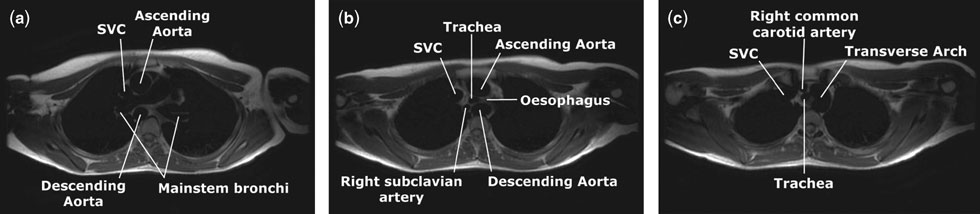
A16-year-old otherwise healthy girl was referred with dysphagia. She had no history of stridor. Physical examination was normal. Echocardiography revealed a left aortic arch with otherwise normal intracardiac anatomy. The transverse aortic arch appeared atypical, with poorly visualized branches, prompting cardiac magnetic resonance imaging (video link – steady state free precession cine images [FIESTA™] in coronal view – see www…). On black blood double inversion axial views (Fig. 1a–c), a left aortic arch, and right-sided descending thoracic aorta were seen. At the level of the carina (b), the trachea and oesophagus were compressed by the course of the aorta. The right subclavian artery arose anomalously as the final branch of the arch (b), while the right common carotid artery arose as the first vessel (c). Also shown are the superior caval vein (SVC) and the main stems of the bronchi. Presence of a right-sided arterial ligament was confirmed in the operating room, and the ligament was divided.
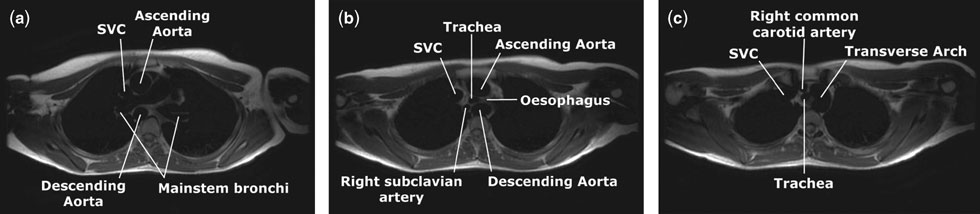
Figure 1
When a left aortic arch coexists with a right-sided descending aorta, the right subclavian artery is the terminal branch of the aortic arch. In this setting, a persistent arterial duct or ligament almost always connects the right pulmonary artery to the descending aorta, or the base of the subclavian artery (Fig. 2). This forms a complete vascular ring that may produce respiratory compromise in infancy or dysphagia during childhood. Because it is one of the few vascular anomalies approached through a right thoracotomy, careful preoperative evaluation of the sidedness of the descending thoracic aorta is essential. This may now be achieved with computed tomography or magnetic resonance imaging.
Figure 2