The normal aortic valve is composed of the three semilunar valves. According to the position of valve and coronary ostia, it can be divided into left, right, and none coronary valve. However, bicuspid aortic valve usually consists of two valves with different sizes, which is the most common CHD, with an incidence of 1%–2% in the population. Reference Hoffman and Kaplan1,Reference Borger, Fedak and Stephens2 Sievers et al had introduced a classification system based on the number of the raphes and spatial position of cusps. Reference Sievers and Schmidtke3 Although bicuspid aortic valve patients have no obvious symptoms in the early stage, they will gradually suffer from aortic stenosis or insufficiency, endocarditis, aortic aneurysm, aortic dissection, and other complications with the increase of age. Reference Siu and Silversides4
Most bicuspid aortic valve patients with aortic dilation need to perform surgical procedures, such as aortic valve replacement and ascending aortic replacement or angioplasty. At present, all surgical strategies are mainly based on the maximum ascending aortic diameter. Reference Hiratzka, Creager and Isselbacher5 Due to the hemodynamics and pathophysiological changes affected by genetics, the surgical strategy for BVA patients is limited only by ascending the aortic diameter. Reference El-Hamamsy and Yacoub6 Some studies have shown that the valve function of bicuspid aortic valve patients may have a greater impact on the occurrence of aortic adverse events after aortic valve replacement than ascending aorta diameter. Reference Girdauskas, Rouman and Disha7,Reference Girdauskas, Disha and Raisin8 Therefore, more indicators to guide the current surgical strategy are needed to explore.
In the present study, we aimed to evaluate the mid-term outcome of aortic valve replacement for bicuspid aortic valve or tricuspid aortic valve and the related risk factors by propensity score-matched analysis.
Patients and methods
Patients
This is a retrospective study. A total of 278 patients who underwent aortic valve replacement from January 2014 to June 2019 in the Second Affiliated Hospital (Xinqiao Hospital) of Chinese People’s Liberation Army Medical University were included. They were divided into tricuspid aortic valve and bicuspid aortic valve groups (177 in tricuspid aortic valve group and 101 in bicuspid aortic valve group). In the bicuspid aortic valve group, there were 17 patients with Type 0 Ap (Anterior-posterior), 24 with Type 0 Lat (Lateral), 54 with Type 1, and 6 with Type 2. Inclusion criteria were adult patients (age ≥18 years); patients with ascending aorta diameter ranging from 35 to 50 mm; and all bicuspid aortic valve types were confirmed by echocardiography and intraoperative exploration. Exclusion criteria were patients who were diagnosed with infective endocarditis, Marfan syndrome, or connective tissue disease and patients who died during perioperative period. Aortic adverse events were defined as reoperation and sudden cardiac death. The follow-up time was the time from the first aortic valve replacement to the occurrence of aortic adverse events. If not, it was calculated to 31 June, 2020. The clinical data of all patients were obtained from the Digital Medical Record Review System by surgeons.
Surgical procedures
All aortic valve replacement procedures were performed by experienced cardiac surgeons according to a standardised technique, which involved median sternotomy incision, cardiopulmonary bypass, perfusion with cold blood cardioplegia, and replacement with proper mechanical valve size.
After operation, patients were routinely given therapy. Postoperative treatment included anticoagulation, antibiotic usage, nourishing cardiac muscle, blood pressure control, blood glucose control, and other symptomatic supportive measures. During follow-up, transthoracic echocardiography was used to assess the heart function and valve function and to detect the postoperative ascending aorta.
Propensity score matching
The 1:1 propensity score matching analysis was used to adjust the treatment selection bias and possible imbalances in baseline characteristics between patients in the two groups. The propensity score for an individual was calculated according to the covariates of gender, age, body mass index, smoking, drinking, hypertension, diabetes mellitus, coronary artery disease, valve function, left atrial diameter, left ventricle diameter, aortic sinus diameter, ascending aorta diameter, fractional shortening, left ventricular ejection fraction, and Euro Score II using a multivariable logistic regression model. Reference Nashef, Roques and Sharples9 First, random ordering the bicuspid aortic valves and tricuspid aortic valves. Second, selecting the bicuspid aortic valve subject and finding the tricuspid aortic valve subject with the closest propensity score. Finally, we tested the multiple calliper widths. A calliper width of 0.2 resulted in the best trade-off between homogeneity and retained sample size. The propensity score matching analysis was conducted using the SPSS statistical software (IBM SPSS Statistics version 25.0 for Windows; IBM, New York, United States of America).
