The assessment of the haemodynamic status of neonates during the transitional period has gained considerable interest over the last decade. Several modalities are now being implemented to measure myocardial function, cardiac output, and end organ perfusion to form a more comprehensive appraisal of the cardiovascular system.Reference Groves, Singh and Dempsey1 In particular, the use of echocardiography, non-invasive cardiac output monitoring, and near-infrared spectroscopy can facilitate a more targeted approach to the management of cardiovascular compromise, aid in monitoring the response to treatment and provide important prognostic information.Reference Dempsey and El-Khuffash2
More advanced echocardiography techniques, including deformation analysis and measurement of rotational mechanics, may prove superior to more conventional measurements of myocardial function (such as shortening fraction) in identifying dysfunction, characterising disease-specific myocardial phenotype, and guiding therapeutic intervention.Reference Breatnach, Levy, James, Franklin and El-Khuffash3 Furthermore, the use of bioreactance technology for the continuous and non-invasive assessment of cardiac output, stroke volume, and systemic vascular resistance can improve how we monitor the cardiovascular health beyond the simplistic use of blood pressure, which can often be misleading.Reference Weisz, Jain, Ting, McNamara and El-Khuffash4, Reference Forman, Breatnach and Ryan5
Reference ranges for myocardial deformation and rotational mechanics in addition to cardiac output measured non-invasively are emerging for term infants greater than 37 weeks gestation, and extremely premature infants less than 29 weeks gestation.Reference El-Khuffash, Schubert, Levy, Nestaas and de Boode6, Reference James, Corcoran, Mertens, Franklin and El-Khuffash7 However, there is a paucity of data on mid-to-late preterm infants between 30+0 and 34+6 weeks gestation. In the clinical setting, this cohort of infants is vulnerable to respiratory morbidity and is at risk of pulmonary hypertension; they are usually managed with data extrapolated from term infants. There is a need to describe patterns of various myocardial and haemodynamic parameters for this cohort. In this study, we aimed to describe left and right ventricular functional measurements, including longitudinal strain and systolic strain rate in addition to left ventricular rotational mechanics in this population over the first 48 hours of age. We also aimed to describe the non-invasive assessment of left ventricular output, stroke volume, and total peripheral resistance in stable preterm infants between 30 and 34 weeks gestation over the first 48 hours of age.
Methods
This was a prospective observational study carried out at the Rotunda Hospital, Dublin, Ireland over an 8-month period between April and November, 2018. The Rotunda Hospital is a stand-alone tertiary maternity hospital with 9000 deliveries per annum. Preterm infants between 30+0 and 34+6 weeks gestation admitted to the neonatal ICU were considered for inclusion. Infants with CHD, chromosomal abnormalities, life-limiting conditions, and those who developed culture-proven sepsis, needed inotropes and/or inhaled nitric oxide over the first week of age, and those that died before hospital discharge were excluded from the study. In addition, we excluded multiple pregnancies with monochorionic-diamniotic twins with evidence of twin-to-twin transfusion syndrome due to the documented myocardial dysfunction occurring in this group of infants.Reference Breatnach, Bussmann and Levy8 Parents of eligible infants were approached shortly after neonatal ICU admission and informed written consent was obtained before enrolment. The ethical committee on human research at The Rotunda Hospital approved the protocol.
Following recruitment, important antenatal, birth, and neonatal characteristics were collected. This included mode of delivery, gender, gestation, birthweight, important antenatal events, Apgar score and cord pH, need for resuscitation, respiratory status, need for/and type of ventilation support, and important outcomes including the need for surfactant replacement therapy, duration of ventilation, and length of hospital stay.
