker, school teacher, and school intervention specialist).
Selecting assessment measures
A number of factors contribute to the decision about which tests to include in the assessment battery. The reason for referral is an essential first consideration for the examiner. Reasons to evaluate a school-age child with CHD can include school readiness, baseline evaluation for an at-risk child, measuring the change in function after a stroke, re-entering school after a critical event (e.g., transplantation), documenting deficits to gain access to services or provide treatment planning, maintaining or updating already existing services, clarifying a potential diagnosis of concern (e.g., attention-deficit/hyperactivity disorder, autism spectrum disorder), or monitoring change and progress across development at critical stages. The results of the evaluation need to be considered in the context of previous evaluations. For some referrals, the examiner will be free to select testing measures and may want to assess all domains of function comprehensively. However, in some situations, there are factors that limit or influence the type of measures selected. For example, in children who are non-verbal, globally developmentally delayed, or have a known intellectual disability, the test battery will be brief and will assess only skills expected for their abilities. In children with sensory or motor impairments, the test battery might need to be modified (e.g., for visual impairments, emphasis placed on auditory/verbal measures). For rating scales given to family members, it is appropriate to inquire about whether help is typically needed to read questionnaires, which may result in the need to use reduced or simplified rating scales for parents. Caregivers may also prefer that rating scales be provided in their first language, if available. Finally, insurance companies may limit the amount of time approved for patient care, or the ability to administer specified test measures (e.g., academic measures may not be approved); thus, a brief or modified test battery may be required. They may also deny evaluations for purposes not deemed medically necessary (e.g., monitoring development, school readiness).
English as a second language
Evaluation of bilingual children is challenging and fraught with controversy. See an alternative resource for details and practical considerations when assessing bilingual patients. Reference Rivera Mindt, Arentoft and Kubo Germano31 Briefly, there is an expectation that bilingual children lag behind monolingual peers in language development; however, this is an oversimplification, and may lead to under-referral and under-identification of bilingual children who need additional support. Given that lexical–semantic systems are distributed across two languages, consideration of a child’s combined linguistic skills is important. Along these lines, approaches that assess a child in both languages have been found to more accurately classify bilingual children with language impairment. Reference Pena, Bedore and Kester32 In addition to considering relative exposure to and use of each language, clinicians must consider parental characteristics and socio-economic factors that have a significant impact on language development and may further impact testing. Reference Hammer, Komaroff, Rodriguez, Lopez, Scarpino and Goldstein33 Finally, it is also important to consider that some measures may be more vulnerable to the effects of bilingualism (e.g., retrieval tasks, given frequency of use in each language and interference), Reference Gollan, Montoya, Cera and Sandoval34 though others may not be impacted (e.g., list learning tasks). Reference Gasquoine, Croyle, Cavazos-Gonzalez and Sandoval35 Given the complex factors used to determine how to evaluate the bilingual child, referring providers of children with CHD need to work closely with local neurodevelopmental providers to determine the best clinical approach. When a Cardiac Neurodevelopmental Follow-up Programme does not have a bilingual psychologist or neuropsychologist, there will likely be a referral process to local bilingual providers who can complete an evaluation (e.g., community/school psychologist, speech/language therapist).