Statistical analysis
The statistical analyses were conducted using the SPSS statistical software (IBM SPSS Statistics version 25.0 for Windows; IBM, New York, United States of America). Measurement data were expressed as means ± standard derivation if they were normally distributed, or median values (interquartile range) if not. Comparisons between the two groups were performed using t-tests for normally distributed variables or Mann–Whitney U-test for variables without normally distributed. Counting data were expressed as frequencies and percentages (%) and were compared using Pearson’s χ2 test or Fisher’s exact test, as appropriate. Univariate logistic regression analysis was used to compare propensity score matching follow-up cohort in terms of their preoperative clinical characteristics. Variables with p < 0.2 in the univariate logistic regression analysis and other variables which were considered likely to have important prognostic values were then included in a multivariate logistic regression analysis. Multivariate logistic regression analysis was performed using enter model with entry criteria of p < 0.05 and exit criteria of p < 0.1. Results were tabulated as odds ratios with 95% confidence intervals. All statistical tests were two-tailed, with statistical significance when p < 0.05.
Results
Propensity score matching analysis included 80 pairs of patients (n = 160), and the baseline characteristics between bicuspid aortic valve group and tricuspid aortic valve group were matched (Table 1). Moreover, there was no statistical difference in intraoperative and postoperative outcomes between the propensity score matching cohort (Table 2). A total of 137 patients in propensity score matching cohort were followed up, and the loss rates in bicuspid aortic valve and tricuspid aortic valve groups were 12.50% and 16.25%, respectively. The median follow-up time was 43 months, with interquartile range of 26.50–58.00 months. During follow-up, there were no significant differences in the diameter of aortic sinus, the diameter difference of aortic sinus, and annual variation of aortic sinus diameter between bicuspid aortic valve and tricuspid aortic valve groups (p = 0.593, p = 0.379 and p = 0.457, respectively). Meanwhile, the incidence of aortic adverse events, the velocity of mechanical prosthetic valve, the peak pressure difference across the valve, the mechanical prosthetic valve function, and New York Heart Association functional class were statistically similar between bicuspid aortic valve and tricuspid aortic valve groups (Table 3). Although the ascending aorta diameter between the two groups did not differ on the whole (Fig 1), patients with bicuspid aortic valve were associated with a larger diameter difference of ascending aorta (p = 0.003), a larger annual variation of ascending aorta diameter (p = 0.002), and a higher rate of ascending aorta continued to enlarge (p = 0.030) comparing with patients with tricuspid aortic valve (Table 3, Figs 1 and 2).
Table 1. Patient characteristics

AAO = ascending aorta; AS = aortic valve stenosis; AR = aortic valve regurgitation; Both = AS and AR; BAV = bicuspid aortic valve; BMI = body mass index; FS = fractional shortening; IQR = interquartile range; LA = left atrial; LV = left ventricle; LVEF = left ventricular ejection fraction; M = median; PSM = propensity score matching; SD = standard deviation; TAV = tricuspid aortic valve.
Data were expressed as n (%), mean ± SD, or M (IQR)
Statistically significant (p < 0.05) values are in bold
Table 2. Procedural characteristics and perioperative outcomes in PSM cohort
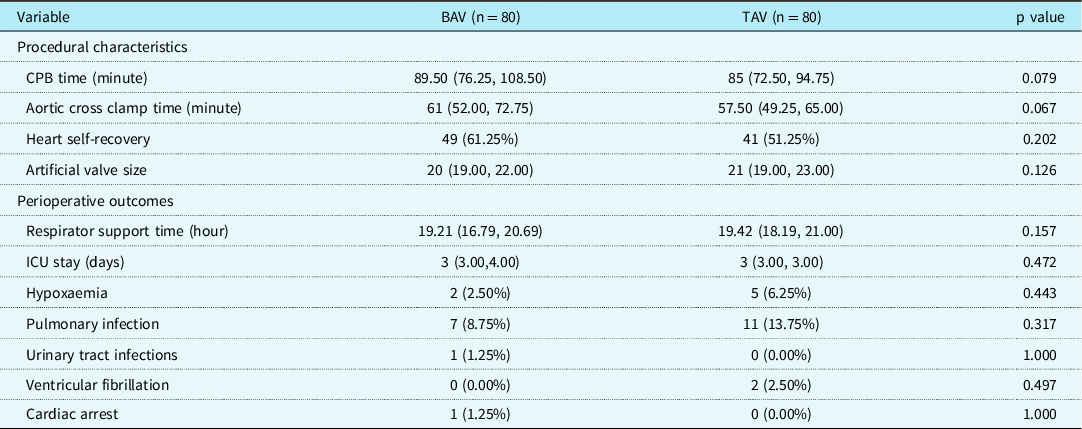
BAV = bicuspid aortic valve; CPB = cardiopulmonary bypass; ICU = intensive care unit; IQR = interquartile range; M = median; PSM = propensity score matching; TAV = tricuspid aortic valve.