Echocardiography assessment
Echocardiography was carried out on Day 1 within the first 10 hours following birth and at the end of Day 2 of age using a Vivid S6 ultrasound system (General Electric Medical, Milwaukee, United States of America) with either a 7–12 MHz multi-frequency probe. Scans were performed without sedation when the infants were in a quiet steady state in a supine position. Image acquisition was performed in accordance with recently published guidelines using standard neonatal windows.Reference de Boode, Singh and Gupta9 All images were transferred to an archiving system in raw Digital Imaging and Communication in Medicine format for offline analysis by a single investigator. A detailed description of the methodology used to obtain the images and perform offline analysis, in addition to feasibility and reproducibility data of all the functional measurements are described in detail elsewhere.Reference Groves, Singh and Dempsey1, Reference El-Khuffash, Schubert, Levy, Nestaas and de Boode6, Reference Nestaas, Schubert, de Boode and El-Khuffash10
We obtained conventional functional measurements including ejection fraction, mitral and tricuspid valve early and late diastolic velocities. Patent ductus arteriosus characteristics including diameter, systolic and diastolic flow velocities and flow pattern were collected. Left and right ventricular dimensions were obtained including left ventricular end-diastolic diameter, left ventricular length, mitral value annulus diameter, aortic valve diameter, right ventricular length and mid-cavity diameters, tricuspid valve annulus and pulmonary artery diameters.Reference James, Corcoran and Jain11 Pulmonary artery acceleration time and right ventricular ejection time were obtained from the pulmonary artery pulsed wave Doppler.Reference Jain, Mohamed and El-Khuffash12 In addition, right ventricle-specific functional parameters including tricuspid annular plane systolic excursion and fractional area change were measured using a right ventricle-focused four-chamber view.Reference James, Corcoran and Jain11, Reference Levy, Dioneda and Holland13
Tissue Doppler imaging was used to obtain systolic, early diastolic, and late diastolic velocities from the bases of the left ventricular lateral wall, the septum, and the right ventricular free wall using methodology published elsewhere.Reference Nestaas, Schubert, de Boode and El-Khuffash10 Left ventricular event timings including systolic and diastolic times, isovolumic relaxation, and isovolumic contraction were measured using the tissue Doppler wave obtained from the septum. We narrowed the sector width to achieve a frame rate of greater than 240 frames per second for image acquisition.Reference de Boode, Singh and Gupta9
Speckle tracking echocardiography was used to derive left ventricular global longitudinal strain and longitudinal systolic strain rate using the apical four-, two-, and three-chamber views. In addition, right ventricular free wall longitudinal strain and longitudinal systolic strain rate were derived from a right ventricle-focused apical view using a published protocol.Reference El-Khuffash, Schubert, Levy, Nestaas and de Boode6 Left ventricular rotational mechanics including apical and basal rotation, twist, torsion (twist indexed to length), twist and untwist rates were also derived using speckle tracking echocardiography from the parasternal short-axis view at the levels of the mitral valve and the apex.Reference James, Corcoran, Mertens, Franklin and El-Khuffash7 We used a frame rate between 120 and 130 frames per second for image acquisition to achieve frame rate to heart rate ratio of 0.7–0.9 for optimal tracking.Reference El-Khuffash, Schubert, Levy, Nestaas and de Boode6 We presented absolute deformation values (without the negative sign where appropriate), and therefore, higher values indicate higher function.
