CHD is the most common birth defect, occurring in ~8 per 1000 births (0.8%) in the Western world.Reference Goossens, Stephani and Hilderson 1 Historically, 20–40% of children born with CHD were expected to survive into adulthood.Reference Macmahon, McKeown and Record 2 , Reference Zomer, Vaartjes, Grobbee and Mulder 3 As a result of advances in diagnostic methods and improved management of infants and children with complex CHD, the profile of those living with CHD is rapidly changing. The median age of patients with severe-complexity CHD increased from 11 years in 1985 to 17 years in 2000.Reference van der Bom, Zomer, Zwinderman, Meijboom, Bouma and Mulder 4 , Reference Marelli, Mackie, Ionescu-Ittu, Rahme and Pilote 5 Over 90% of those born with CHD now reach adulthood. In a landmark medical achievement, the number of those living with adult CHD exceeded that of children with CHD in 2000, and now approaches a ratio of 2:1 with >2.5 million adult CHD patients in North America and Europe.Reference Goossens, Stephani and Hilderson 1 , Reference Zomer, Vaartjes, Grobbee and Mulder 3 , Reference Vis, van der Velde and Schuuring 6 – Reference Rodriguez and Marelli 9
As the adult CHD population continues to grow, effective long-term care of these patients presents a significant challenge. Comprehensive adult CHD care not only entails ongoing medical management of sequelae of both congenital and acquired disease but also requires navigation of the complex transition process from paediatric to adult healthcare systems. Guidelines on the indications for, and frequency of, follow-up recommend that most adult CHD patients, even those with simple lesions, warrant ongoing evaluation by a cardiologist.Reference Warnes, Williams and Bashore 10 , Reference Mackie, Ionescu-Ittu, Therrien, Pilote, Abrahamowicz and Marelli 11
Lack of follow-up in adolescents and adults with CHD is a major concern. Factors that lead to lack of follow-up and poor transition have been investigated within universal healthcare paradigms in Europe and Canada.Reference Zomer, Vaartjes, Grobbee and Mulder 3 , Reference Vis, van der Velde and Schuuring 6 , Reference Mackie, Ionescu-Ittu, Therrien, Pilote, Abrahamowicz and Marelli 11 – Reference Mackie, Rempel, Rankin, Nicholas and Magill-Evans 14 Gaps in medical surveillance have been documented in up to 30–70% of those with CHD, leading to increased morbidity and mortality.Reference Zomer, Vaartjes, Grobbee and Mulder 3 , Reference Vis, van der Velde and Schuuring 6 , Reference Mackie, Ionescu-Ittu, Therrien, Pilote, Abrahamowicz and Marelli 11 , Reference Yeung, Kay, Roosevelt, Brandon and Yetman 12 , Reference Gurvitz, Inkelas, Lee, Stout, Escarce and Chang 15 – Reference Moons, Hilderson and Van Deyk 17 American centres have reported lapses in care of >3 years in 21–61% of adult CHD patients who eventually return to cardiology care.Reference Yeung, Kay, Roosevelt, Brandon and Yetman 12 , Reference Gurvitz, Valente and Broberg 18 Discontinuity of care during the transition between paediatric to adult providers has been linked to multiple factors including patient, provider, healthcare, systemic, and economic factors. Most notable among these factors are inadequate patient and family preparation for transition, cognitive and/or psychosocial impairments, patient–provider attachment, inadequate programme integration, and poor access to adult speciality care.Reference Gurvitz, Valente and Broberg 18 , Reference Roberta 19
It is crucial to optimise the transfer of patients with CHD from paediatric to adult healthcare services to preclude loss of medical continuity resulting in preventable morbidity and mortality. Appropriate and timely transition plays a central role in the future health of these patients. We sought to describe the factors leading to poor follow-up within a high-volume single centre.
Methods
Study design and population
All patients aged 16–17 years with CHD that had been seen for an ambulatory paediatric cardiology visit in 2003 at a single tertiary care institution in the United States of America were considered. The study was conducted in accordance with, and approved by, the local Institutional Review Board. A waiver for documentation of consent was granted to allow verbal informed consent for participation. Patients with primary International Classification of Diseases, Ninth Revision (ICD-9) codes for predefined CHD lesions were included. Exclusion criteria included documented developmental delay or significant intellectual disability at the time of index visit. All patients were stratified by CHD lesion complexity into four subgroups – simple, moderate, severe, and unclassified – derived from categorisations established during the 32nd Bethesda Conference.Reference Warnes, Williams and Bashore 10 When appropriate, secondary ICD-9 diagnoses were used to accurately categorise patients. In cases in which patients carried more than one ICD-9 code for CHD, classification was based on the lesion of greatest severity. Lesions not explicitly represented within the guidelines were labelled unclassified. Maintenance of care was defined as at least one ambulatory assessment by a cardiac provider within the same healthcare system <3 years after index visit. Loss of follow-up was defined as no documented ambulatory visits with a cardiac provider within the same healthcare system for ⩾3 years at the time of chart review.