Timing of evaluations
Children with CHD do not experience a single neurological insult; instead, there are combinations of “developmental and destructive” influences over the course of development described in more detail above. Reference Volpe13 In fact, research suggests that a larger proportion of children require support over time. Reference Bellinger and Newburger36 Children with CHD may “grow into” certain patterns of strengths and weaknesses as developmental expectations change over time, and weaknesses in higher order skills may emerge even in the absence of early delays (or after early delays resolve). Thus, repeated assessment of neurodevelopmental skill areas is strongly recommended to provide, and regularly updates, recommendations for treatment. Reference Heilbronner, Sweet, Attix, Krull, Henry and Hart37
Recommendations regarding the frequency and timing of re-evaluations should take into consideration environmental stress points, or periods where expectations in a child’s environment change dramatically. These align with key periods in neurodevelopment, which can vary across cognitive and behavioural dimensions. This approach is consistent with the National Institutes of Health Research Domain Criteria approach, Reference Insel38 which highlights the importance of monitoring shared skill areas that are vulnerable across formal diagnoses found regularly in our population (such as attention-deficit/hyperactivity disorder, learning disorders, or autism spectrum disorder). A key to this approach is understanding that (1) neurodevelopmental trajectories can be non-linear, and thus have periods of accelerated progress (e.g., developmental “leaps”), (2) there are sensitive periods for both development and intervention in key skill areas, and (3) development of skill areas is intertwined, such that disruptions in one skill area can influence the development of another set of skills, a concept known as a developmental cascade. Reference Casey, Oliveri and Insel39 The development of executive function, a key area of vulnerability in CHD, exemplifies this well. There are a variety of executive skills domains, which develop in a non-linear fashion, with key periods of accelerated growth that align with maturational changes in frontocortical networks in the brain. Reference Anderson40 In addition, executive skills are vulnerable across populations and diagnoses, such as attention-deficit/hyperactivity disorder, autism spectrum disorder, or psychiatric conditions. Weaknesses in executive skills can impact multiple domains of functioning. Finally, in CHD, early weaknesses in executive skills may be a part of a developmental cascade that influences later academic success and emotional/behavioural adjustment. Reference Cassidy, White, DeMaso, Newburger and Bellinger41,Reference Cassidy, White, DeMaso, Newburger and Bellinger42
Developmental transition points
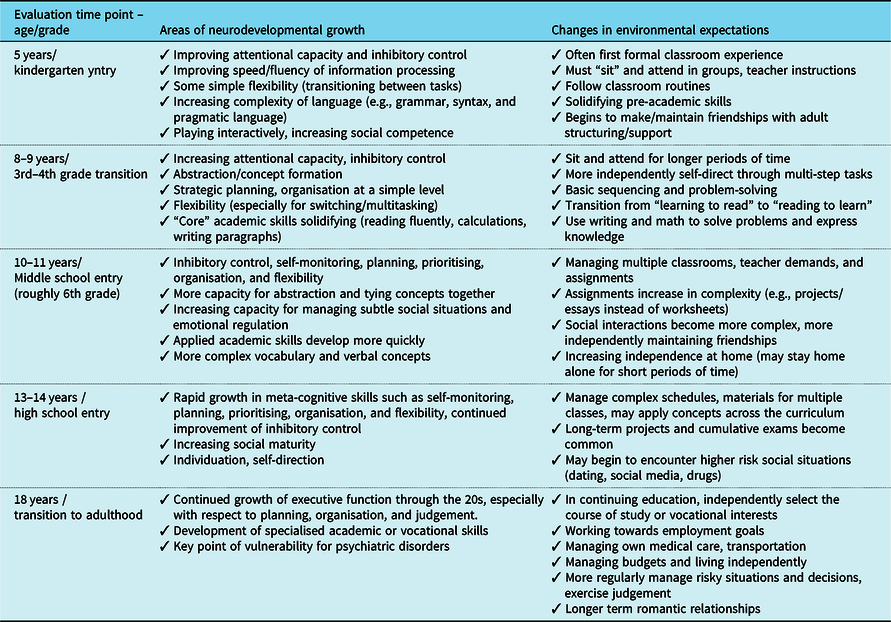
With the above theoretical frameworks and clinical guidelines in mind, key time points for re-evaluation of children with CHD are outlined in Table 1. The reader is also referred to a previously published patient page, Reference Brosig, Butcher and Ilardi43 which provides practical, “real world” examples of what potential difficulties may look like in day-to-day life at various stages in development. This can be a helpful resource to share with parents when explaining the need for serial assessment. As noted above, for the 5-year-old child specifically, the clinician should select either the 0–5 (Ware and colleagues, this journal edition) or 5–21-year core assessment battery (Table 2) based on the timing of the child’s kindergarten enrolment and his/her overall developmental abilities. For 5-year-old children who are not yet in kindergarten and/or children whose anticipated level of overall cognitive ability is well below age expectations, the 0–5-year battery may be more appropriate. For 5-year olds not falling within either of these categories, the 5–21-year battery would likely be more appropriate.