Continuous haemodynamic monitoring
We used the NICOM™ system (Cheetah Medical Inc., Massachusetts, United States of America) that employs transthoracic bioreactance to obtain continuous haemodynamic readings during the study period. Bioreactance is a technique which involves the analysis of the frequency spectra variation resulting from a delivered oscillating current when it traverses the thoracic cavity.Reference Squara, Denjean, Estagnasie, Brusset, Dib and Dubois14 Four emitting and receiving electrodes are placed on the anterior thorax in a manner that “boxes” the heart. The sensor strips consist of two contact points. Upper thoracic electrode strips were placed over the mid-clavicles and upper back bilaterally. The lower electrode sensors are placed between the sixth and seventh intercostal spaces at the mid-axillary line. NICOM measurement of stroke volume and left ventricular output are obtained every minute. Systemic vascular resistance is calculated by the NICOM system on an hourly basis as the mean blood pressure is manually entered using the following formula: systemic vascular resistance = (mean blood pressure × 80)/left ventricular output as per the entered algorithm. Blood pressure was measured non-invasively on an hourly basis by the nursing staff using an appropriately sized cuff. Our group has previously demonstrated the reliability of NICOM in trending changes in left ventricular output, stroke volume, and systemic vascular resistance over time in various neonatal populations.Reference Weisz, Jain, Ting, McNamara and El-Khuffash4, Reference Forman, Breatnach and Ryan5, Reference Weisz, Jain, McNamara and El-Khuffash15
Statistical analysis
Continuous data were tested for normality using the Shapiro–Wilk test and a histogram representation of data and summarised as means (standard deviation) or medians [interquartile range] as appropriate. Categorical data were summarised as counts (%). Two group analyses were conducted using the Student’s t-test, the Mann–Whitney U-test, or Chi-square test as appropriate. Linear regression was used to assess independent association between important predictor variables and speckle tracking echocardiography-derived functional measurements. Serial data were compared using one-way analysis of variance with repeated measures. Change in the continuous haemodynamic data from baseline was compared between infants with and without surfactant administration using a graphical representation and change from baseline using mean change and 95% confidence intervals. We used SPSS version 25 to conduct the analyses. Statistical significance is achieved with a p-value < 0.05.
Results
During the study period, 116 infants between 30+0 and 34+6 were admitted to the neonatal ICU: 15 refused consent, 37 were not approached due to investigator/equipment unavailability, 7 had chromosomal anomalies, 5 had life-limiting conditions, 4 were monochorionic-diamniotic twins, and 3 received inotropes. Forty-five infants with a mean (± standard deviation) gestation and birthweight of 32.7 ± 1.2 weeks and 1894 ± 345 g were included in this study. Twenty-one (47%) were male, 42 (93%) were delivered via caesarean section, 32 (71%) received a complete course of antenatal steroids, and 15 (33%) received magnesium sulphate. Seven mothers (16%) developed pre-eclampsia prior to delivery with two (4%) exhibiting absent umbilical artery end-diastolic flow. Nine mothers (20%) had prolonged rupture of membranes. Twenty-one infants (47%) were from a dichorionic-diamniotic twin pregnancy. The median [interquartile range] cord pH and 5-minute Apgar score were 7.31 [7.28–7.35] and 9 [9–10], respectively. Ten infants (22%) required invasive mechanical ventilation for 1 day (in addition to surfactant administration) and 34 infants required continuous positive airway pressure for a median of 2 [1–5] days. The infants’ median hospital stay was 17 [12–23] days. All infants survived to hospital discharge without significant morbidity and were free of oxygen.
Table 1 illustrates the conventional echocardiography markers. There was no change in ejection fraction or mitral valve inflow velocities over the two time points. There was an increase in tricuspid valve atrial contraction wave and velocity time index. All infants had a patent ductus arteriosus on Day 1 and this decreased to 36% by Day 2. There was an increase in systolic and diastolic velocities across the ductus over the two time points. The proportion of infants (out of those with an open ductus) with a bidirectional shunt remained constant over the two time points (Table 1).
Table 1. Conventional measurements
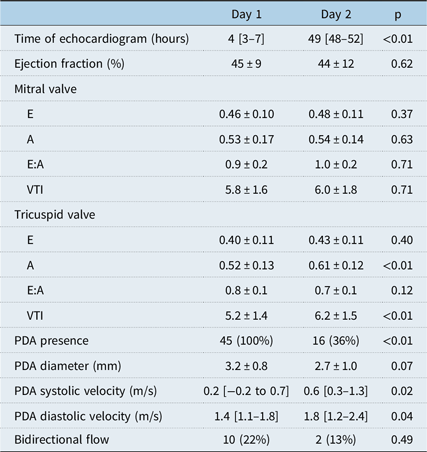
VTI = Velocity time index; PDA = Patent Ductus Arteriosus.
