Neurodevelopmental disability is the most common complication for survivors of surgery for congenital heart disease (CHD). Reference Gaynor, Stopp and Wypij1 A systematic review of motor and cognitive outcomes after surgery for CHD consistently revealed cognitive and motor delays in children after cardiac surgery in early infancy. Reference Snookes, Gunn and Eldridge2 Survivors are at risk for neurodevelopmental morbidity caused by both biological and environmental risk factors. Reference Marino, Lipkin and Newburger3 As a result, an important shift has occurred toward mitigating morbidity associated with surgical and supportive care and greater integration of developmental care practices in inpatient and outpatient care. We previously found motor impairments in infants hospitalised for cardiac surgery are common and associated with longer intubation and prolonged exposure to the intensive care (ICU) environment. Reference Uzark, Smith, Donohue, Yu and Romano4 It seems likely that prolonged periods of immobility, supine positioning and confinement after the operation impede motor development and may contribute to loss of motor strength. A developmental theory termed “developmental cascades” refers to the cumulative consequences for the development of the many interactions and transactions occurring in developing systems that result in spreading effects across levels, among domains at the same level and across different systems. Reference Masten and Cicchetti5 Acquisition of motor skills can facilitate greater exploration and learning and may promote a more positive developmental cascade. Libertus and colleagues found that motor training, manipulations of emerging reaching skills, in 3-month-old infants facilitated object exploration and attention skills at 15 months of age. Reference Libertus, Joh and Needham6
Awake prone positioning or “tummy time”, a crucial component of the development of head control and upper body strength which are the building blocks for later developmental skills, is recommended to facilitate motor milestone development in infants. The primary aim of this study was to evaluate the feasibility and efficacy of a tummy time intervention to improve motor skill development in young infants after cardiac surgery.
Patients and methods
The study was approved by the University of Michigan Institutional Review Board and registered at clinicaltrials.gov (NCT02700646). Parental consent was obtained. Infants less than 4 months of age were randomly assigned to tummy time with or without outpatient reinforcement or standard of care.
Patient population
A convenience sample of 64 infants less than 4 months of age who were intubated for at least 24 hours following cardiac surgery was included in the study. The study excluded infants with pre-operative clinical evidence of a central nervous system anomaly or history of central nervous system insult and infants with a history of prematurity born at less than 36 weeks gestation.
Procedure and measures
Infants were randomly assigned to one of three groups:
Group 1 – Inpatient Intervention: During hospitalisation after cardiac surgery, recommendations for tummy time were made to bedside staff and parents by a study nurse and physical therapist. Instructions and placement of the infant in the prone position or tummy time were demonstrated to reassure parents regarding the safety of this positioning. Parents received mirrors and small blankets with tags to motivate the infant to tolerate the prone position, and an infant support pillow for tummy time. Prior to discharge, the infant’s parent was given tailored instructions regarding daily, at-home tummy time with directions to advance the daily duration of tummy time, starting with a goal of 5 minutes three times daily.
Group 2 – Inpatient + Outpatient Intervention: This intervention included the inpatient intervention described above plus outpatient telephone follow-up provided by a psychologist weekly for 4 weeks and then biweekly to help families overcome barriers to achieving the tummy time intervention (e.g., child distress, scheduling).
Group 3 – Control/Standard of Care: Participants received an American Academy of Pediatrics brochure (Back to Sleep, Tummy to Play) describing the importance of tummy time during play. There was no additional instruction above the standard of care. Parents were given a board book and a small blanket for the infant. There was not clinical equipoise to recommend no tummy time.
Neuromotor skills were assessed using the Alberta Infant Motor Scale (AIMS) administered to each infant prior to hospital discharge and at 3 months after discharge by physical therapists. The AIMS is a standardised scale used to assess and monitor the gross motor development of infants, by passive observation of spontaneous motor activity of the infant in prone, supine, sitting and standing positions. Reference Piper and Darrah7 Each item is scored as “observed” or “not observed” with items ordered by increasing difficulty. The assessment is used to evaluate or monitor motor development, maturation or change over time as the result of ageing or intervention, incorporating components of motor development deemed essential to the treatment of at-risk infants. The AIMS has established reliability and validity to measure motor development in infants aged 0–18 months. Reference Piper and Darrah7 In addition, parents were contacted by telephone at 1, 4, and 8 weeks after discharge from the hospital to assess the infant’s developmental progress and approximate daily time spent in various activities/positions, including tummy time, in the prior 24-hour period. Parents of Group 1 and Group 3 patients were contacted by a research nurse. Parents of Group 2 patients were contacted by the paediatric psychologist as described above. Parents of all infants who returned for follow-up were given a gift card to cover transportation and other expenses.