Table 1. Critical time points for serial evaluation of school-age children with CHD. Of note, these are the minimum number of recommended evaluations in children with identified difficulties, more frequent re-evaluation will likely be recommended
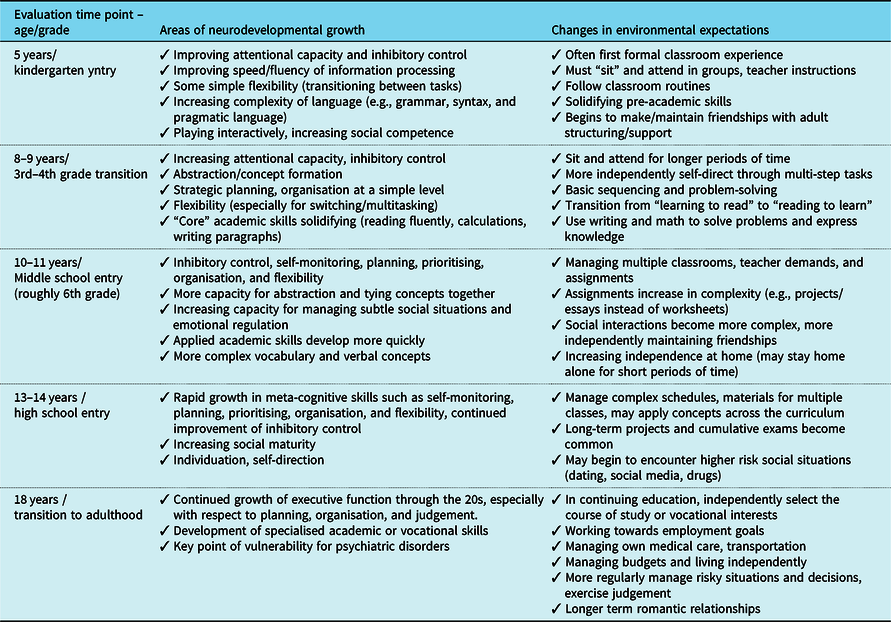
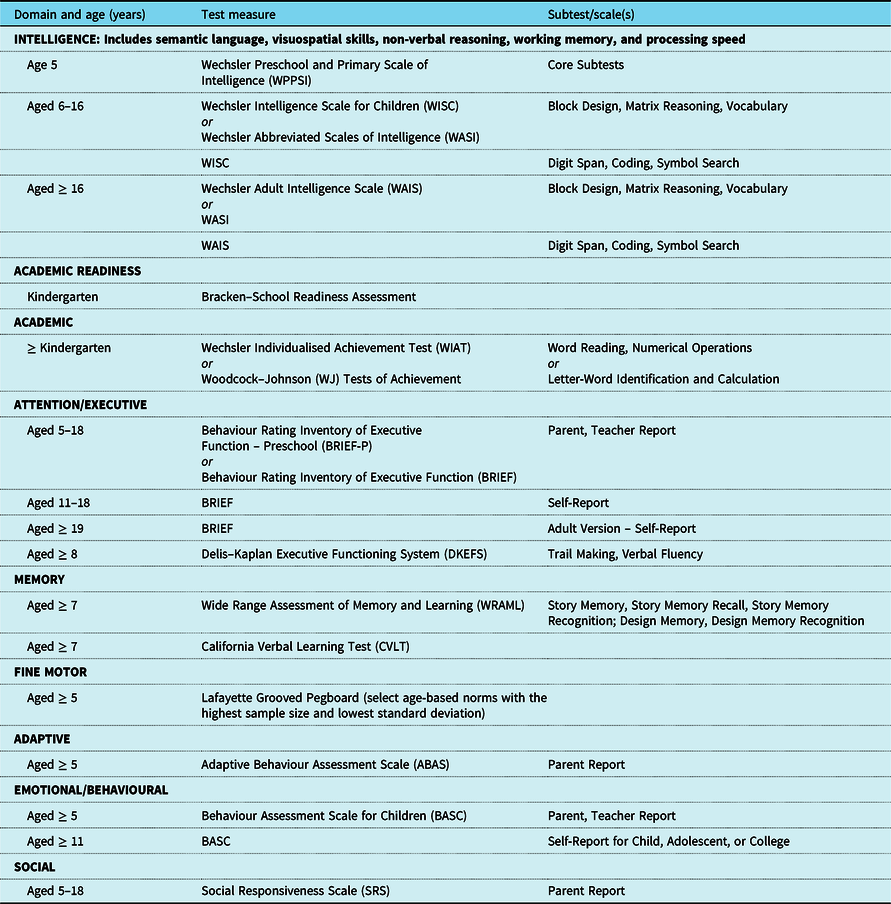
Table 2. Core assessment battery for a brief evaluation of school-age children (aged 5 to young adult) with CHD

Please note that the core assessment battery is a current recommendation; examiners should carefully consider clinical, cultural, and ethical factors to adjust the battery as appropriate. The most recent test version and age-based norms are recommended. Some tests/rating scales are available in multiple languages; see details from the test publisher as this is continually updated based on revisions. For an extended list of additional clinical measures that would allow for a comprehensive assessment, see Table 3
Domains to be evaluated
Given the extent of variability in the neurodevelopmental profile of the school-age child with CHD, as well as the multiple factors that contribute to this variability, patterns of strengths and weaknesses can occur both within and across domains. Reference Cassidy, Ilardi and Bowen5,Reference Latal44 A comprehensive assessment across domains should be completed, especially for baseline testing or after an event that increases the risk of neurological change (e.g., open-heart surgery, documented stroke, or seizures). New areas of assessment within a given domain may be added as development progresses (e.g., executive functioning, memory). Below is a review of domains that should be considered for evaluation, and this is followed by core (Table 2) and extended assessment battery (Table 3) recommendations. It is important to note that these recommendations relate to English-speaking countries or countries where the suggested batteries have language-specific norms. Some assessment tests, in particular, those for language development or rating scales may not be available as they have not been translated and validated. In that case, region and language-specific batteries and scales should be selected by an experienced (neuro)psychologist or developmental paediatrician.