Values presented as means ± SD, median [interquartile range], or count (%).
There was no change in left ventricular dimensions or event timings over the two time points (Table 2). Septal wall tissue Doppler diastolic function measurements increased over the study period. Speckle tracking echocardiography-derived left ventricular global longitudinal strain (but not systolic strain rate) also increased in addition to untwist rate (Table 2). There was an increase in right ventricular pulmonary artery acceleration time, right ventricular ejection time, and pulmonary artery acceleration time to right ventricular ejection time ratio. This was accompanied by an increase in right ventricular free wall early diastolic tissue Doppler velocity wave, in addition to tricuspid annular plane systolic excursion and fractional area change (Table 3).
Table 2. Left ventricle function measurements

SR = Strain Rate.
Values presented as means ± SD, median [interquartile range], or count (%).
Table 3. Right ventricle function measurements
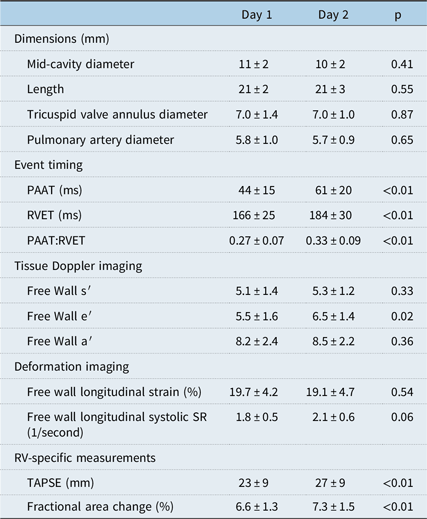
PAAT = Pulmonary Artery Acceleration Time; RVET = Right Ventricular Ejection Time; TAPSE = Tricuspid Annual Plane Systolic Excursion; SR = Strain Rate.
Values presented as means ± SD, median [interquartile range], or count (%).
Using univariate analysis, we examined the association between potential important perinatal characteristics (multiple pregnancies, pre-eclampsia, antenatal steroids) and speckle tracking echocardiography-derived functional measurements. Infants in receipt of a complete course of antenatal steroids demonstrated lower Day 1 left ventricular global longitudinal systolic strain rate (1.6 ± 0.2 versus 1.9 ± 0.3 1/second, p < 0.01) and lower Day 2 right ventricular free wall longitudinal strain (17.0 ± 3.6 versus 23.9 ± 4.2%, p < 0.01). This relationship remained significant for both measurements on linear regression when adjusting for gestational age (left ventricular global longitudinal systolic strain rate: standardised β −0.48, p < 0.01; right ventricular free wall longitudinal strain: standardised β −0.64, p < 0.01). There were no associations between ventilation status, patent ductus arteriosus presence, flow pattern, and any of the speckle tracking echocardiography-derived functional measurements on either day (data not shown). In addition, dichorionic-diamniotic twin pregnancy did not have an influence on any of the measured functional parameters (data not shown).
NICOM data were available on 29 infants and were commenced at a median of 4 [3–6] hours. Those infants had a similar gestation (32.6 ± 1.2 weeks) and birthweight (1900 ± 393 g) to the entire cohort. In addition, they had a similar rate of male gender (43%), twin deliveries (32%), caesarean section (93%), pre-eclampsia (21%), prolonged rupture of membranes (25%), magnesium sulphate (39%), and a complete course of antenatal steroid administration (71%). There was an increase in NICOM-derived left ventricular output over the study period [mean 34%, 95% confidence interval 21–47%]. This was driven by a predominant increase in NICOM-derived stroke volume [29%, 16–42%] rather than heart rate [5%, −2 to 12%]. There was an increase in mean blood pressure [11%, 1–21%] but a fall in systemic vascular resistance [−14%, −25 to −3%] (Fig 1). Six infants received surfactant replacement therapy and had a higher increase in left ventricular output (61 versus 27%, p = 0.02) and stroke volume (57 versus 22%, p = 0.02) over the study period. There was no difference in the change of heart rate, systemic vascular resistance, or mean blood pressure between infants with and without surfactant administration. In addition, there was no difference in echocardiography-derived pulmonary artery acceleration time or right ventricular ejection time between infants with or without surfactant administration.