A retrospective, cross-referenced review using the hospital electronic medical record was performed to gather demographic information including age and gender of all study patients. The last documented cardiac visit and type of cardiac provider seen – paediatric, adult, or adult CHD – was recorded.
Attempts to personally contact all patients, including those with loss of follow-up, were made by the authors using a multi-tiered protocol. Investigators were blinded to the presence or absence of loss of follow-up. Initial attempts used the documented telephone number. If the patients were no longer living at that residence, alternate contact numbers were obtained from family members or prior guardians. If no contact was made or if numbers were disconnected or non-functioning, a focused chart review was performed to locate alternate contact numbers. A standardised recording was left on voicemail or answering machines when appropriate. A dedicated study telephone line was created and was made available for patients to call at any time after receiving a recorded message. If no contact was made, the aforementioned steps were repeated three times until all avenues to contact the patient were exhausted. After verbal informed consent, a standardised telephonic survey was administered to patients who were successfully contacted. Questionnaire topics were developed with the intent to assess demographic information, as well as multiple aspects of CHD care, knowledge, and commonly encountered barriers to CHD care (Table 1). Answers were collected in a yes/no or multiple-choice manner.
Table 1 Questionnaire topics.

ACHD=adult CHD; PCP=primary care provider
Statistical analysis
Cochran–Armitage trend test was used to examine the relationship between loss of follow-up and the following variables: gender, complexity of CHD, and type of cardiac provider last seen. Questionnaire answers were aggregated and reduced to binary values within 15 distinct categories, creating a framework that allowed statistical analysis. Answers were analysed as categorical variables using both χ2 test and Fisher’s exact test, with p-value<0.05 considered statistically significant. Categorical variables are represented as percentages, and continuous variables as means and standard deviations (SD). Data are reported as means with SD or numbers with percentages (%). All analyses were performed using SAS software version 9.21 (SAS Institute Inc., Cary, North Carolina, United States of America).
Results
A total of 5874 eligible ambulatory cardiac patients were evaluated, of whom 197 (3.3%) met the inclusion criteria. Baseline characteristics including primary CHD diagnosis are described in Table 2. The group was 54% male. Mean age was 25 (SD 1.0) years. Anatomic classification of CHD complexity categorised 35.6% of patients as simple (n=70), 42.1% as moderate (n=83), 14.7% as severe (n=29), and 7.6% as unclassified (n=15) defects (Fig 1). Patients had last received care from a variety of cardiology providers. The majority (62%) of patients were last seen by a paediatric cardiologist. Only 34% had transitioned to an adult CHD provider within the system (Fig 2).

Figure 1 Distribution of lesion severity.
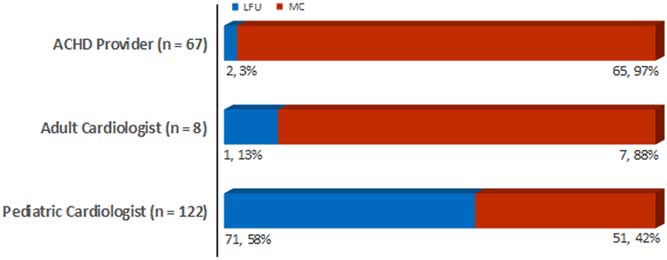
Figure 2 Follow-up trends, by last cardiac provider seen. ACHD=adult CHD; LFU=loss of follow-up; MC=maintenance of care.
Table 2 Baseline patient characteristics.

AVSD=atrioventricular septal defect; HOCM=hypertrophic obstructive cardiomyopathy; PDA=patent ductus arteriosus; RVOT=right ventricular outflow tract; VSD=ventricular septal defect
Loss of follow-up, defined as no ambulatory cardiac visits within the single healthcare system for a period of ⩾3 years, was seen in 74 of 197 patients (37.6%) (Fig 3). Most patients with loss of follow-up could not be successfully contacted, and their status is unknown. Higher complexity of CHD was associated with maintenance of care (p=0.0114). A significant association was also noted with respect to last cardiac provider seen: patients who had successfully transitioned into the care of adult CHD providers were most likely to maintain continuity (p<0.001).