Table 3. An extended or full clinical assessment battery for a comprehensive evaluation of school-age children (aged 5 to young adult) with CHD

Please note that the extended assessment battery is a current recommendation; examiners should carefully consider clinical, cultural, and ethical factors to adjust the battery as appropriate. The most recent test version and age-based norms are recommended. Some tests/rating scales are available in multiple languages; see details from the test publisher as this is continually updated based on revisions. Measures for special clinical considerations are included (e.g., TONI for a non-verbal child). Various options are represented within each domain, but clinicians should use their judgement to select the most appropriate option (e.g., typically only one measure of intelligence). Assessment of the child should also include the core assessment battery as shown in Table 2
Intellectual functioning
Intellectual functioning is influenced by an individual’s genes, environment, education, and experiences. An intelligence quotient (IQ) is obtained by using standardised tests of intellectual functioning, and often includes performance on multiple subtests related to verbal, visual, spatial, working memory, and processing speed abilities. Performance on standardised intellectual quotient tests is often considered to be an indicator of the child’s potential to learn in traditional educational environments. Children with CHD typically perform within the average range on measures of intellectual functioning, although children with the most complex forms of CHD score within the lower end of the average range. Reference Mahle, Clancy, Moss, Gerdes, Jobes and Wernovsky45,Reference Bellinger, Wypij and duPlessis46 Moreover, intellectual quotients related to verbal reasoning are often relatively stronger than those related to non-verbal tasks, including fluid reasoning and visual–spatial skills. Reference Karsdorp, Everaerd, Kindt and Mulder47 When significant intra-subtest variability occurs, indicating the presence of marked strengths and weaknesses, the index scores or overall Full-Scale Intellectual Quotient will not be informative. Additional assessment from other domains is necessary to identify patterns of strengths and weaknesses.
Language
Understanding and expressing language is fundamental to communication, learning, and social competency. Children with complex CHD can present with lower performance on measures of language and speech articulation. Reference Bellinger, Wypij and Kuban48,Reference Brosig, Mussatto and Hoffman49 Delays in language can hinder academic skill development, with a particular influence on learning and retention in the areas of reading, written expression, math reasoning, and auditory processing. Both receptive and expressive language requires an understanding and application of critical linguistic components including morphology, syntax, and semantics. Pragmatics is another necessary aspect of language, involving the non-verbal and verbal rules that are needed for social communication. Problems related to pragmatic language and social communication have more recently become evident in children with CHD. Reference Bellinger50,Reference Calderon, Bonnet, Courtin, Concordet, Plumet and Angeard51 Assessment in the area of language is essential to understand the child’s communication abilities and needs, especially in the younger child. A broad assessment typically includes evaluation in receptive, expressive, and pragmatic skills. If speech articulation is an area of concern, assessment of oromotor functioning, phonation (sound production), resonance, voice, and fluency may be necessary. Given the complexities of evaluating language, for those children with concerns, referral to a speech/language specialist may be needed to more fully assess needs and develop an intervention plan. This therapist may be part of the Cardiac Neurodevelopmental Follow-up Programme team or an outside referral may be needed.
Visual–spatial
Visual–spatial processing abilities are needed to make sense of and reason with information that is not easily put into words, such as symbols and visual patterns. From simple visual discrimination or matching to more complex pattern analysis and visuospatial constructional skills, the ability to process visual information permits access to real-world experiences and learning opportunities. In children with CHD, visual–spatial skills tend to be weaker than verbal abilities. Reference Karsdorp, Everaerd, Kindt and Mulder47,Reference Mills, McCusker, Tennyson and Hanna52 Children with visual–spatial weaknesses struggle with organising, remembering, recognising, and reproducing visual information. This may affect their performance on a variety of academic tasks, crossing multiple subject areas, including geometry, interpreting graphs and charts, copying notes off a board, using number lines, making and understanding maps, organising work on a page, and interpreting graphic organisers. Deficits in complex visual–spatial processing have been well documented amongst children and adolescents with critical CHD and have been linked to academic achievement difficulties, most notably in math and higher order reading comprehension. Reference Bean Jaworski, White, DeMaso, Newburger, Bellinger and Cassidy53,Reference Bellinger, Bernstein, Kirkwood, Rappaport and Newburger54 Children with relatively weaker visual–spatial skills may prefer to process content verbally, and may appear disorganised to their teachers. Assessment of visual–spatial skills will be an essential part of the evaluation and may reveal subtle to obvious impairments that indicate the need for accommodations in the classroom.
