Pulmonary atresia with intact ventricular septum is a rare lesion, comprising <1% of all CHDReference Ashburn, Blackstone and Wells1 with 1-year survival ranging from 68% to 88%.Reference Ashburn, Blackstone and Wells1,Reference Schneider, Blom and Bruggemans2 Established risk factors for increased mortality include tricuspid valve annulus z score less than −2 and low birth weight.Reference Ashburn, Blackstone and Wells1,Reference Liava’a, Brooks and Konstantinov3–Reference Awori, Mehta and Mitema5 Literature has suggested the strongest mortality predictor is presence of right ventricular-dependent coronary circulationReference Grant, Faraoni and DiNardo6 (defined as presence of coronary sinusoids with proximal stenosis resulting in RV preload-dependent myocardial perfusion).
For many patients with pulmonary atresia/intact ventricular septum, survival in the neonatal period is dependent on alternative sources of pulmonary blood flow.Reference Mallula, Vaughn and El-Said7 The anatomic pathophysiology necessitates unrestrictive atrial level right-to-left shunting to offload venous return and augment the left ventricular cardiac output that supplies both the systemic and pulmonary circulation via patent ductus arteriosus.Reference Chikkabyrappa, Loomba and Tretter8 Neonates born with restrictive atrial level communication may require urgent balloon atrial septostomy to create this unrestrictive flow. After establishing adequate pulmonary circulation, infants can be managed via single-ventricle palliation, one-and-a-half ventricle, or as a bi-ventricular repair. The management strategies for pulmonary atresia/intact ventricular septum are evolving as the role of catheter-based intervention is expanding.
The selection of a primary repair strategy is complex and individualised. Important factors include the presence of coronary sinusoids and the size of the tricuspid valve annulus. In patients without sinusoids and an adequate tricuspid valve annulus, establishing prograde pulmonary flow (either by surgical transannular patch or more recently by radiofrequency perforation of the pulmonary valve) promotes growth of the hypoplastic right ventricle.Reference Chikkabyrappa, Loomba and Tretter8 Patients who achieve adequate right ventricular growth with preserved function may be managed as a bi-ventricular repair and may not require additional intervention until much later in life. On the other end of the spectrum, patients with coronary sinusoids or a small tricuspid valve annulus are often managed with single-ventricle palliation. Those in the middle may be managed with a bidirectional Glenn via the so-called one-and-a-half ventricle repair. The decision about which management strategy to pursue is complex. We report outcomes and destination circulation after newborn intervention for pulmonary atresia/intact ventricular septum patients.
Methods
This is a 30-year (1988–2018) retrospective study of patients with pulmonary atresia/intact ventricular septum conducted at a single paediatric cardiac centre. Patients who did not follow-up at the index institution (≤1 follow-up visit) and patients with concomitant Ebstein anomaly were excluded. Patients were grouped based on the type of newborn intervention (within the first month of life), presence of coronary sinusoids, and destination circulation (single ventricle, one-and-a-half ventricle, and bi-ventricular). Median follow-up duration was calculated based on the date of birth (or date of presentation/transfer to index institution) and the date of most recent follow-up visit.
Discrete variables were summarised as percentages and continuous variables with median and interquartile range. Statistical analysis was completed using Fischer’s exact test, t-tests, multivariate linear regression modelling, and Kaplan–Meier for survival. Statistical analyses were computed using Excel and SPSS (version 26), with a p-value <0.05 considered statistically significant (all reported p-values are two-sided). This study was approved by the Institutional Review Board of the University of California San Diego.
Results
Ninety patients met inclusion criteria, as shown in Fig 1. One patient received a neonatal transplant and was excluded from the analysis. Fifty-six per cent of patients were male and the median gestational age was 39 weeks (interquartile range 37–39). Demographics are reported in Table 1. Coronary sinusoids noted at catheterisation or by echo were present in 55%, of those approximately half had angiographic confirmation of right ventricular dependence. The median year of birth was 2007 (interquartile range 1999–2013) and the median follow-up was 8 years (interquartile range 2.3–17.8). All-cause mortality was 10%, and early mortality under 18 months of age was 8.8%.
