Infants with congenitally malformed hearts have a high incidence of being born with low weight, that is of less than or equal to 2500 grams at birth.Reference Rosenthal, Wilson, Pemutt, Boughman and Ferencz1–Reference Kramer, Trampisch, Rammos and Giese3 Such low weight has been found to be a risk factor for increased mortality for infants undergoing surgical correction of congenital cardiac disease.Reference Pawade, Waterson, Laussen, Karl and Mee4 This increased risk is probably multifactorial, relating to technical issues with surgery given the considerations of size, and the attendant complications of prematurity. In addition, low weight at birth is also associated with other major congenital anomalies and being small for gestational age, both of which might adversely affect morbidity and mortality.
Different strategies for management have been employed to decrease the increased risk of morbidity and mortality in this population, including delaying surgery in an attempt to achieve a higher weight or, in amenable lesions, performing an initial palliative procedure instead of undertaking repair in single stage. These approaches share the underlying principle of waiting for a higher weight, and more mature post-menstrual gestational age of the infant. None has been shown to improve outcome, and some studies suggest that intervening mortality is higher,Reference Chang, Hanley, Lock, Castaneda and Wessel5 and significant morbidities are associated with the delay.Reference Reddy, McElhinney, Sagrado, Parry, Teitel and Hanley6 Thus, except in the most premature and the smallest infants, many centres, including ours, are now performing surgical repair early and, when possible, as a single stage.
In infants born at full term with normal weight, mortality has continued to improve with newer surgical techniques, modifications in bypass, and advances in peri-operative care. Previous studies have reported reasonable mortality for surgical repair of congenital cardiac disease in those born at low weight, albeit that few of these studies included many patients with functionally univentricular physiology, and fewer documented pre- and/or post-operative morbidities. The aim of our study is to describe the early morbidities, current rates of mortality, and risk factors for mortality in infants born with low weight and requiring surgery for congenital cardiac disease.
Methods
We carried out a retrospective review of the data from all infants born with low weight who had surgery for congenital cardiac disease during their initial hospitalization at The Children’s Hospital of Philadelphia from July, 2000, through July, 2004.
We identified the patients from our cardiothoracic database, obtaining information from the medical record. Institutional review board approval was obtained, with a waiver of informed consent. Criterions for inclusion were weight at birth less than or equal to 2500 grams, and congenital cardiac disease requiring surgery during the initial hospitalization. We excluded patients having isolated persistent patency of the arterial duct. Patients were classified as small for gestational age, appropriate for gestational age, or large for gestational age based on existing curves.Reference Battaglia and Lubchenco7 Prematurity was defined as gestational age less than 37 weeks. Major congenital anomalies included chromosomal aberrations, genetic syndromes, and other anomalies requiring surgery, such as duodenal atresia or cleft palate.
Data collected included preoperative, intraoperative, and postoperative variables. Necrotizing enterocolitis was divided into either suspected or definite based on criterions existing for staging.Reference Walsh and Kliegman8 An autopsy diagnosis of necrotizing enterocolitis was classified as definite. Infections were included if positive cultures, or polymerase chain reaction testing, were documented and treatment undertaken. Infections at the site of surgery included superficial and deep infections, with deep infections or mediastinitis requiring surgical debridement. Respiratory support was defined as days on mechanical ventilation and continuous positive airway pressure. Chronic lung disease was diagnosed and categorized according to the consensus definition of the National Heart, Lung and Brain Institute workshop.Reference Jobe and Bancalari9 Periventricular leukomalacia was defined as the presence of echogenic focuses or cystic lesions. Magnetic resonance imaging was used as the definitive test in those who had divergent results on ultrasound and magnetic resonance imaging. The ultrasonic investigation closest to discharge or death was used for diagnosis of periventricular abnormalities, while for intracranial hemorrhage we used the investigation showing the worst findings. Length of stay was defined by the number of days as in-patient on any service at our institution until discharge to home, transfer to an outside institution, or death. Cardiac lesions were categorized into one of four diagnostic classes using an anatomic classification, previously shown to correlate with mortality risk.Reference Clancy, McGaurn and Wernovsky10 Those in the first class are patients with 2 complete ventricles and no obstruction in the aortic arch. Those in the second class have 2 complete ventricles but an obstructed aortic arch. Those in the third class have functionally univentricular hearts in the absence of obstruction in the aortic arch, while those in the fourth class have both functionally univentricular hearts and obstruction of the aortic arch. Aorto-pulmonary shunts, and banding of the pulmonary trunk, were considered palliative procedures when they were performed as the initial surgery instead of a single-stage repair for patients having functionally bivenrtricular hearts. The initial stage of staged reconstruction procedures were performed with blood to the lungs supplied by a conduit placed from the right ventricle to the pulmonary arteries or a modified Blalock-Taussig shunt in those with functionally univentricular hearts.
Descriptive data is presented as the mean plus or minus the standard deviation for normally distributed data, and the median with the range in other circumstances. A univariate analysis was performed to identify risk factors of in-hospital mortality, using chi-squared analysis or Fisher’s exact test when appropriate for categorical and dichotomous variables. For continuous variables, comparisons were performed using Student’s t test for normally distributed data, or the Wilcoxon rank sum test otherwise. Risk factors found to be significant using a p-value of less than 0.15 by univariate analysis were placed into a stepwise, logistic regression model to identify independent risk factors of mortality. Statistical analysis was performed using STATA 9.2.
Results
Preoperative characteristics
Over the period of study, we found a total of 105 patients meeting the criterions for inclusion. The median weight at birth was 2130 grams, with a range from 431 to 2,500 grams. The median gestational age was 36 weeks, with a range from 25 to 41.1 weeks. Of the infants, 28 (27%) were small for gestational age. These infants had a similar birth weight, at 2038 as opposed to 2160 grams (p = 0.2), but higher gestational age at 37.6 versus 35 weeks (p < 0.001) than the infants born at a gestationally appropriate weight. None of the patients was large for gestational age. Of the group, 67 (64%) had been born prematurely, with 28 (27%) being less than 34 weeks gestation at birth. Distribution of diagnoses by the anatomic classification is shown in Table 1. Associated major congenital anomalies were seen in 32% of the population, with these diagnoses listed in Table 2.
Table 1 Diagnoses subdivided by anatomic classification.