Memory
The ability to learn and remember information supports a foundation upon which more complex/abstract knowledge or experiences can be built intuitively. Memory is necessary for learning and later recalling the meaning of symbols (e.g., letters, numbers), vocabulary, math facts and procedures, historical events, and science facts, to name a few. Socially, memory abilities support the formation and maintenance of friendships, the ability to recall names and recognise familiar faces, and the ability to adhere to rules. Weaknesses in other domains can significantly impact memory as well, especially attention and executive function; thus, teasing apart the factors contributing to memory problems or “forgetfulness” is critical. For children with CHD specifically, available evidence seems to indicate memory vulnerability, although a consistent pattern of memory skills development has not been documented across studies. Reference Brosig, Mussatto and Hoffman49,Reference Mills, McCusker, Tennyson and Hanna52,Reference Pike, Woo and Poulsen55–Reference Wotherspoon, Eagleson and Gilmore57 A large study found that adolescents with critical biventricular CHD are indeed at risk for deficits in learning and memory, particularly visual–spatial memory. Reference Cassidy, Newburger and Bellinger58 The evaluation should therefore consider different types of learning and memory (e.g., rote versus contextual, verbal versus visual–spatial).
Attention/executive function
Attention is a multi-component domain that allows individuals to both focus on relevant stimuli and block out unnecessary distractions in the environment. Sustained attention, or the ability to concentrate and maintain attention over time, is particularly important for supporting on-task behaviour, and thus is crucial for effective performance in school, social, and recreational activities. Like attention, executive functioning is also a complex and multi-faceted domain that supports goal-directed behaviour. Inhibitory control, working memory, and cognitive flexibility (shifting) are generally recognised as fundamental executive functioning capacities, which in turn give rise to more complex and higher order executive functioning skills, such as planning and problem-solving. Reference Diamond59 Amongst the many areas of neurobehavioural vulnerability documented in studies of children and adolescents with CHD, attention and executive function deficits seem to be amongst the most prominent. Reference Cassidy, White, DeMaso, Newburger and Bellinger42,Reference Calderon, Bonnet, Courtin, Concordet, Plumet and Angeard51,Reference Sanz, Berl, Armour, Wang, Cheng and Donofrio60
Children with CHD have an increased incidence of attention-deficit/hyperactivity disorder Reference Holland, Cassidy and Stopp61,Reference DeMaso, Labella and Taylor62 including attention problems that can result in reduced engagement with instruction, and limited ability to complete assignments/homework. Children with hyperactivity/impulsivity are more likely than typical peers to miss classroom time due to behaviour problems and social relationships can be negatively impacted. They may struggle to demonstrate their learning effectively, since they are prone to inconsistent performance, careless errors, and impulsive responses, all of which can result in grades and test scores that underestimate a child’s ability. Students with weak executive functioning may struggle to plan their work and monitor their progress, which affects complex assignments and long-term projects. Poor organisation and flexibility can impact the older student’s ability to manage multiple classes and teachers, each with its own syllabus, routines, materials, and expectations. Executive problems may cause poor synthesis and integration of information, and reduce the ability to recognise underlying organisational structures. Reference Bean Jaworski, White, DeMaso, Newburger, Bellinger and Cassidy53 Instead, students may rely on concrete examples, and fail to perceive the overall gestalt of information, thus impairing multiple school activities, including recognising patterns and rules in math and science, identifying themes or main ideas in a text, focusing on a thesis or topic in writing, and drawing conclusions across texts and subjects. A comprehensive assessment of attention and executive functioning in the child with CHD should include multiple sources of data, including parent and teacher rating scales, behavioural observations, as well as objective assessment with standardised test measures.
