Case report
A 10-year-old boy presented with high-grade fever for 12 days, along with left-sided cervical lymphadenopathy, macular rash over the trunk, bilateral non-suppurative conjunctivitis, fissuring of the lips, and desquamation over the back of the trunk, satisfying the clinical criteria for diagnosis of Kawasaki disease. Routine investigations revealed leucocytosis, sterile pyuria, as well as elevated C-reactive protein (24 mg/L) and erythrocyte sedimentation rate (56 mm per 1st hour). His chest X-ray and the 12-lead electrocardiogram were normal. Two-dimensional echocardiography revealed giant coronary aneurysms (Fig 1a–d) involving the left main artery, left anterior descending artery, and the right coronary artery (Supplementary video 1). Mild pericardial effusion was noted. Intravenous immunoglobulin was given on the 12th day of illness as per the standard recommended dose. The patient was submitted to anticoagulation treatment with warfarin, followed by an adequate dose to maintain international normalised ratio values from 2.0 to 3.0. Baseline international normalised ratio before the detection of thrombus was 1.2; aspirin was added to the treatment protocol. The patient was followed up with serial echocardiographies. Follow-up two-dimensional echocardiography at 6 months (Fig 1e and f) revealed giant coronary aneurysms involving the left and right coronary arteries, with thrombus visualised in the left anterior descending artery (Supplementary video 2). There were no associated regional wall motion abnormalities. Left ventricular systolic function was normal (Supplementary video 3). As the patient was asymptomatic, with a normal electrocardiogram, he was managed conservatively and was under regular follow-up. The warfarin dosage for the patient was adjusted to attain a therapeutic international normalised ratio of 2–3, along with daily administration of 75 mg of aspirin.
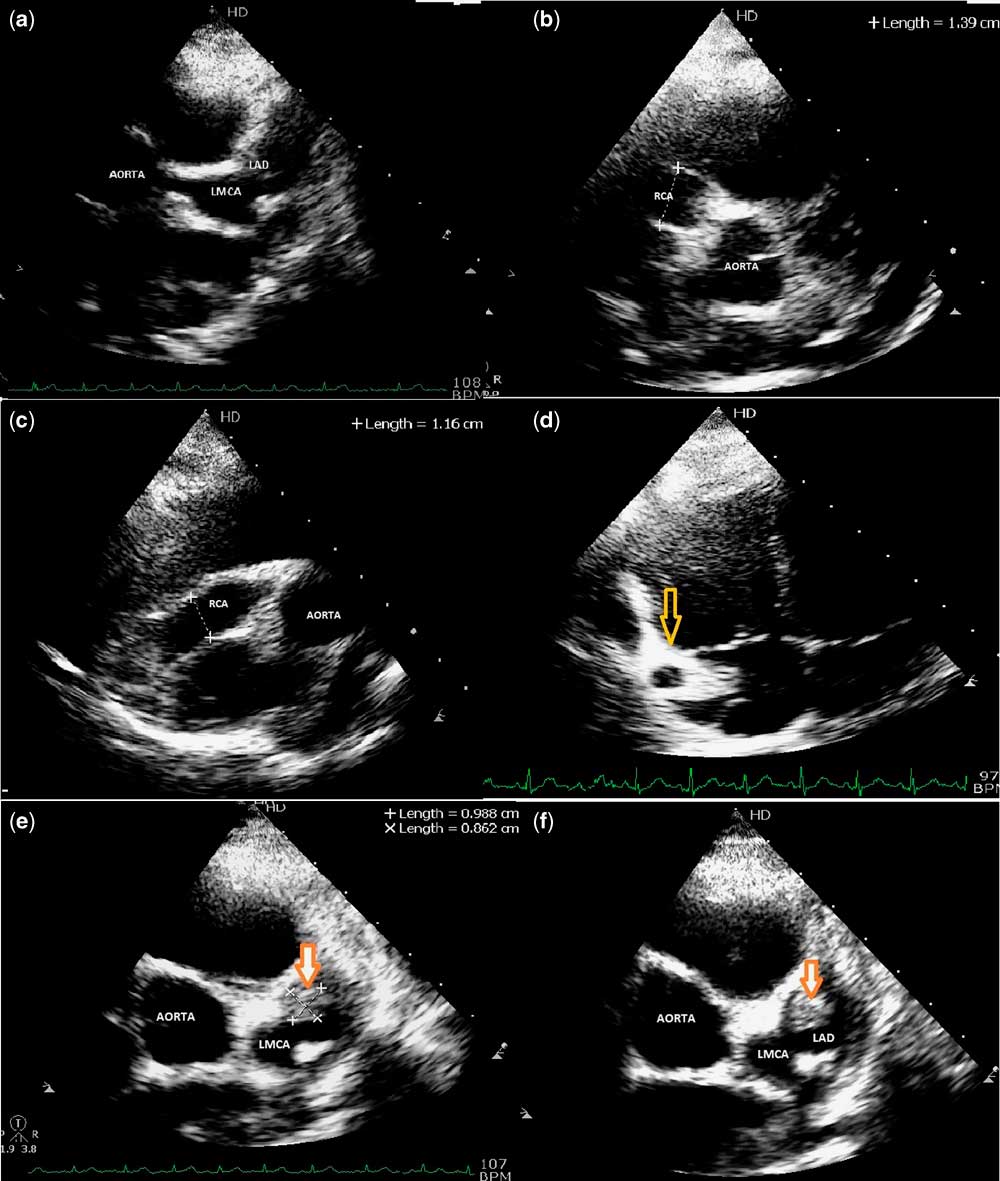
Figure 1 ( a ) Parasternal short-axis view showing giant coronary aneurysms involving the left main coronary artery and left anterior descending artery. ( b and c ) Modified parasternal short-axis view showing a giant coronary aneurysm measuring 13 mm involving the proximal and mid-right coronary artery. ( d ) Modified subcostal four-chamber view that shows (yellow arrow) the distal right coronary artery. ( e and f ) Modified short-axis view revealing a 9×8 mm thrombus in the left anterior descending artery.