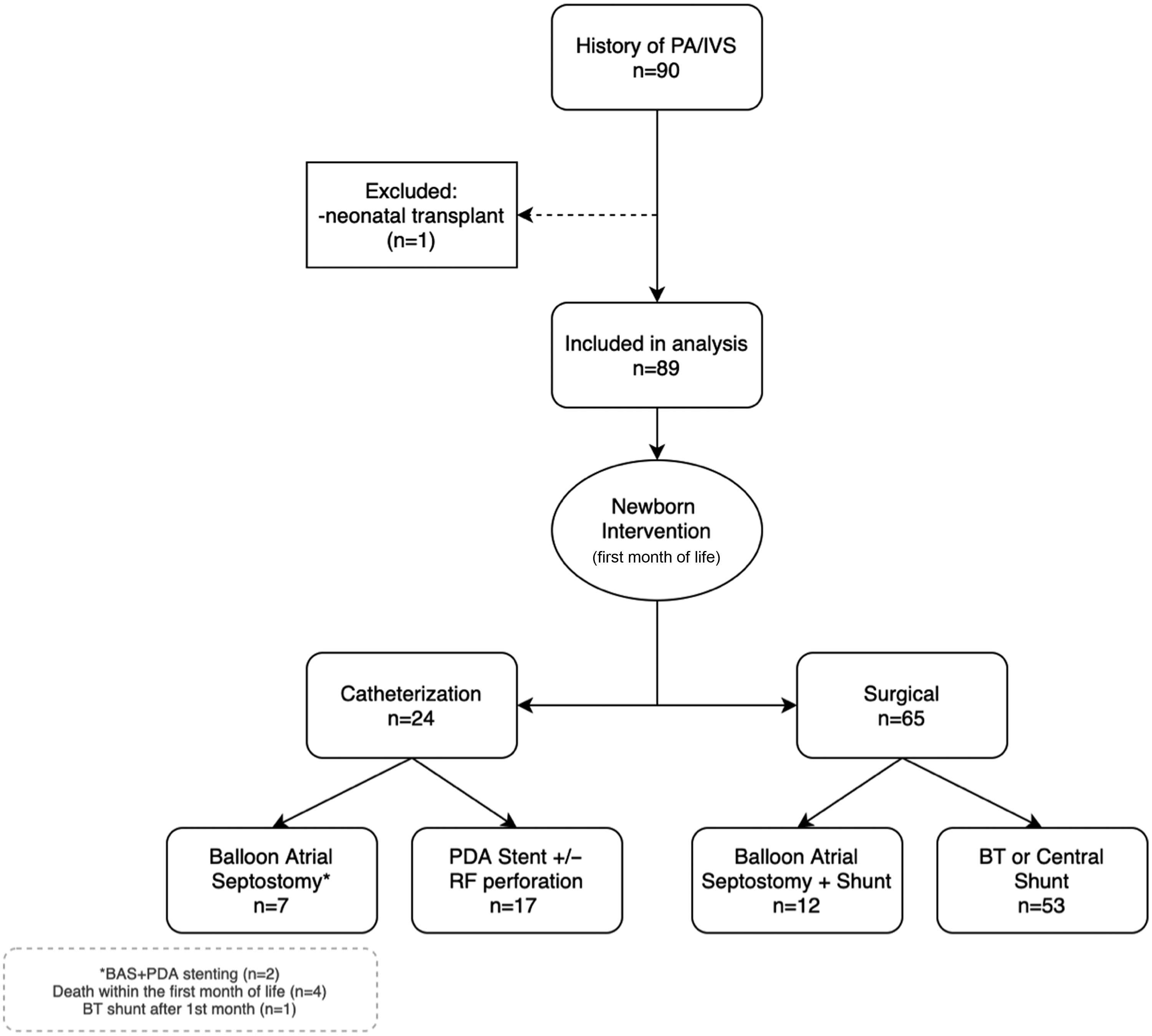
Figure 1. Inclusion/exclusion criteria.

Figure 2. Survival curve, infants with PA/IVS who require BAS compared to those who do not require BAS in the newborn period.
Table 1. Demographic data

* Accompanied by PDA stenting in two patients.
+ Died at <30 days of life, no definitive surgical plan/palliation pursued.
RVDCC=Right ventricular-dependent coronary circulation.