Table 2 Major Congenital Anomalies.

Operative characteristics
The median age at surgery was 5 days, with a range from zero to 125 days, corresponding to a median post-menstrual gestational age of 37.1 weeks, with a range from 31.1 to 44.1 weeks. The median weight at surgery was 2190 grams, with a range from 1110 to 3004 grams. At the time of surgery, the infants who had been small for their gestational age weighed almost the same as those with appropriate gestational ages, at 2160 versus 2200 grams (p = 0.9), and were of a similar age, at 5 days versus 4 days (p = 0.9). The age at surgery according to diagnostic class is shown in Figure 1. Palliative procedures were performed in only 4 patients (8%) in those with functionally biventricular hearts. Aorto-pulmonary shunts were created in all patients with functionally univentricular hearts in the absence of obstructed aortic arches as the first operation for planned staged reconstruction. All those having obstructed aortic arches in the setting of functionally univentricular physiology underwent the initial stage of a staged reconstruction, except for one patient who had an operative balloon atrial septostomy at birth, but did not survive to the initial stage of a staged reconstruction. Operative support times by anatomic class are reported in Figure 2. Procedures on cardiopulmonary bypass were performed in 99 patients, with deep hypothermic circulatory arrest used in 78 patients.
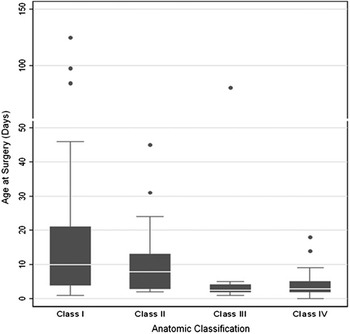
Figure 1 Box plot of age at surgery by anatomic classification. Solid line within box = median, box = width of interquartile range, error bars = furthest measurement within 1.5 interquartile range from the box, and circle = outlying measurement.