Patient demographics/clinical data
Demographic, pre-operative, intra-operative and post-operative clinical data for all infants was obtained from the medical record. Patient-related variables included sex, race, age at surgery, gestational age, diagnosis, significant non-cardiac anomalies, operative procedure performed, cardiopulmonary bypass time, neurologic complications, ventilator days and ICU and hospital length of stay.
Statistical Analyses
Descriptive statistics are reported as frequency and percentage (%) for categorical variables and median with interquartile range (IQR) or a full range for continuous variables. Demographic and clinical characteristics at initial assessment were compared between infants who completed the 3-month assessment and those without follow-up using Chi-square test or Fisher’s exact test for categorical variables and Wilcoxon rank sum test for continuous variables. Similar comparisons in demographic and clinical characteristics at initial assessment as well as at 3-month assessment were made between groups using Chi-square test or Fisher’s exact test for categorical variables and Wilcoxon rank sum test or Kruskal–Wallis test for continuous variables, as appropriate. Duration of daily tummy time as reported by parents was also dichotomised as less than 15 minutes or 15 minutes or more tummy time as previously dichotomised by Salls et al. Reference Salls, Silverman and Gatty8 The overall change in Alberta Infant Moror Scale score from initial assessment to 3-month follow-up was examined using one-sample t-test. To examine the impact of the tummy time intervention on motor skills, change in AIMS score was compared between tummy time intervention groups and the standard of care group, using two-sample t-test. Demographic and clinical characteristics at initial assessment by tummy time duration (<15 minutes versus >15 minutes) were also compared using Chi-square test, Fisher’s exact test or Wilcoxon rank sum test, as appropriate. Linear regression without and with adjustment for age at initial assessment was used to evaluate the association between tummy time duration and change in AIMS score. All analyses were performed using SAS Version 9.4 (SAS Institute Inc., Cary, NC). A p-value <0.05 was considered statistically significant.
Results
Patient characteristics
Parents of infants (n = 64) who had cardiac surgery at a median age of 5 days (range 2 days −3.4 months) were randomly assigned to inpatient tummy time instruction (n = 20), inpatient + outpatient tummy time instruction (n = 21) or standard of care (n = 23). Forty-nine (77%) returned for 3 months follow-up after discharge at a median age of 3.9 months (IQR 3.6–4.4). Infants who were ill by parent report and/or hospitalised at the time of follow-up were excluded. There were no significant differences in demographic/clinical characteristics or initial AIMS scores between infants who completed the 3-month follow-up assessment and those without follow-up. Parents were more likely to be present during the initial AIMS assessment in patients who returned for follow-up (94% versus 73%, p = .047). Patient characteristics by groups are summarised in Table 1. Overall, 11 (22%) infants had single ventricle lesions. Four infants had post-operative seizures, two infants with clinically apparent strokes. Total ICU length of stay ranged from 2 to 40 days (median 8 days) with a total hospital length of stay ranging from 5 to 72 days (median 16.5 days). Overall there were no significant differences in patient characteristics between the study groups except shorter total ICU length of stay in the inpatient tummy time instruction group compared to other groups.