Figure 1. Non-invasive cardiac output monitoring measurements. Whiskers represent one standard error. BP = blood pressure. X-axis denotes time from birth in hours.
Discussion
In this prospective observational cohort study, we determined patterns for left and right ventricular functional measurements derived using conventional and advanced echocardiography techniques in mid-to-late preterm infants born between 30+0 and 34+6 weeks gestation during the immediate transitional period. We also presented continuous non-invasively-derived haemodynamic data including left ventricular output, stroke volume, and systemic vascular resistance over a 48-hour period soon after birth. We demonstrated increases in functional parameters predominantly in the right ventricle. Those changes coincided with an increase in left ventricular output and stroke volume identified using NICOM. The administration of antenatal steroids was associated with lower Day 1 left ventricular global longitudinal strain rate and lower Day 2 right ventricular free wall longitudinal strain. Surfactant administration resulted in a larger increase in stroke volume and left ventricular output over the study period. A large proportion of infants in our cohort were from a dichorionic-diamniotic twin pregnancy. This did not appear to influence any of the functional measurements on univariate analysis. We previously reported that monochorionic-diamniotic twin pregnancies (which we excluded from this study) demonstrated important functional patterns especially in those with evidence of twin-to-twin transfusion syndrome.Reference Breatnach, Bussmann and Levy8
The assessment of myocardial performance during the transitional period in the neonatal population using newer echocardiography techniques is gaining considerable interest.Reference Breatnach, Levy, James, Franklin and El-Khuffash3 Reference values in addition to changes to those functional measurements secondary to certain disease states in extremely preterm infants (<29 weeks gestation) and in term infants (>37 weeks gestation) are emerging in the literature.Reference de Boode, Roehr and El-Khuffash16 However, there is a paucity of data on infants in the later preterm phase, particularly between 30 and 34 weeks gestation. In clinical practise, the haemodynamic management of those infants using echocardiography currently relies on data extrapolated from term infants. This approach is inappropriate as this cohort of infants is likely to still experience functional and structural immaturity more closely related to their more premature counterparts. The myocardium of those infants is also likely to be “characterised by systolic dysfunction due to an immature and inefficient contractile apparatus and diastolic dysfunction due to the lack of elastic compliant tissue and a preponderance of stiff fibres.”Reference Bussmann and El-Khuffash17 The functional reserve in this group is also likely to be compromised and therefore ill equipped to face early postnatal stresses. In addition, later preterm infants are at a higher risk of experiencing respiratory morbidity including respiratory distress syndrome and pulmonary hypertension; they are also likely to receive interventions such as surfactant replacement therapy.Reference Huff, Rose and Engle18 All of these conditions can influence myocardial performance during the early neonatal period.