Speed of processing
Processing speed refers to the efficiency with which an individual is able to take in information and generate an appropriate behavioural response. Reference Kail and Salthouse63 Throughout childhood and adolescence, developmental increases in white matter microstructure support greater speed of processing Reference Ferrer, Whitaker, Steele, Green, Wendelken and Bunge64 which in turn contributes to advances in fluid reasoning Reference Kail and Salthouse63,Reference Astrid65,Reference Kail66 and executive function skills. Reference Rose, Feldman and Jankowski67 Children and adolescents who process information more slowly than their peers are at risk for falling behind in the classroom, and may require extended time to effectively demonstrate their knowledge and skills. They may also become more easily distracted or off-task and have trouble taking notes. They are also at high risk for fatigue on account of having to exert considerably more effort than their peers to complete assignments and keep up with their classmates. The speed of processing may be undermined in the context of CHD. Reference Mills, McCusker, Tennyson and Hanna52 Amongst school-age children with critical CHD (d-transposition of the great arteries), processing speed was associated concurrently with executive function and reading abilities, and indirectly predicted later reading and math abilities. Reference Cassidy, White, DeMaso, Newburger and Bellinger41 Screening of processing speed is essential to the evaluation and can help facilitate accommodations for academic areas that are heavily reliant on the speed of performance (e.g., timed math fact testing, standardised testing).
Motor skills
Mastery of fine motor skills involves the ability to use the hands and fingers (in coordination with the eyes) to engage in activities such as picking up small objects, self-care, handwriting, and playing an instrument. Young children with CHD often struggle with tasks that require fine motor skills, such as feeding and turning book pages during infancy, and using scissors, tying shoelaces, and buttons/zippers during preschool. Reference Limperopoulos, Majnemer and Shevell68,Reference Limperopoulos, Majnemer and Shevell69 Weaknesses in fine motor skills have been reported in early elementary school years and can impact the development of letter and number formation skills in handwriting. Reference Majnemer, Limperopoulos, Shevell, Rosenblatt, Rohlicek and Tchervenkov70,Reference Holm, Fredriksen, Fosdahl, Olstad and Vollestad71 Fine motor impairments can also impact the accuracy and efficiency of keyboarding skills. If handwriting and/or keyboarding skills remain inefficient, it is challenging for the growing student to keep up with increasing academic demands. Evaluation of fine motor skills can be quick and easy, and can lead directly to academic recommendations (e.g., extended time for writing tasks). Technology tools may also be helpful and referral to an occupational therapist for an assistive technology evaluation may be needed.
Development of gross motor skills involves learning to coordinate the movements of the large muscles including legs, arms, and the body’s core. Given restrictions related to medical fragility and surgical interventions, it is not surprising that delays are often apparent within the first year of life in children with CHD. Although “catch-up” is often seen after about 18 months of life, delays may persist and manifest as appearing clumsy, having difficulty with balance, appearing awkward when running, jumping, climbing, or kicking a ball. Reference Holm, Fredriksen, Fosdahl, Olstad and Vollestad71 These limitations may have important impacts on social interactions in physical play or participation in team sports and may lead to teasing and bullying. Reference Liamlahi, von Rhein and Buhrer30 When concerns are presented or observed, referral to a physical therapist may be needed to assist with treatment options given that this area is not typically included in the neurodevelopmental evaluation. A physical therapist may be part of the Cardiac Neurodevelopmental Follow-up Programme team or an outside referral may be needed.
Academic
Historically, it has been found that approximately 1/3–1/2 of children with complex CHD receive special education services, while 7%–15% are placed in a separate classroom, and approximately 18% are retained a grade. Reference Bean Jaworski, White, DeMaso, Newburger, Bellinger and Cassidy53,Reference Bellinger, Wypij and Rivkin72,Reference Shillingford, Glanzman, Ittenbach, Clancy and Gaynor73 Children with more complex medical histories are at particularly high risk for learning challenges, including children with histories of cyanosis, single-ventricle physiology, seizure, stroke, multiple prolonged open-heart surgeries, and those who have underlying genetic conditions. Reference Bellinger, Rivkin and DeMaso74,Reference Wray and Sensky75 A population-based cohort study of third-grade educational records indicated that children with CHD were 1.24 times more likely to not meet academic standards in reading or math. Reference Oster, Watkins, Hill, Knight and Meyer76 Outcome studies indicate more specifically that math is especially vulnerable, Reference Cassidy, White, DeMaso, Newburger and Bellinger41,Reference Bellinger, Bernstein, Kirkwood, Rappaport and Newburger54,Reference Bellinger, Wypij and Rivkin72 although lower performance compared to the normative population has also been reported for reading and spelling. Reference Mahle, Clancy, Moss, Gerdes, Jobes and Wernovsky45,Reference Bellinger, Wypij and Rivkin72 Academic progress in reading and math requires integration of multiple cognitive skills that can be weak in children with CHD (e.g., visuospatial skills in math, attention, executive skills, and higher order language in reading comprehension). A written expression can also be challenging for children with CHD, partly due to fine motor weaknesses that impact handwriting, but also due to retrieval and executive functioning demands. If possible, the neurodevelopmental evaluation should include at least an academic screening, although some insurance companies will not cover academic testing. Coordination with the schools may be needed for more extensive testing of academic areas that are a concern. Recently, some Cardiac Neurodevelopmental Follow-up Programmes have added school intervention specialists to act as liaisons between the family, the school, and the medical team.