Figure 2 Box plot (a) of total support time by anatomic classification. Solid line within box = median, box = width of interquartile range, error bars = furthest measurement within 1.5 interquartile range from the box, and circle = outlying measurement. The box plot b is for deep hypothermic circulatory arrest and aortic cross-clamp time by anatomic classification. Solid line within box = median, box = width of interquartile range, error bars = furthest measurement within 1.5 interquartile range from the box, and circle or diamond = outlying measurement.
Mortality
Of the group, 80 patients (76%) survived to hospital discharge. Survival by anatomic classification is shown in Figure 3. Survival by birth weight can be seen in Table 3. We lost 3 patients during the operation. Identified precipitating factors for death include disseminated herpes infection in 1, aspergillus infection in 1, candidal infection in 1, an abdominal catastrophe in 2, intraventricular hemorrhage in 1, cardiac failure in 9, and multi-organ system failure in 10. Only 1 patient survived from the 9 patients with functionally univentricular hearts and obstructed aortic arches who required extracorporeal membrane oxygenation post-operatively. Death occurred in 7 patients after unsuccessful resuscitation from cardiac arrest, albeit that extracorporeal membrane oxygenation was not used in the resuscitation of these patients. In addition, of the 16 patients who initially survived a cardiac arrest, 10 ultimately died.

Figure 3 Box plot of survival by anatomic classification.
Table 3 Survival by birth weight and anatomic classification.

*No survival difference between birth weight groups by Fisher’s exact test, p = 0.48.
Risk Factors for Mortality
The association between demographic, pre-operative, operative, and post-operative variables and mortality is shown in Table 4. We used the significant variables found in this analysis to identify independent risk factors for mortality. Since the patients having obstructed aortic arches in the setting of a functionally univentricular heart were most strongly associated with mortality, we crested a variable in the model to identify these patients. Given the co-linearity between other significant intraoperative support variables, only total support time was entered into the model. Multiple stepwise logistic regression identified the need for cardiopulmonary resuscitation and extracorporeal membrane oxygenation as independent risk factors for mortality in this population (see Table 5).
Table 4 Univariate analysis for mortality.

*Any infection = bloodstream infection, urinary tract infection and surgical site infection.
†includes only time at the Children’s Hospital of Philadelphia.
Table 5 Multivariate analysis.

Morbidity
Neurologic
Preoperative brain imaging was most commonly performed using ultrasound and postoperative imaging more commonly included magnetic resonance imaging. The incidence of neurologic morbidities can be found in Table 6.
Table 6 Incidence of selected morbidities.

Numbers in parentheses represent the total number of patients available for analysis.
*Does not include 3 patients who died intraoperatively.
†Not all patients had head imaging.
The gestational age range of the patients who developed post-operative intraventricular hemorrhages graded at 3 or 4 was 31 to 39 weeks. No patients with intraventricular or parenchymal hemorrhages pre-operatively had progression identified post-operatively, though not all had post-operative imaging performed. In addition, of the 5 patients with periventricular echogenicities diagnosed preoperatively, 4 had postoperative head imaging in which only 2 patients had persistence of the periventricular echogenicities.
Infection