The functional echocardiography data obtained from our study population resemble the trends obtained from more extremely premature infants (<29 weeks gestation), rather than term infants.Reference James, Corcoran and Jain11 A patent ductus is present in all infants at Day 1, with over a third (36%) remaining open by 48 hours of age. This contrasts with term infants where the majority (64%) exhibit ductal closure by Day 1 with only 4% remaining patent by Day 2. In addition, none of the healthy term population exhibit bidirectional shunting across the ductus by 24 hours of age.Reference Jain, Mohamed and Kavanagh19 We compared left and right ventricle longitudinal strain measurements derived from this cohort with published data (by our group) from extremely preterm infants <29 weeks gestation and healthy term infants between 37 and 42 weeks gestation.Reference Levy, El-Khuffash and Patel20, Reference Breatnach, Forman and Foran21 Day 1 left and right ventricular longitudinal strain obtained from this cohort more closely resemble data from extremely preterm infants (Fig 2). Furthermore, Day 1 left ventricle rotational mechanics obtained from this cohort resemble those obtained from the more extremely premature population which are characterised by lower apical rotation and a blunted counter-movement of the base resulting in lower twist and torsion when compared to controls (Table 4).Reference James, Corcoran, Mertens, Franklin and El-Khuffash7, Reference Breatnach, Forman and Foran21In term infants and older children, physiologically, torsional mechanisms are greatest towards the apex because (1) the right-handed helix in the subendocardium and the left-handed helix in the subepicardium converge towards the apex to form the “vortex of the double helical loop”; and (2) the electric excitation of cardiac motion begins in the apex and travels to the base.Reference Levy, El-Khuffash and Patel20 Prematurity may alter these mechanisms and the observed functional differences in this study further emphasise the potential vulnerability of this cohort and the limited myocardial reserve present in mid-to-late preterm infants. The apparent negative effect of antenatal steroid administration on left ventricular global longitudinal systolic strain rate on Day 1 and right ventricular longitudinal strain on Day 2 is interesting. Animal studies demonstrate varying effects of antenatal steroid administration on the cardiomyocyte ranging from acceleration of structural maturity and proliferation (promoting improved function) to alterations to β-adrenoceptor responsiveness “which may render the offspring vulnerable to subsequent cardiac dysfunction.”Reference Tare, Miller and Wallace22, Reference Sakurai, Osada and Takeba23 Further clinical studies are needed to assess the morphological and functional effect of antenatal steroid administration in the neonatal population.