Emotional and behavioural
Evaluation of emotional and behavioural functioning typically involves rating scales from parents, teachers, and the child/adolescent, but should also include observations of the child during testing and with family members. When needed, a clinical interview with the child could also be completed. Comparisons across raters can highlight pervasive problems or variability across settings, as well as the child’s self-awareness. A confluence of factors places children with CHD at increased risk for emotional and behavioural challenges, Reference DeMaso, Calderon and Taylor77 including disease/medical factors, Reference Holland, Cassidy and Stopp61,Reference Freitas, Castro and Sarmento78 parenting style, Reference Brosig, Mussatto, Kuhn and Tweddell79 and family stress. Reference Visconti, Saudino, Rappaport, Newburger and Bellinger80–Reference Ravindran and Rempel82 The type of informant and setting can be associated with different perceptions of the child’s psychosocial adjustment, and/or the child may behave differently across settings based on the level of structure or overwhelm; the differences between informants should be interpreted carefully for each child. Reference McCusker, Armstrong, Mullen, Doherty and Casey83,Reference Bellinger, Newburger, Wypij, Kuban, duPlesssis and Rappaport84 Self-report measures completed by the school-age child may show fewer symptoms than other informants, Reference DeMaso, Labella and Taylor62 but an increase in psychosocial problems has also be reported by older children, Reference Freitas, Castro and Sarmento78 which may relate to greater self-awareness of limitations, feeling different than peers, learning challenges, and worry about the future. Both internalising and externalising symptoms become more apparent across raters in older children, Reference Karsdorp, Everaerd, Kindt and Mulder47 and adolescent females (compared to males) are at higher risk of problems with psychosocial adjustment. Reference Freitas, Castro and Sarmento78 Less adaptive coping strategies Reference Jackson, Gerardo, Monti, Schofield and Vannatta85 and externalising problems in children and adolescents have been associated with weaker executive functioning. Reference Cassidy86 Positive appraisals related to living with CHD have also been reported by patients on the quality of life measures, Reference Schaefer, von Rhein and Knirsch87 thus highlighting their psychosocial resiliency, but a higher quality of life is also associated with lower disease severity. Reference Latal, Helfricht, Fischer, Bauersfeld and Landolt88,Reference Marino, Tomlinson and Wernovsky89
Adaptive
Adaptive skills include “the practical, everyday skills required to function and meet environmental demands, including effectively and independently taking care of oneself and interacting with people”, or “how well a person meets community standards of personal independence and social responsibility in comparison to others of similar age and socio-cultural background”. Reference Association90,Reference Harrison and Oakland91 Studies of children with CHD suggest that adaptive delays can be seen as early as 18–24 months of age, and can persist into early school-age years across multiple domains, especially conceptual and social skills. Reference Alton, Rempel, Robertson, Newburn-Cook and Norris92,Reference Alton, Taghados, Joffe, Robertson and Dinu93 Achieving success in adaptive functioning is certainly related to other developmental skills, such as fine-motor skills for self-care, language for communication, emotional/behavioural adjustment for social/leisure skills, and executive functioning for self-direction. Opportunities to interact with the environment also are crucial to the development of adaptive skills. In children with CHD, these opportunities may be restricted due to illness Reference Uzark, Zak and Shrader94 or parental overprotectiveness Reference DeMaso, Campis, Wypij, Bertram, Lipshitz and Freed95 both of which may contribute to increased dependence and poor adaptive skills. Indeed, healthy siblings/cousins of children with CHD tend to have stronger adaptive skills. Reference Kern, Hinton, Nereo, Hayes and Gersony96 A comprehensive measure of adaptive functioning completed by a primary caregiver should be part of the neurodevelopmental evaluation.