Figure 3 ( a ) Enrolment algorithm. ( b ) Enrolment algorithm, by maintenance of care (MC) and loss of follow-up (LFU).
Surveyed patients
Successful contact was made with 78 (39.6%) of 197 patients (Fig 3). Three (1.5%) patients were excluded after contact owing to previously undocumented developmental or cognitive delays, and nine patients (4.6%) declined participation. In all, 58 patients answered the questionnaire. This group comprised those with maintenance of care (n=42) and those with loss of follow-up (n=16), as determined by chart review (Fig 3). The mean age was 24 (SD 1.2) years, with 41.4% males (n=24). Simple-complexity lesions were present in 16 patients (27.6%), moderate complexity in 26 patients (44.8%), severe complexity in 11 patients (19%), and unclassified defects in five patients (8.6%). A summary of questionnaire answers is found in Table 3. Only half (53.4%) of the patients were able to accurately name their CHD lesion. Maintenance of care was associated with the use of prescription cardiac medications (p=0.0009) and female gender (p=0.021). Discussions with providers specifically regarding employment plans (p=0.0027) and the importance of long-term follow-up (p=0.034) were also associated with maintenance of care. Discussion between providers and patients regarding insurance and disability benefits (p=0.08) or the presence of lapses in current or prior insurance coverage (p=0.08) were not found to be statistically significant factors associated with loss of follow-up.
Table 3 Questionnaire demographics and answers of surveyed patients (n=58).

ACHD=adult CHD; LFU=loss of follow-up; MC=maintenance of care
NS=not significant (p⩾0.05)
* Financial, pre-existing condition, poor work coverage
Deceased patients
In total, eight patients (4.1%) were deceased, half of whom had severe-complexity CHD. Details regarding the circumstances of death were elicited from family members (Table 4). The majority (63%) of deaths were due to known sequelae of CHD, including arrhythmias, heart failure, and pulmonary hypertension. Three (38%) of the deceased patients belonged to the group with loss of follow-up.
Table 4 Circumstances and cause of death in deceased patients (n=8).

LFU=loss of follow-up
Discussion
The ageing and expanding adult CHD population brings new challenges. This single-centre study describes the rates of, and factors leading to, loss of follow-up and maintenance of care in adolescents with CHD as they enter adulthood. A disproportionately small number of these patients currently receive appropriate medical surveillance.Reference Yeung, Kay, Roosevelt, Brandon and Yetman 12 Up to 70% of patients with CHD experience lapses in care after leaving paediatric care, and prior large-scale studies within universal healthcare systems suggest that many patients who do not maintain follow-up are likely lost to care.Reference Mackie, Ionescu-Ittu, Therrien, Pilote, Abrahamowicz and Marelli 11 , Reference Yeung, Kay, Roosevelt, Brandon and Yetman 12 , Reference de Bono and Freeman 16 – Reference Gurvitz, Valente and Broberg 18 , Reference Reid, Irvine and McCrindle 20 Identification of factors that lead to poor continuity is imperative to address the high rates of interrupted care in this population. There has been a wide variation in reported percentages of patients with lapses in care or loss of follow-up, partly driven by substantial differences in definition of study criteria and variable study populations and recruitment methods. Within our single centre, 74 of 197 patients (37.6%) had loss of follow-up.