Kawasaki disease was initially described by Tomisaku Kawasaki, a Japanese paediatrician, in 1967. It is a febrile vasculitis affecting medium-sized arteries, with a predilection for the coronary arteries. It predominantly affects children between 6 months and 5 years of age. Aneurysms usually appear between 1 and 4 weeks after the onset of fever. An aneurysm developing after 6 weeks of fever is rare. Coronary arterial abnormalities develop in 15–25% of children with untreated Kawasaki disease. It has been seen that therapy with parenteral immunoglobulin and aspirin within the first 10 days of onset of fever reduces the prevalence of coronary arterial abnormalities to ~5%.Reference Singh and Kawasaki 1
A coronary aneurysm is diagnosed when the internal lumen diameter of the coronary arteries is found to be >3 mm in children younger than 5 years or >4 mm in children older than 5 years on two-dimensional echocardiography. The American Heart Association has classified coronary aneurysms on the basis of their sizes as small (<5 mm), large (5–8 mm), and giant coronary aneurysms (>8 mm).Reference Newburger, Takahashi and Gerber 2 Giant coronary aneurysms are less likely to regress, and they have the highest association with progression to stenosis and myocardial infarction.Reference Gerding 3 Factors favouring aneurysm regression include an age of onset >1 year, aneurysm diameter <8 mm, fusiform morphology, and being of female sex. Overall, 50–67% of vessels with Kawasaki disease showed regression 1–2 years after onset, when reviewed using angiography. Coronary aneurysms are most commonly seen in proximal segments of the left anterior descending artery and right coronary artery. An echocardiogram may also reveal decreased left ventricular contractility, mild valvular regurgitation (most commonly mitral regurgitation), and pericardial effusion.Reference De Ferranti 4 Intravenous immunoglobulin was given on the 12th day of illness. There are few data on the efficacy of intravenous immunoglobulin therapy administered after more than 10 days of onset of illness. American Heart Association and American Academy of Pediatrics guidelines, however, recommend that intravenous immunoglobulin should still be administered to children with Kawasaki disease who present symptoms after the 10th day of illness, such as persistent fever, coronary aneurysms, or evidence of ongoing systemic inflammation.Reference Newburger, Takahashi and Gerber 2 , Reference Marasini, Pongiglione and Gazzolo 5
The present report illustrates a rare case of Kawasaki disease with a delayed presentation at 10 years of age, giant coronary aneurysms, and an accompanying coronary arterial thrombus that was detected by two-dimensional echocardiography.
Acknowledgements
None.
Financial Support
This research received no specific grant from any funding agency, commercial or not-for-profit sectors.`
Conflicts of Interest
None.
Supplementary Material
To view supplementary material for this article, please visit https://doi.org/10.1017/S1047951117001329