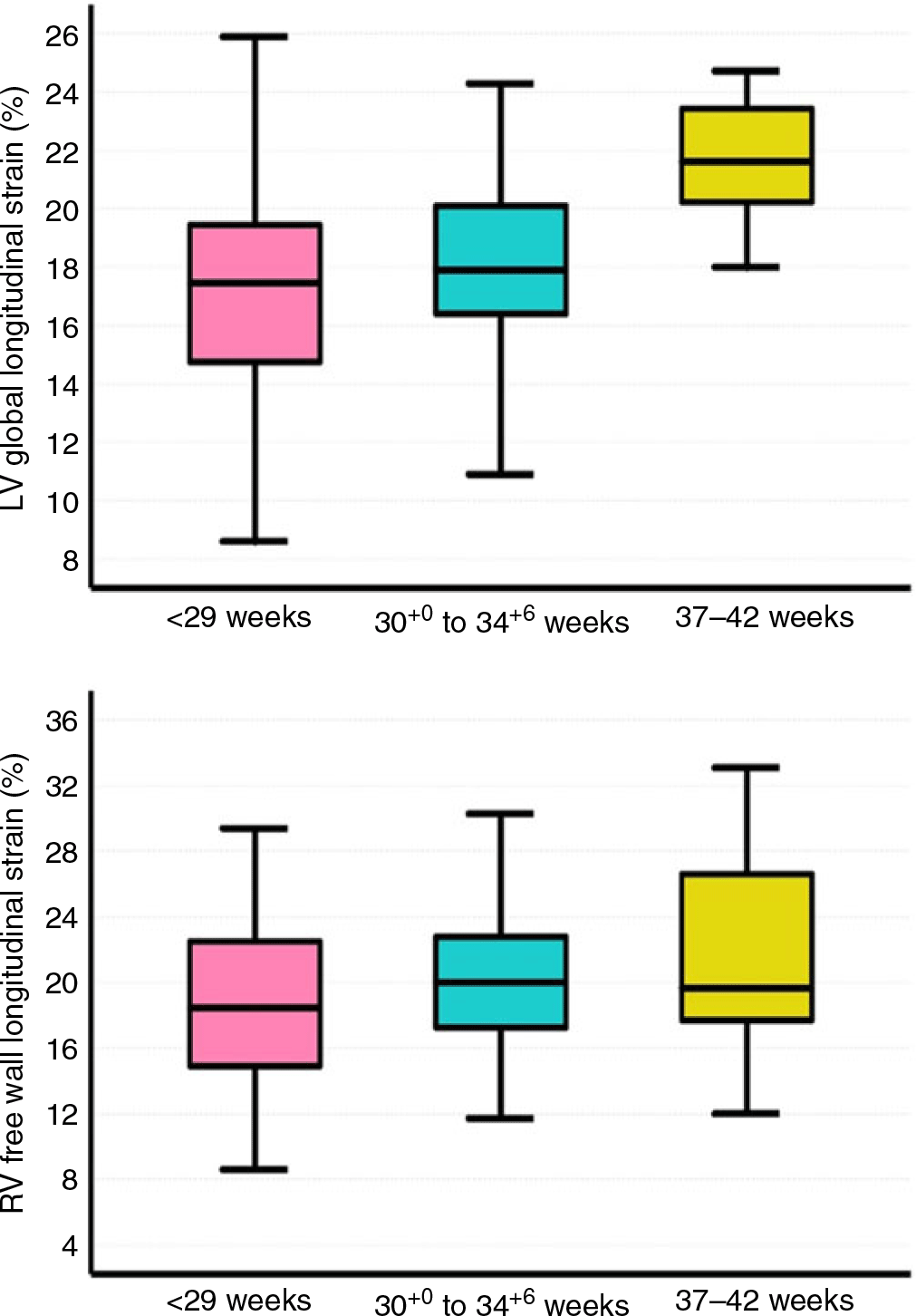
Figure 2. Deformation measurement comparisons on Day 1 of age. LV = left ventricle; RV = right ventricle. Preterm infant data obtained from ref. (Reference Levy, El-Khuffash and Patel20). Term infant data obtained from ref. (Reference Breatnach, Forman and Foran21).
Table 4. Left ventricle rotational mechanics comparisons

LV = Left ventricle.
Values presented as median [interquartile range]
In this cohort, the most important change occurring during the transitional period appears to be the fall in pulmonary vascular resistance identified using pulmonary artery acceleration time and right ventricular ejection time. Those measurements have previously been shown to closely correlate with right heart catheterisation measurements of pulmonary vascular resistance in children.Reference Levy, Patel and Groh24 A rising pulmonary artery acceleration time (in addition to the indexed measure, pulmonary artery acceleration time to right ventricular ejection time ratio) indicates a fall in pulmonary vascular resistance. In our population, there was a significant rise in pulmonary artery acceleration time and pulmonary artery acceleration time to right ventricular ejection time ratio indicating a fall in pulmonary vascular resistance. This was accompanied by an increase in left ventricular output driven mainly by an increase in stroke volume rather than heart rate suggesting an improvement in pulmonary blood flow and left ventricular preload. Surfactant administration to this patient cohort appears to augment this rise in left ventricular output secondary to stroke volume improvement. The underlying mechanism of this surfactant-associated increase is unclear as we were unable to demonstrate differences in pulmonary artery acceleration time between infants with and without surfactant administration. This may be secondary to the relatively small sample size of our cohort. However, the mechanism is likely to be increased pulmonary blood flow. There was an increase in some right ventricular systolic measures of function, tricuspid annular plane systolic excursion, and fractional area change, highlighting improved right ventricular performance secondary to a fall in right ventricular afterload. The lack of demonstrable improvement in right ventricular deformation measurement is likely to reflect the relative lack of influence of loading conditions on those parameters.