Social
Challenges in social functioning have been identified in a number of studies on children with CHD, Reference Bellinger50,Reference Williams, McCrindle, Ashburn, Jonas, Mavroudis and Blackstone97 including the ability to appreciate subtle social rules and pragmatic nuances of language, the ability to engage appropriately in reciprocal social interactions, and the ability to self-monitor and regulate behaviour/impulses in ways that support typical peer relationships. Social difficulties may present as awkwardness, immaturity, or annoying behaviours around children/adults, social withdrawal or a preference to play alone, problems initiating or maintaining age-typical relationships, increased teasing/bullying (as well as poor ability to recognise these), and difficulty advocating for oneself and resisting peer pressure. A deficit in theory of mind, or the ability to understand and appreciate another person’s perspectives, has specifically been identified as an important contributor to the social challenges of children with CHD, Reference Bellinger50,Reference Calderon and Bellinger98 and may be associated with an increased risk of autism spectrum disorder in children with CHD. Reference Tsao, Lee and Jeng99 Along with behavioural observations and parent report, behaviour rating scales from various observers will be important for assessing social functioning. When concerns are raised about possible autism spectrum disorder, it may be necessary to refer to a trained specialist.
Assessment recommendations
As described above, the American Heart Association and the American Academy of Paediatrics scientific statement Reference Marino, Lipkin and Newburger1 for the management of developmental concerns in CHD made general recommendations for test measures to be included in the neurodevelopmental evaluation. Since the publication of this statement in 2012, working group and steering committee members of the Cardiac Neurodevelopmental Outcome Collaborative have created assessment battery recommendations to fully address both clinical needs and challenges, as well as research. The first assessment battery is considered the core test battery, or a bare minimum set of measures that are highly recommended. This includes measures selected because they are clinically sensitive, psychometrically strong and well-normed, widely available, allow for continuity/comparison across most of the paediatric years, allow for (brief) assessment across domains, and include both objective and subjective measures. This core test battery is brief, and thus will help guide evaluation priorities at sites or for clinical situations that are impacted by limited funding/insurance issues and/or limited testing/provider resources. In some cases, there are test choices within a domain to allow sites with only limited instruments to use readily available tests and thus reduce costs and training. See Table 2 for the core assessment battery.
A second extended assessment battery was also developed to provide recommendations for a more comprehensive neurodevelopmental evaluation. This is meant as an extension of the core battery. The longer protocol includes test choices within domains that can be used based on the reason for referral, presenting concerns, differential diagnosis, global delays, sensory/motor impairments, or reduced site/provider resources. The extended assessment battery can be used to evaluate domains more extensively at key developmental transition points, and when ongoing concerns are present and interventions need to be updated. Some measures can be used to obtain an age equivalency for skill areas in children who are unable to complete a measure typical for chronological age. Parent rating scales on the extended assessment battery include areas that may contribute to developmental concerns in the child (e.g., parent stress, family environment). Some measures below are determined to be amongst the best tools available, but may have normative or psychometric limitations (e.g., Lafayette Grooved Pegboard). Finally, a gold standard measure for evaluating behaviours related to possible autism spectrum disorder requires extensive and specialised training; this expertise may not be available at all sites and an outside referral may be needed. See Table 3 for the extended assessment battery.
It is important to note that the assessment batteries published in this paper are meant to be current recommendations. All trained examiners realise that standardised test instruments change across time for many reasons, including updated normative data and attempts to reduce cultural bias. Some tests are discontinued over time. More recently, commonly used tests are being transitioned to digital assessment tools (e.g., Q Interactive, Q Global), and in the near future, the original test kits will no longer be available. This is igniting a paradigm shift in how we administer test measures and digitally store information about a child’s abilities. Despite this, measures in the core battery are expected to continue to exist in some form over time. It is essential that trained professionals continually update their knowledge about current measures so that the most appropriate clinical and ethical considerations can be applied in measuring a child’s abilities.
Summary
The number of children and adults with CHD is growing faster than the systems that support them. The school-age years are a critical time for identifying and monitoring developmental needs to help children and families gain access to resources. When referrals are part of routine care in children with CHD and within a Cardiac Neurodevelopmental Follow-up Programme, associated anxiety may be lessened in families, developmental concerns can be identified before serious problems arise, and school/family may be more likely to adhere to recommendations. Consistent use of recommended assessment batteries will also increase opportunities for research collaborations across sites Reference Wernovsky100 . With larger research samples and standardised assessment batteries, outcome data will be more likely to improve the quality of care, thereby also increasing the quality of life in children and families of children with CHD.
Acknowledgements
This work represents the efforts of the working groups within the Cardiac Neurodevelopmental Symposium, and more recently, the Cardiac Neurodevelopmental Outcome Collaborative, which is supported by its institutional members. For an updated list of current Cardiac Neurodevelopmental Outcome Collaborative members, visit the following link: https://www.cardiacneuro.org/institutions/.
Financial support
This research received no specific grant from any funding agency, commercial, or not-for-profit sectors.
Conflicts of interest
None.