The adult CHD population is heterogeneous, ranging from those with mild defects requiring little or no intervention to severe-complexity lesions. The distribution of CHD severity in our population is similar to previously published estimates.Reference Marelli, Mackie, Ionescu-Ittu, Rahme and Pilote 5 , Reference Warnes, Liberthson and Danielson 7 Most patients with adult CHD require periodic assessment owing to potential need for re-intervention and risk of premature death, arrhythmias, endocarditis, pulmonary hypertension, or heart failure.Reference Goossens, Stephani and Hilderson 1 , Reference Zomer, Vaartjes, Grobbee and Mulder 3 , Reference Yeung, Kay, Roosevelt, Brandon and Yetman 12 , Reference Iversen, Vejlstrup, Sondergaard and Nielsen 21 , Reference Foster, Graham and Driscoll 22
Uninterrupted healthcare should continue in the period spanning adolescence to adulthood.Reference Goossens, Stephani and Hilderson 1 , Reference Warnes, Liberthson and Danielson 7 , Reference Warnes, Williams and Bashore 10 , Reference Foster, Graham and Driscoll 22 – Reference Deanfield, Thaulow and Warnes 24 Successful implementation of a transition process requires purposeful movement of adolescents and young adults from child-centred to adult-oriented healthcare systems. This is integral to minimise morbidity and mortality.Reference Goossens, Stephani and Hilderson 1 , Reference Warnes, Williams and Bashore 10 , Reference Gurvitz, Valente and Broberg 18 – Reference Reid, Irvine and McCrindle 20 , Reference Foster, Graham and Driscoll 22 , Reference Moons, Pinxten and Dedroog 23 , Reference Kirk 25 – Reference Knauth, Verstappen, Reiss and Webb 27 Most cardiology programmes do not have formal transition programmes.Reference Hilderson, Saidi and Van Deyk 28 An informal transition programme was in place at our institution at the time of enrolment that encouraged transition of care to adult CHD providers in early adolescence. This allowed variability based on patient, family, and paediatric cardiac provider’s preference. Despite shared adult CHD and paediatric cardiology clinic space, nearly 1/3 of patients had loss of follow-up with lapses of care ⩾3 years as they entered young adulthood. Although superior to international estimates of attrition that approach 75% in some cases, this represents a sizable portion of patients with suboptimal transition and is consistent with prior American multicentre studies that report that nearly half of adult CHD patients experience significant gaps in cardiology care at some point.Reference Gurvitz, Valente and Broberg 18 , Reference Wacker, Kaemmerer and Hollweck 29
Recognition of specific factors leading to loss of follow-up is essential for transition process improvement. Lack of patient awareness about the necessity for long-term follow-up has previously been described as a common reason for poor follow-up.Reference Mackie, Rempel, Rankin, Nicholas and Magill-Evans 14 In our experience, although nearly all (95%) patients surveyed reported that they believed they should continue to see a cardiac specialist past the age of 18, this was not predictive of maintenance of care. Female gender was associated with a greater likelihood of maintenance of care, a pattern that has previously been demonstrated.Reference Goossens, Stephani and Hilderson 1 , Reference Mackie, Ionescu-Ittu, Therrien, Pilote, Abrahamowicz and Marelli 11 Also consistent with previous studies, those with moderate- and severe-complexity lesions were more likely than those with simple lesions to maintain continuity of care.Reference Mackie, Ionescu-Ittu, Therrien, Pilote, Abrahamowicz and Marelli 11 , Reference Yeung, Kay, Roosevelt, Brandon and Yetman 12 , Reference Gurvitz, Valente and Broberg 18 , Reference Reid, Irvine and McCrindle 20 , Reference Mackie, Pilote, Ionescu-Ittu, Rahme and Marelli 30 , Reference Norris, Webb and Drotar 31 Although previous studies have described good continuity in patients followed by their paediatric cardiologist, patients within our population last seen by an adult CHD provider had less lapses in care when compared with those last seen by a paediatric or adult cardiologist.Reference Norris, Webb and Drotar 31 This highlights an important concept that although the transfer of care itself from paediatric to adult care is of paramount importance, the transition process continues afterwards, and successfully transferred patients may still experience lapses in care.Reference Saidi and Kovacs 26 Despite speculation that the development of cardiac symptoms may prompt seeking care, the presence of cardiac symptoms, perceived occupational limitations secondary to cardiac causes, or a need to visit an urgent care or emergency department within the last year were not predictive of improved continuity or maintenance of care. Interestingly, although the presence of cardiovascular symptoms was not predictive of continuity, those patients taking prescription cardiac medications had improved long-term continuity of care. Similarly, it has been reported that young adults who had undergone more paediatric surgeries or recent cardiac catheterisation had improved continuity.Reference Mackie, Rempel, Rankin, Nicholas and Magill-Evans 14 These findings are suggestive of a positive impact of contact with healthcare providers around the time of invasive procedures on continuity.
Complicated healthcare systems may present a barrier to successful transition. The non-universal American healthcare paradigm presents a challenge with regard to continuity of care; a change or loss of insurance coverage has previously been reported as a contributor to gaps in care.Reference Gurvitz, Valente and Broberg 18 Difficulties accessing health insurance benefits were reported by 15 patients, half of whom were denied owing to pre-existing conditions. The majority (10) had moderate-complexity CHD. Although there was a trend towards significance, lapses in insurance coverage were not a statistically significant predisposing factor to loss of follow-up in our population.