Blood stream infections were the most common type of infection both pre- and post-operatively. In 6 patients (5.7%) bacteraemia had been identified pre-operatively. All but one patient had coagulase negative staphylococcal infection associated with an in-dwelling venous catheter. The other patient with pre-operative bacteremia had early onset bacteremia with Escherichia coli. Post-operatively, blood stream infections occurred in 23 (23%) of the patients. Additional infections are listed in Table 6. In 8 patients, there had been 2 or more episodes of bacteremia. Mediastinitis requiring surgical debridement occurred in 6 patients, and 5 had superficial wound infections.
Necrotizing Enterocolitis
Suspected or definite post-operative necrotizing enterocolitis occurred in 19 (19%) of the patients. Of this group, only 5 had definite necrotizing enterocolitis as based on the criterions for staging.Reference Walsh and Kliegman8 No patients with necrotizing enterocolitis received surgical intervention. No patients with functionally biventricular hearts with unobstructed aortic pathways were diagnosed with necrotizing enterocolitis. The majority of patients (79%) with suspected and definite necrotizing enterocolitis had functionally univentricular hearts with obstruction of the aortic arch.
Respiratory Complications
Preoperative respiratory support had not been needed in 40 (38.1%) of the patients. The median length of pre and post-operative respiratory support, respectively, was 2 days, with a range from zero to 66 days, and 6 days with a range from zero to 108 days. Of the 30 patients less than 36 weeks gestation at birth, 13 (43.3%) met the criterions for the diagnosis of chronic lung disease.
Cardiac problems
Prostaglandin E1 had been administered pre-operatively in 78 patients (74.3%), the median length of treatment being 3 days, with a range from 1 to 66 days. No patient had required pre-operative extracorporeal membrane oxygenation. Preoperative cardiac catheterization was performed in 11 patients (10.5%), for diagnostic reasons in 7, to create atrial septal defects in 3, and unsuccessfully to balloon an aortic coarctation in the other. Extracorporeal membrane oxygenation was needed in 2 patients due to failure to separate from cardiopulmonary bypass in the operating room, while an additional 6 patients (5.7%) had intraoperative revision of the initial procedure. These revisions included modification of a systemic-to-pulmonary arterial shunt, and conversion from a single stage repair to the initial stage of a staged reconstruction.
Postoperatively, 11 patients (10.5%) required re-operations during their initial hospitalization. These operations included valvoplasties in 5, revised shunts in 4, closure of a residual ventricular septal defect in 1, and banding of a conduit placed from the right ventricle to the pulmonary arteries in the other. Postoperative catheterisations were required in 14 patients (13.3%), including 3 interventions to dilate recurrent coarctations, and 1 to place a stent in a modified Blalock-Taussig shunt. Extracorporeal membrane oxygenation was needed in 12 patients (11.7%) during their hospitalization, including 8 patients requiring extracorporeal oxygenation as a resuscitative effort due to a cardiac arrest. Overall, 23 patients (22%) had post-operative events requiring cardio-pulmonary resuscitation.
Length of stay
Total length of stay ranged from 1 to 134 days, with a median of 20 days. The median length of stay for patients whose entire hospitalization only occurred at our institution was 17 days, with a range from 1 to 134 days. Length of post-operative stay alone ranged from zero to 133 days, with a median of 16 days. We transferred 34 patients to an outside institution to complete their hospitalization. Effects of the presence of various morbidities on length of stay are shown in Table 7.
Table 7 Univariate analysis for length of stay