Assessing function in a relatively stable cohort of infants in this gestational range will assist the clinician in managing dysfunction occurring in various disease states and grading disease severity. In addition, those values can aid the clinician in monitoring response to treatment. There is an increasing realisation that premature birth is associated with a higher risk of cardiovascular events later in life, including heart failure, a reduction in myocardial functional reserve, and an impaired response to physiological stress.Reference Burchert and Lewandowski25 Measuring left and right ventricular performance using deformation has the advantage of characterising function regionally and globally. Deformation analysis can also be used to reveal the underlying pathophysiological aetiology for dysfunction, and aid in risk stratification and prognostication of infants at greatest risk of adverse long-term cardiovascular outcome. Strain is influenced by loading conditions and intrinsic contractility and therefore, a fall in strain can be a result of either adverse loading conditions or a compromise in intrinsic contractility. On the other hand, systolic strain rate appears to be uninfluenced by loading conditions and any changes in its value are likely to reflect intrinsic contractility. “Characterization of adverse loading conditions and impaired contractility with advanced strain and strain rate measures provide a deeper understanding of myocardial performance phenotyping in preterm infants.”Reference Bussmann and El-Khuffash17 Speckle tracking echocardiography has the advantage of being angle-independent. However, tracking can be compromised in when the heart rate is very fast due to frame rate limitations, and therefore assessment of diastolic function in premature infants using this modality required further research and validation.Reference El-Khuffash, Schubert, Levy, Nestaas and de Boode6
Tissue Doppler imaging has the advantage through the high-temporal resolution of accurately determining event timings throughout the cardiac cycle. This can provide further physiological insights into functional phenotype exhibited by infants between 30 and 34 weeks gestation. For example, is it evident from this data set that this cohort spends a longer time in systole rather than diastole providing further evidence that their myocardial function is closer to the more immature counterparts (less than 29 weeks gestation) rather than term infants. Tissue Doppler imaging is very angle-dependent, however, which can make accurate assessment of velocities difficult is the alignment of the ventricular walls in relation to the interrogation line is suboptimal. In addition, non-functioning regions on the myocardial walls through tethering to functional regions within the myocardium may appear to have normal velocities.Reference Nestaas, Schubert, de Boode and El-Khuffash10, Reference Breatnach, Franklin, James, McCallion and El-Khuffash26
The importance of these results should be interpreted within the framework of the inherent limitations in this study. The relatively small sample size limited our ability to assess the impact of all important antenatal and perinatal factors on myocardial performance during the transitional period. However, this study serves as a stepping stone for further research on myocardial function and adaptation under normal physiological circumstances in addition to pathological conditions in infants in this gestational age bracket. Research questions must now focus on further delineating changes during the transitional period, the impact of important disease state including pulmonary hypertension and growth restriction.
In conclusion, this study illustrates values of left and right ventricle functional parameters in uncomplicated mid-to-late premature infants born between 30 and 34 weeks gestation during the early transitional period. Left ventricular function remains relatively preserved over the first 48 hours in this population. Right ventricular function measurements (tricuspid annular plane systolic excursion and fractional area change) increase in magnitude, likely reflecting the physiological decline in pulmonary vascular resistance with an observed increase in pulmonary artery acceleration time measures. Non-invasive cardiac output monitoring is feasible in mid-to-late preterm infants and highlights important changes over the transitional period. There is an increase in left ventricular output which is driven by an improvement in stroke volume. This is likely to represent improved loading conditions secondary with enhanced pulmonary blood flow due to declining pulmonary and systemic vascular resistance. Surfactant administration may further augment left ventricular preload in this population.
Acknowledgements
None.
Financial Support
This study was funded by multiple sources: EU FP7/2007-2013 grant (agreement no. 260777, The HIP Trial); the Friends of the Rotunda Research Grant (Reference: FoR/EQUIPMENT/101572); Health Research Board Mother and Baby Clinical Trials Network Ireland (CTN-2014-10); Medical Research Charities Group/Health Research Board/Friends of the Rotunda Research Grant (HANDLE Study, MRCG-2013-9).
Conflict of Interest
None.
Ethical Standards
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national guidelines on human experimentation (Irish Council of Bioethics) and with the Helsinki Declaration of 1975, as revised in 2008, and have been approved by the institutional committees (Rotunda Hospital Ethics Board).