Data were expressed as n (%), or M (IQR)
Statistically significant (p < 0.05) values are in bold
Table 3. Follow-up data of PSM follow-up cohort

BAV = bicuspid aortic valve; IQR = interquartile range; M = median; NYHA = New York Heart Association functional class; PSM = propensity score matching; SD = standard deviation; TAV = tricuspid aortic valve
Data were expressed as n (%), mean ± SD, or M (IQR)
Statistically significant (p < 0.05) values are in bold

Figure 1. Comparison of ascending aorta diameter and changes in propensity score matching (PSM) follow-up cohort (tricuspid aortic valve (TAV): n = 67; bicuspid aortic valve (BAV): n = 70). (a) Comparison of AAO diameter between TAV and BAV groups before aortic valve replacement (AVR). (b) Comparison of AAO diameter between TAV and BAV groups at follow-up. (c) Comparison of AAO diameter difference between TAV and BAV groups. (d) Average annual variation of AAO diameter between TAV and BAV groups. NS: the difference between TAV group and BAV group was not statistically significant (p > 0.05); *the difference was statistically significant (p < 0.05).

Figure 2. Comparison of ascending aortic dilatation between tricuspid aortic valve (TAV) and bicuspid aortic valve (BAV) groups in propensity score matching (PSM) follow-up cohort (TAV: n = 67; BAV: n = 70). During the follow-up, the number of people whose ascending aorta continued to dilate was shown in the black column, if not, it was shown as a grey column. *the difference was statistically significant (p < 0.05).
Among 10 variables included in the logistic model of the propensity score matching follow-up cohort, valve classifications and valve functions were statistically significant between the two groups. The risk of ascending aorta continued to enlarge in type 1 bicuspid aortic valve group was 5.173 times higher than that tricuspid aortic valve group (p = 0.003). In contrast to the simple valvular stenosis, the risks of ascending aorta continued to enlarge in patients with valvular regurgitation alone or valvular stenosis merging regurgitation were higher up to 3.673 and 6.489 times, respectively (p = 0.030 and p = 0.006, respectively) (Table 4).
Table 4. Logistic regression analysis of propensity score matching (PSM) follow-up cohort

Furthermore, bicuspid aortic valve cohort (n = 70) was screened out from the propensity score matching cohort. Five variables were included in the logistic model of the bicuspid aortic valve cohort. Moreover, the results showed that Type 1 in bicuspid aortic valve (OR 5.157; 95% CI 1.053, 25.272; p = 0.043), age ≥ 40 years (OR 6.956; 95% CI 1.228, 39.410; p = 0.028), and pure aortic regurgitation (OR 4.322; 95% CI 1.174, 15.911; p = 0.028) were independent risk factors for the continued dilation of the ascending aorta in bicuspid aortic valves (Table 5).
Table 5. Logistic regression analysis of bicuspid aortic valve (BAV) group in propensity score matching (PSM) follow-up cohort

Discussion
It has been reported that the incidences of root dilation and ascending aorta dilatation are about 35% and 42% in bicuspid aortic valves, respectively. Reference Masri, Kalahasti and Alkharabsheh10 A guideline suggests that the absolute threshold of ascending aorta diameter in bicuspid aortic valves is more than 50 mm, while there is no strict regulation for moderate ascending aortic dilatation (45–50 mm) due to the low level of evidence (IIb/C). Reference Hiratzka, Creager and Isselbacher5 At the same time, whether the normal to mildly dilated ascending aorta (d ≤ 45 mm) in bicuspid aortic valves should be treated is also not specified. This guideline is mainly based on the study of Boger et al in 2004. Reference Borger, Preston and Ivanov11 They found that the rate of 15-year free from ascending aorta-related complications was 86%, 81%, and 43% in bicuspid aortic valves with the aortic diameter of <40 mm, 40–44 mm, and 45–49 mm after aortic valve replacement, respectively. It suggested that not all patients with bicuspid aortic valves will experience continued dilatation of the ascending aorta or even adverse aortic events after aortic valve replacement. For patients with bicuspid aortic valves at high risk of continued aortic dilatation, attention should be paid to treating the ascending aorta. Therefore, it is of great clinical significance to find out the influencing factors about ascending aorta continued dilatation in patients with bicuspid aortic valves.