Table 1. Patient and clinical characteristics at initial assessment by study group in infants who completed 3-month assessment (N = 49)
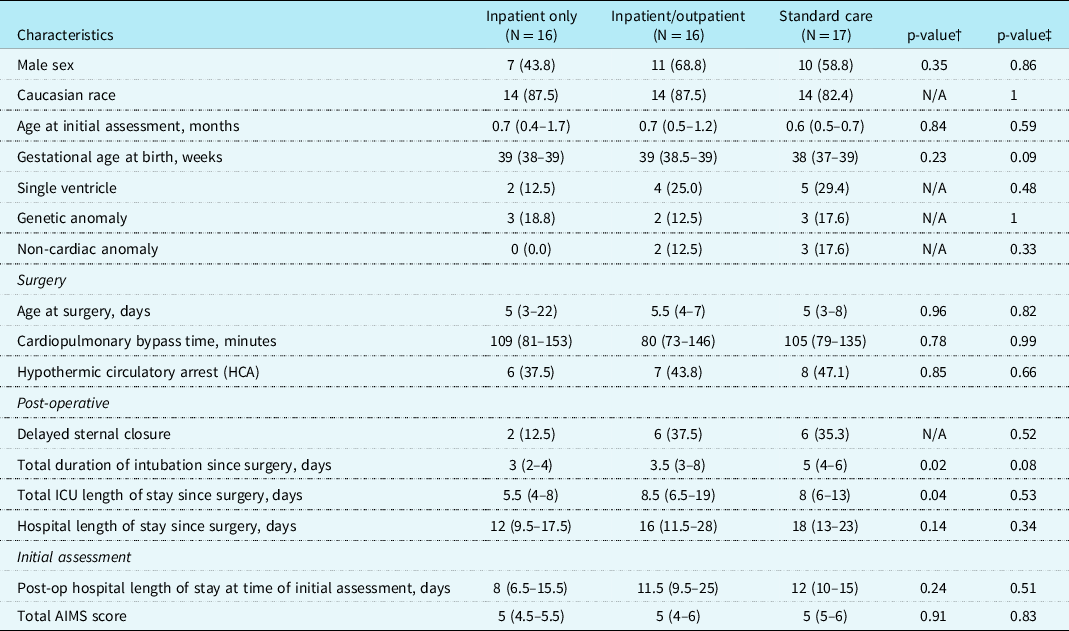
Data are presented as N (%) for categorical variables and median (interquartile range) for continuous variables
†Three-group comparison was made as inpatient only versus inpatient/outpatient versus standard care and p-value from Chi-square test for categorical variables and Kruskal-Wallis test for continuous variables
‡Two-group comparisons were made as inpatient only or inpatient/outpatient versus standard care and p-value from Chi-square test or Fisher’s exact test for categorical variables and Wilcoxon rank sum test for continuous variables
Comparison of intervention groups. At follow-up, reported daily tummy time varied within groups but was not significantly different between groups (Table 2). Nearly one-third (28%) of the parents in the intervention groups and 35% of the parents in the control group reported less than 15 minutes of tummy time daily at follow-up. Overall AIMS scores improved significantly between initial and 3-month assessment (7.6 ± 3.8, p < 0.0001) as expected with advancing age, however 30% of infants had scores below the 10th percentile for age. There was a trend toward greater change/increase in AIMS scores in infants who received either inpatient or inpatient/outpatient tummy time intervention in comparison to infants who received standard of care (mean 8.3 ± 4.0 versus 6.4 ± 2.9, p = 0.08).
Table 2. Three-month assessment by study groups in infants who completed 3-month assessment (N = 49)

Data are presented as N (%) for categorical variables and median (interquartile range) for continuous variables
† Three-group comparison was made as Inpatient only versus Inpatient/Outpatient versus standard care and p-value from Chi-square test for categorical variables and Kruskal–Wallis test for continuous variables
‡ Two-group comparisons were made as Inpatient only or inpatient/outpatient versus standard care and p-value from Chi-square test for categorical variables and Wilcoxon rank sum test for continuous variables
Relationship between tummy time duration and AIMS scores. There were no significant differences in patient and clinical characteristics at initial assessment between infants with <15 minutes versus ≥15 minutes of tummy time daily (Table 3). However, the change in AIMS score from pre-discharge to 3-month follow-up was significantly less in infants with less than 15 minutes of tummy time daily than in infants with >15 minutes of daily tummy time (p = 0.01) (Fig 1). This significance remained even with adjustment for age at initial assessment (adjusted mean 5.9 versus 8.5, p = 0.02). There were no significant differences between the groups with respect to receipt of therapies at follow-up (33% in infants with <15 minutes versus 48% in those >15 minutes, p = 0.33).

Figure 1. Comparison of change in AIMS scores from pre-discharge to 3 months post-discharge in patients with <15 minutes and ≥15 minutes of tummy time.