An understanding of the nature of one’s own condition plays a role in poor transition. It has been postulated that, especially in those with less severe CHD, the importance of long-term follow-up may not be emphasised, leading to a poor understanding of conditions and expected sequelae. In a Dutch cohort of 91 adolescents with simple- to moderate-complexity CHD, less than half were able to describe their own heart defect.Reference Van Deyk, Pelgrims and Troost 32 In our group, 46.6% of surveyed patients were unable to name their CHD lesion. A quarter of surveyed patients, regardless of whether or not they had loss of follow-up, believed that they were “cured” of their CHD (Table 3). Structured patient education in patients with CHD increases knowledge of their heart defect, medication side effects, signs of deterioration, appropriate contraceptive methods, and risk factors for endocarditis.Reference Van Deyk, Pelgrims and Troost 32 Our results suggest that focused education regarding both the need for specialised long-term adult CHD care and future employment plans are predictive of improved continuity, although patients’ self-reported perception of the need for ongoing cardiac visits was not a contributing factor to continuity. Although discussions regarding the possibility of future cardiac interventions or surgery are an important part of adult CHD education, they do not influence loss of follow-up. These findings allude to a link between increased knowledge of one’s own heart condition and improved long-term continuity, and highlight starting points for the further development of educational tools and safeguards to improve the efficacy of the transition process.
Limitations
Limitations of this study include the retrospective analysis of data, limited enrolment, and inability to assess continuity of care outside our healthcare system in those who could not be contacted. Response rates were limited by the inability to contact many of the eligible patients, as well as hesitancy to participate in a survey once successfully contacted. Limited enrolment remains a significant hurdle in the assessment of continuity in this population. Most other authors’ attempts to contact patients lost to follow-up have had similarly poor success despite using a variety of methods such as mailed surveys, telephonic questionnaires, and social networking sites.Reference Wacker, Kaemmerer and Hollweck 29 , Reference Valente, Lewis and Vaziri 33 Even within the universal healthcare system in Germany, which allowed tracking of over 10,500 patients with CHD, there was a response rate of only 24%.Reference Wacker, Kaemmerer and Hollweck 29 The wide spectrum of CHD complexity we enrolled probably also contributed to greater rates of attrition and limited survey enrolment. Similar efforts within America have been limited to a population of patients with greater overall complexity of CHD, a subgroup that has consistently shown the lowest rates of attrition from care.Reference Norris, Webb and Drotar 31 , Reference Valente, Lewis and Vaziri 33 The proportion of patients with true interruption in cardiac care within the loss of follow-up subset may be overestimated. We were unable to assess whether patients had transitioned their cardiac care to another provider outside of our healthcare system unless they were successfully contacted and answered the questionnaire. In the group of patients with loss of follow-up who were successfully contacted, about half (7 of 16, 44%) reported not seeing a cardiac provider for ⩾3 years. However, in those with documented visits in that time span, 5 (12%) also reported not having seen a cardiac provider for ⩾3 years, calling into question the accuracy of patient recall of the timing of last cardiac visit. As another consequence of limited enrolment, the importance of factors such as presence of cardiovascular symptoms and loss of insurance coverage that did not reach statistical significance are likely underestimated owing to inadequate power. Indeed, surveyed patients with lapses in care frequently cited cardiac symptoms or pregnancy as the primary reason for re-establishing care. The association between simple CHD and increased likelihood of loss of follow-up may be partly owing to some patients being told they did not require ongoing surveillance. Last, although the questionnaire was specifically developed to gather qualitative data pertinent to the study drawing on relevant published literature, it was not psychometrically validated as a scale.
Conclusion
Preventing attrition of patients with CHD during transition of care between paediatric and adult providers is a major challenge. Despite the increasing prominence of specialised care for adult CHD, emphasis on successful transition and long-term adult CHD follow-up continues to be poor. Formal transition programmes incorporating focused education for this at-risk population are a vital component of adult CHD care. In our single- centre experience, patients with greater complexity of CHD, those using prescription medications, those who received dedicated transition education, and those who established care with adult CHD providers had superior follow-up. Patients with simple and moderate complexity CHD represent a subgroup with worse long-term follow-up that may benefit from increased scrutiny and focused transition education. In view of the increasing numbers of survivors of childhood chronic illness such as CHD, there is an urgent need for further developments in all aspects of transitional care to improve the long-term outcomes for this growing population and allow these young people to meet their full adult potential in the years to come.
Acknowledgements
The authors thank Amber Khanna, MD, for her editing assistance and feedback during the preparation of this manuscript.
Authors’ Contribution
All authors take responsibility for the data presented and their discussed interpretation.
Financial Support
This research received no specific grant from any funding agency or from commercial or not-for-profit sectors.
Conflicts of Interest
None.
Ethical Standards
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national guidelines on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008, and has been approved by the institutional review board of The Ohio State University.