Seventy-two per cent of patients were managed surgically in the newborn period, 70% via modified Blalock–Taussig shunt, and 30% via central aortopulmonary shunt. Twelve patients had a balloon atrial septostomy before surgical intervention. The majority of infants managed surgically had evidence of coronary sinusoids, though only 30% had right ventricular dependence. Not surprisingly, most who underwent surgical intervention ultimately ended up with single-ventricle palliation. The median year of birth was 2001 (interquartile range 1994–2007) for patients who underwent surgical shunt and 2008 (interquartile range 1994–2007) for patients who underwent balloon atrial septostomy as well as surgical shunt.
Twenty-four patients were managed exclusively via transcatheter intervention in the newborn period, patients were grouped based on if they required an atrial septostomy or not. Twenty-four patients who were managed via transcatheter intervention were born more recently than those who underwent primary surgical repair (p < 0.0001). Most did not require an atrial septostomy, 70% underwent ductal stenting accompanied by radiofrequency perforation and/or pulmonary valvuloplasty. A minority of these patients had coronary sinusoids (11.8%) and none had evidence of right ventricular-dependent circulation. Notably, 82% of this group was able to achieve the bi-ventricular repair. There were seven patients who required atrial septostomy (without additional surgical intervention) in the newborn period. Within this group, four died in the newborn period, one underwent septostomy and ductal stenting and died at 7 months, one patient ultimately required surgical shunt placement at the age of 1 (now managed as one-and-a-half ventricle repair), and one underwent a bidirectional Glenn and is awaiting Fontan.
Of the total 89 patients, 21% required balloon atrial septostomy, as shown in Table 2. Most of these patients (63%) also required a shunt within the first month of life and are included in the surgical cohort. Of those who required a septostomy, most ended up with single-ventricle palliation (n = 13, 68%). Two patients were palliated to one-and-a-half ventricle circulation and four died in the newborn period. None of the patients who required an atrial septostomy were able to achieve a bi-ventricular circulation.
Table 2. Subgroup analysis of infants who required balloon atrial septostomy

+ Early death in the newborn period (<30 days) prior to the decision on destination anatomy.
Overall mortality at median 8 years follow-up was 10%. Eight of the nine deaths occurred in the first 18 months of life (median age at death: 2.7 months, interquartile range: 0.7–6.1 months), as shown in Table 3. Patients who required balloon atrial septostomy in the newborn period had significantly higher mortality than those who did not (36% versus 1.4%, p < 0.001; Fig 2). Of those who died before 18 months, 87% required atrial septostomy in the newborn period, of which 85% had documented evidence of right ventricular-dependent coronary circulation. Five patients had evidence of myocardial ischaemia at the time of death (elevated troponin, EKG changes) and one patient had an out-of-hospital arrest, as shown in Table 4. The presence of coronary sinusoids was not identified as an independent risk factor for 18-month mortality (HR: 0.61; 95% CI: 0.21–16.5). However, undergoing balloon atrial septostomy was found to be a significant predictor of early mortality (HR: 3.18; 95% CI: 2.7–215.6).
Table 3. All-cause mortality

Table 4. Details surrounding early deaths (prior to 18 months)

RVD = Right ventricular dependent
Discussion
Overall mortality for patients with pulmonary atresia/intact ventricular septum at median 8-year follow-up was 10%, consistent with previously published literature.Reference Schneider, Blom and Bruggemans2 We found that early mortality was significantly higher in patients requiring balloon atrial septostomy, the mechanism for this finding is likely multifactorial. Patients with a restrictive atrial communication requiring septostomy at birth often present with haemodynamic collapse and more severe disease. Our report is the first to quantitatively delineate this mortality difference. Interestingly, two of the eight early deaths (Table 4) were due to complications from sepsis, both underwent BAS and surgical shunt in the newborn period. There may be a peri-procedural elevated infectious risk, though more research is needed before definitive conclusions can be drawn given the limited number of affected patients. The higher mortality (36% versus 3.4%) for patients requiring septostomy may have implications on clinical management (including the timing of surgical/transplant referral), appropriate counselling, and expectation setting for families and providers.