Table 3. Patient and clinical characteristics at initial assessment between infants who spent <15 minutes versus >15 minutes on daily tummy time (N = 48)

Data are presented as N (%) for categorical variables and median (interquartile range) for continuous variables
‡ P-value from Chi-square test or Fisher’s exact test for categorical variables and Wilcoxon rank sum test for continuous variables
Discussion
Motor impairments are common in infants hospitalised for a cardiac operation and may be mitigated by tummy time/awake prone positioning. Unfortunately, while parents of infants who were randomised to the inpatient or inpatient/outpatient tummy time intervention groups were given recommendations for daily tummy time at home following discharge, one in three parents did not follow the recommendation. In spite of randomisation, parents made the ultimate decision about prone positioning of their infant. Consistent with our findings, in a sample of infants from a general paediatric medical practice, Salls and colleagues Reference Salls, Silverman and Gatty8 found that overall infants are spending very little awake time in prone position, a change in practice since the American Academy of Pediatrics (AAP) “Back to Sleep” campaign, with concern that some caregivers may not be allowing infants to lie prone even while awake. 9 The AAP revised the original recommendation to “Back to Sleep, Tummy to Play” to provide opportunities to facilitate motor milestone development and prevent positional plagiocephaly 10 and suggests beginning exposure to awake prone positioning the first day the infants are discharged from the hospital after birth for short durations of 3–5 minutes two to three times per day. 11 However, many parents of infants may remain fearful of sudden infant death syndrome. Reference Davis, Moon, Sachs and Ottolini12 Anecdotally, parents of infants with CHD also fear “putting pressure on the heart” or causing distress as well as reporting advice to restrict placing the infant prone for 2–6 weeks after surgery, so called “sternal precautions” which have never been studied or validated.
Zachry and Kitzmann examined caregiver awareness of the American Academy of Pediatrics prone play recommendation in general paediatric practice and examined why some infants are not provided tummy time. Reference Zachry and Kitzmann13 They found that many parents avoid the prone placement for play because their infant is resistant or intolerant of the position (35%) and suggest parents need education regarding the importance of providing awake prone time beginning in the first days of an infant’s life to decrease the risk of intolerance. Unfortunately, infants who experience no periods of consistent tummy time early in infancy, as is more likely in infants hospitalised for cardiac surgery, may then be more likely to show distress when placed in prone position. Ricard and Metz also reported that one-third of parents felt discouraged when infants cried when placed in prone position. Reference Ricard and Metz14 Initial exposure to tummy time can simply be implemented by placing the baby on a caregiver’s chest as early as the newborn period, a position Mendres-Smith found to be better tolerated by resistant infants. Reference Mendres-Smith, Borrero, Castillo, Davis, Becraft and Hussey-Gardner15 Parental holding and skin to skin care can be done safely in the ICU and hospital environment and benefits both infant and parent. Reference Fineman, LaBrecque, Shih and Curley16 Studies have demonstrated that prone positioning can be safely performed even in critically ill infants with acute lung injury Reference Fineman, LaBrecque, Shih and Curley16 and infants and children receiving extracorporeal membrane oxygenation. Reference Haefner, Bratton, Annich, Bartlett and Custer17 Beyond neuromotor benefits, other potential physiologic benefits of prone positioning during hospitalisation include improved respiratory and gastric function. Reference Picheansathian, Woragidpoonpol and Baosoung18 Furthermore, we have seen no adverse effects of prone positioning during or post-hospitalisation in any of our post-sternotomy infants who are encouraged to be placed in the prone position when awake by physical therapists, occupational therapists, nurses and other members of our developmental care team. In addition, there is no validated evidence within the literature that supports the “sternal precautions” that are often referenced as a rationale against tummy time.