Discussion
The risk for death in infants born at low weight and undergoing surgery for congenital cardiac disease is significant, but improved in our cohort when compared to some other studies with similar populations and diagnoses. Previous studies have reported early mortality rates ranging from 10 to 42%.Reference Pawade, Waterson, Laussen, Karl and Mee4–Reference Reddy, McElhinney, Sagrado, Parry, Teitel and Hanley6, Reference Clancy, McGaurn and Wernovsky10–Reference Rossi, Seiden and Sadeghi15 Those reporting the lowest mortality, however, included no patients with functionally univentricular physiology, and all their patients were able to undergo surgery at a single stage.Reference Reddy, McElhinney, Sagrado, Parry, Teitel and Hanley6 Mortality was comparable for our patients having functionally biventricular hearts, at 10.2%. While this rate of death might be considered reasonable, it remains higher than the rate of death in the overall population of neonates undergoing surgery for congenital cardiac disease.
Factors such as being born with very low weight, less than 1500 grams, being small for gestational age, or having associated major congenital anomalies, have been hypothesized to be risk factors for mortality in the studied population. As have others,Reference Pawade, Waterson, Laussen, Karl and Mee4, Reference Dees, Lin, Cotton, Graham and Dodd12, Reference Reddy and Hanley13 however, we failed to find a statistically significant effect for these risk factors on mortality. It is likely that, as in our study, few infants in the lowest gestational age and lowest weights at birth had severe forms of congenital cardiac disease, as many of those infants do not survive to repair, or are not offered repair due to extreme prematurity. Infants who are small for gestational age have been reported to have increased risk for mortality and morbidity when compared to controls matched for gestational age.Reference Simchen, Beiner and Liviathan16–Reference Aucott, Donohue and Northington19 These infants in our study, however, were of lower weight but more mature, by gestational age, both at birth and at the time of surgery compared to patients born for appropriate gestational age. While being small for gestational age was not a statistically significant variable associated with increased survival, the patients who were small for gestational age, at 18%, trended toward lower mortality than those who were appropriate for gestational age, at 26%. The only other study that reported on the outcome of patients with congenital cardiac disease who were small for their gestational age also reported lower rates of mortality in those born at term.Reference Oppido, Napoleone and Formigari14 It is tempting to purport that this decreased mortality is due to this population being more mature, perhaps suggesting gestational age is a more important risk factor for poor outcome than weight. To date, however, no studies have had significant power to explore this relationship. As for associated anomalies, there have been contradictory reports of their influence on the risk for death in the studied population.Reference Reddy, McElhinney, Sagrado, Parry, Teitel and Hanley6, Reference Numa, Butt and Mee11, Reference Dees, Lin, Cotton, Graham and Dodd12, Reference Oppido, Napoleone and Formigari14 The difference in reported outcomes in this population could be related to different philosophies in aggressiveness of care, or to a bias in the selection of those patients offered operative repairs.
Another significant risk factor for mortality is having a diagnosis of hypoplastic left heart syndrome, or a variant thereof. A recent metanalysis has also demonstrated that diagnosis is a predictor of mortality in infants who undergo surgery when weighing less than 2500 grams.Reference Abrishamchian, Kanhai, Zwets, Nie and Cardarelli20 Mortalities of 45 to 51% have been reported in such infants undergoing staged reconstruction for hypoplastic left heart syndrome and its variants.Reference Pizarro, Davis, Galantowicz, Munro, Gidding and Norwood21, Reference Weinstein, Gaynor and Bridges22 The mortality in our population with these lesions was 38.3%, thus paralleling the historical trend of improving outcomes in infants with hypoplastic left heart syndrome. This mortality, nonetheless, is still much higher than current reported survival, of 85%, for the overall population of infants with hypoplastic left heart syndrome.Reference Tabbutt, Dominguez and Ravishankar23
We found the use of extracorporeal membrane oxygenation and the need for cardiopulmonary resuscitation to be the only statistically significant risk factors for mortality after multivariate logistic regression analysis. There was also a trend for delayed sternal closure to be associated with mortality, which is not surprising given that delayed sternal closure was not performed routinely, and was selectively performed to optimize haemodynamics or in cases with significant bleeding in order to prevent tamponade physiology. Extracorporeal membrane oxygenation was not used as a routine therapy in patients with obstructed aortic arches and functionally univentricular physiology after their initial surgery. Thus, those patients who required extracorporeal membrane oxygenation were patients who either were not able to be weaned from cardiopulmonary bypass in the operating room, were placed on extracorporeal membrane oxygenation as resuscitative therapy for deteriorating haemodynamics, or after a cardiac arrest. Given the high risk of mortality in this population of patients that require extracorporeal membrane oxygenation, and the associated costs and high resource utilization with this procedure, it will be important to investigate if there are identifiable characteristics that could distinguish those surviving the intervention as opposed to those who do not. Perhaps not surprisingly, another study has also reported the need for resuscitation post-operatively to be associated with mortality.Reference Beyens, Biarent and Bouton24 While other factors were not found to influence mortality, several morbidities were found to impact length of stay. Some of these morbidities such as chronic lung disease and infections are preventable with appropriate strategies. Thus, while mortality may not be significantly affected with decreasing these morbidities, hospital costs and resource utilization could be affected positively.
Our study has its limitations, including the small number in our cohort, albeit greater than previously published, and the inability to follow patients after inter-hospital transfer from our institution, thus making it possible that the rate of death may in fact be higher than our in-hospital mortality. In addition, we did not collect data on those patient born with low weight who did not survive to undergo a cardiac operation, nor those patients who were not offered surgical repairs. Another limitation was our method of identifying patients, using a database that only included weight at time of surgery. Thus, patients who were born with low weight, but who weighed more than 2500 grams at the time of surgery, may not have been included in our study.
We can conclude, nonetheless, that while the mortality of infants with congenital cardiac disease born with low weight is high, it is acceptable and perhaps improving, especially in the subgroup of patients with hypoplastic left heart syndrome. The overall survival for our patients is similar to that reported for patients who have a birth weight between 701 and 800 grams,Reference Fanaroff, Stoll and Wright25 and is higher than levels of mortality usually used to assess decisions concerning viability. Weight and gestational age should not be a hindrance to referral of these infants for surgery at a cardiac centre. Given the lack of evidence to suggest that delaying surgery is beneficial, these referrals should be made early. In addition, strategies to avoid morbidities should be employed to help decrease the length of stay, and thus hospital costs.
Acknowledgement
None of the authors have financial disclosures or conflicts of interest to report.