Balloon atrial septostomy is a necessary procedure for infants with the restrictive atrial flow and haemodynamic instability, but may have unintended consequences. Patients with coronary sinusoids and proximal coronary artery stenosis are dependent on right ventricular pressure for coronary perfusion. It has been hypothesised that offloading the right ventricle may result in a coronary steal phenomenon and myocardial ischaemia. Looking closer at the eight early deaths, five had documented myocardial ischaemia and ischaemic EKG changes after the septostomy, suggesting that coronary flow may have been compromised. However, without post-septostomy angiography at the time of decompensation, it is impossible to comment definitively on if these clinical findings were due to a coronary steal phenomenon or acute heart failure/haemodynamic collapse in the setting of critical illness.
In the current era at our institution, all infants with pulmonary atresia/intact ventricular septum undergo an echocardiogram at birth with careful examination of the coronary anatomy, the tricuspid valve, the right ventricle, and the atrial communication, as shown in Fig 3. All newborns are treated with prostaglandin. Infants with highly restrictive atrial septum and evidence of haemodynamic instability (low cardiac output requiring vasopressors or inotropes, echocardiograph evidence of right heart failure, or prenatal hydrops fetalis) are evaluated for urgent balloon atrial septostomy. After haemodynamic stability is achieved, typically several days after birth, all infants under angiographic evaluation of the coronary arteries. If right ventricular coronary dependence is identified, the patient is evaluated for urgent surgical intervention, including consideration for neonatal transplant. Current indications for initiation of transplant workup include left ventricular dysfunction, ischaemic EKG changes, and cardiac biomarker elevation. Infants without right ventricular dependence may be managed as a single ventricle, one-and-a-half ventricle, or bi-ventricular repair depending on the tricuspid valve annulus and clinical response to right ventricular decompression. As the applications of transcatheter intervention expand, over the last decade, our institution has trended away from surgical intervention and towards exclusive transcatheter management in the newborn period, as evidenced by the trends in birth year (Table 1).

Figure 3. Institutional management pathway for neonates with PA/IVS.
Of the 19 patients who required septostomy, the presence of sinusoids and right ventricular dependence was over-represented compared to those who did not require septostomy (Table 2), consistent with the notion that patients who require septostomy at birth often have more severe disease. Interestingly, the patients who underwent both a septostomy and surgical shunt in the newborn period fared better than those who only had a septostomy (18-month mortality 16.7% versus 71.4%, respectively, p = 0.017). Despite the expanding applications of transcatheter interventions in this population, patients presenting with severe disease requiring an atrial septostomy at birth may benefit from surgical intervention and transplant evaluation in the newborn period.
The significantly elevated mortality for patients with pulmonary atresia/intact ventricular septum who require an atrial septostomy is likely multifactorial in the setting of more severe underlying anatomy and post-septostomy haemodynamic changes. For infants with coronary sinusoids and evidence of RV-dependent circulation on angiography, atrial septostomy should only be performed on an urgent or emergent basis and these patients should be considered for early surgical intervention (including consideration for neonatal transplant).
Conclusions
Patients with pulmonary atresia/intact ventricular septum who require balloon atrial septostomy in the newborn period have significantly higher 18-month mortality (36% versus 1.4%) than patients with unrestrictive atrial flow. Quantifying the mortality difference may help guide prognostication and expectation setting for families. Infants who required septostomy and a surgical shunt in the newborn period fared better than those who only underwent septostomy (even when the septostomy was accompanied by ductal stenting and pulmonary valve intervention). For infants with coronary sinusoids and evidence of RV-dependent circulation on angiography, atrial septostomy should only be performed on an urgent or emergent basis and these patients should be considered for early surgical intervention, including consideration for neonatal transplant.
Limitations
This is a single-centre retrospective study spanning a relatively large time frame and multiple management eras. Some clinical data was not available due to changes in electronic medical record systems, for patients with coronary sinusoids, a portion of patients were classified as having RV dependence based on clinical documentation (compared to actual angiographic evidence (Supplementary Table 1). In addition, this is a relatively small series, largely because pulmonary atresia/intact ventricular septum comprises only 1% of CHD.
Acknowledgements
None.
Financial support
There was no financial support for this manuscript.
Conflicts of interest
The authors have no conflicts of interest.
Disclosures
None.
All authors take responsibility for all aspects of the reliability and freedom from bias of the data presented and their discussed interpretation.
Ethical standards
This study was approved by the Institutional Review Board at University of California San Diego.
Supplementary material
To view supplementary material for this article, please visit https://doi.org/10.1017/S1047951121000640.