Prone positioning is essential for strength development of the head, neck, shoulders and trunk. The World Health Organization recommends tummy time for infants because of the benefits of improved motor development and reduced likelihood of deformational plagiocephaly. 19 To our knowledge, our study was the first to examine the utility of a tummy time intervention in the CHD population who is at greater risk for developmental impairments than healthy infants. Importantly, we found infants with CHD who received at least 15 minutes of tummy time daily had significantly less motor impairment than infants with less tummy time. In a recent systematic review, tummy time was positively associated with gross motor and total development, a reduction in the BMI z-score, prevention of brachycephaly and the ability to move while prone, supine, crawling and rolling. Reference Hewitt, Stanley and Okely20 Our findings are consistent with the findings of Salls and colleagues who found that 2-month old infants from a general paediatric medical practice who spent 15 minutes or fewer of awake time in prone position passed the gross motor milestones at significantly lower percentages than the normative population. Reference Salls, Silverman and Gatty8 Majnemer and Barr also found that awake tummy time was significantly associated with AIMS scores in healthy 6-month old infants (r = 0.64) even after adjusting for potential confounders including parental age. Reference Majnemer and Barr21 Their results also suggest that infants of older, more educated parents have lower motor scores which they attribute to overprotectiveness by more educated parents. Reference Majnemer and Barr21 While data regarding parental age and education was not available in our study, overprotectiveness among parents of infants with CHD is well recognised. Reference Bjarnason-Wehrens, Dordel and Schickendantz22 Finally, Wentz compared differences in infants with Down Syndrome beginning a tummy time intervention before 11 weeks of age and after 11 weeks of age. Reference Wentz23 A difference in motor development between early and later groups was apparent at 1, 2 and 3 months following intervention initiation supporting the earlier implementation of tummy time, at a time when many neonates may be hospitalised for cardiac surgery.
As noted by Wentz, Reference Wentz23 there is potential for tummy time to be an impactful intervention in infants, if the family is willing to engage in the activities as recommended. In a qualitative study of barriers and facilitators of tummy time, parents reported that modelling was incredibly helpful. Reference Felzer-Kim, Erickson, Adkins and Hauck24 Several participants found it empowering to watch staff model the tummy time exercises with their infant. This might be especially important during hospitalisation for parents of infants with sternal incisions. However, in spite of the recognised respiratory benefits of prone positioning, many institutions prohibit prone positioning in post-operative patients for several weeks after surgery. A recent survey of healthcare providers found that 80% of respondents reported having institutional protocols for paediatric sternal precautions for 1–8 weeks after surgery, including prone positioning restrictions in 58% of the reported institutions.25 In addition, providers may consider positional plagiocephaly which might be prevented by prone positioning as cosmetic and developmental delays as temporary, failing to recognise the potential cascading of delays and consequences related to inability to explore the environment and develop adaptive skills. The restriction period communicated by providers may be extended even longer by overanxious parents. Caregiver education that directly addresses caregiver concerns is essential, Reference Felzer-Kim, Erickson, Adkins and Hauck24 which prompted us to include an intervention group that included outpatient reinforcement to address parental concerns and barriers. However, we did not detect a difference between intervention groups with and without planned outpatient contacts. It is possible that nurse coordinator follow-up for study measurements provided similar reinforcement and study participation influenced behaviour in all groups. Developmental rounds instituted during the study may have also provided greater focus on developmental needs across all infant groups. We have especially focused developmental resources/therapies post-operatively on infants who spend greater than 5 days in the ICU as this was associated with greater motor impairment during hospitalisation unrelated to surgical complexity in our earlier work. Reference Uzark, Smith, Donohue, Yu and Romano4 Finally, another common barrier identified by Felzer-Kim et al is finding time to do tummy time, especially among single or working parents or related to sibling demands. Reference Felzer-Kim, Erickson, Adkins and Hauck24 A limitation of our study is a lack of information on family characteristics. We also acknowledge that parental estimates of the amount of awake tummy time rely on memory and 24-hour recall. Logging of actual tummy time was not required to avoid adding to the parental burden.
Conclusions
In conclusion, our results highlight the value of tummy time to decrease motor impairment in infants with CHD at increased risk for developmental delays. We recommend modelling prone positioning during hospitalisation and avoidance of sternal precautions that unnecessarily prohibit prone positioning. Involving parents through education and active participation in the infant’s developmental care during hospitalisation may encourage parenting behaviours such as tummy time to promote optimal infant development after discharge. Further research is needed to evaluate the potential of tummy time during and following hospitalisation in a larger sample and to elucidate factors to promote parental compliance with tummy time recommendations to optimise neurodevelopmental outcomes in infants with CHD.
Acknowledgements
We would like to acknowledge the support of the physical therapists who performed the Alberta Infant Motor Skills assessments.
Financial support
This project was supported in part by the Nina Starr Braunwald Career Development Award from the Thoracic Surgery Foundation and a gift from the Norman family.
Conflicts of interest
None.