As far as we know, our study is the first one to investigate the efficacy of aortic valve replacement on bicuspid aortic valves and the influencing factors based on the propensity score matching analysis. Moreover, we fully considered the characteristics of patients, including age, gender, past medical history, valve fusion difference, and valve function. Mahadevia et al found that different types in bicuspid aortic valves led to different hemodynamics, which resulted in different patterns of aortic dilatation. Reference Mahadevia, Barker and Schnell12 The aortic valves of bicuspid aortic valves were replaced with standard mechanical valves after aortic valve replacement, and the hemodynamics had been significantly improved, while our results showed that the risk of continued aortic dilatation in patients with type 1 bicuspid aortic valves was significantly higher than patients with other bicuspid aortic valve types and tricuspid aortic valve. Furthermore, preoperative aortic regurgitation alone and aortic stenosis with regurgitation were associated with a higher risk of continued aortic dilatation compared with valve stenosis alone in the propensity score matching follow-up cohort. We then screened patients with bicuspid aortic valves from the propensity score matching cohort. We found that patients with preoperative aortic regurgitation had a significantly increased risk of continued aortic dilatation after aortic valve replacement. Therefore, the types of bicuspid aortic valves, the function of aortic valve before operation, or other persistent factors may play an important role in the continuous dilatation of the ascending aorta after operation, which is similar to the results of Yasuda et al Reference Yasuda, Nakatani and Stugaard13 and Wang et al Reference Wang, Wu and Li14 .
According to the study of Chim et al, the aortic wall compliance was worse and the spatial distribution of elastin was significantly different in bicuspid aortic valves in comparison with tricuspid aortic valves. Reference Chim, Davies and Mason15 This may be the reason why the ascending aorta of bicuspid aortic valves is more likely to continue to dilate. Moreover, the primary pathological process of aortic aneurysm formation is the loss of aortic smooth muscle cells and the degradation of extracellular matrix, which has been widely accepted in recent years. Reference Maguire, Pearce and Xiao16 Matrix metalloproteinase is considered to be the most important enzyme in the degradation of extracellular matrix. Reference Rabkin17 Ikonomidis et al found that the content and activity of matrix metalloproteinases in the ascending aorta in type 1 bicuspid aortic valves were significantly higher than those in normal aortic tissues, indicating that type 1 bicuspid aortic valves may be more prone to the dilatation of ascending aorta. Reference Ikonomidis, Ruddy and Benton18 This finding was similar to the results of our study. In physiological conditions, the diameter of the ascending aorta will gradually increase with age in both healthy individuals and bicuspid aortic valves. Reference Biaggi, Matthews and Braun19,Reference Stock, Mohamed and Sievers20 Therefore, not only the diameter of the ascending aorta but also age should be considered in operation determination. Our study showed that the risk of continued dilatation of the ascending aorta after aortic valve replacement was significantly higher when age was 40 years or older in bicuspid aortic valves. It may be related to the weakening of extensibilities in the aortic wall due to ageing. Reference Deveja, Iliopoulos and Kritharis21
There are also several limitations of the current study. First, although the interference of confounding factors had been reduced by propensity score matching, some bias existed unavoidably in this retrospective study. For example, aortic valve replacement was not performed by the same surgeon. Second, the accuracy of measuring vessel diameter with echocardiography may be lower than that of CT angiography or MRI, but it is still the most important method in preoperative examination and follow-up review. Reference Nishimura, Otto and Bonow22,Reference Elefteriades, Mukherjee and Mojibian23 Finally, we did not perform a more precise classification of type 1 bicuspid aortic valves because it required a larger sample size.
Conclusion
In conclusion, during the follow-up with 43 months, there was no significant difference in the incidence of aortic adverse events between patients with bicuspid aortic valves and tricuspid aortic valves and their ascending aortic diameter was between 35 and 50 mm. Therefore, aortic valve replacement is still a safe and effective surgical method after mid-term follow-up. However, type 1 bicuspid aortic valves, age ≥ 40 years, and aortic regurgitation are independently and positively correlated with the continued dilation of ascending aorta after aortic valve replacement. Therefore, for patients with bicuspid aortic valves combined with the above risk factors, appropriate treatment of ascending aorta should be simultaneously considered during aortic valve replacement, such as ascending aortic angioplasty, ascending aortic wrapping, Bentall, so as to reduce the risk of long-term dilation and even dissection of ascending aorta.
Acknowledgements
This study was approved by the Medical Ethics Committee of Second Affiliated Hospital of Army Medical University, PLA (No. 2020-YANDI113-01).
Financial support
This study was funded by the Project of Chongqing Science Committee (csts2015shmszx120088) and the Project of Chinese People’s Liberation Army Medical University (CX2019JS216).
Conflicts of interest
None.










