The long term sequels of acute rheumatic fever continue to be a major cause of cardiac disease in young children and adolescents throughout the world, especially in a developing country like India.Reference Sanyal, Berry, Duggal, Hooja and Ghosh1 Amongst the various manifestations of acute rheumatic fever, only carditis leads to morbidity and mortality during the acute stage of the disease, subsequently leading to permanent damage due to chronic rheumatic disease. Despite the modification of the Jones’ criterions,Reference Jones2 and their revision four times,3, 4 carditis is either under-diagnosed during the acute phase, leading to nearly half of patients with established rheumatic disease not receiving prophylaxis, or over-diagnosed when determined on the basis of traditional characteristic auscultatory findings.5 Accurate diagnosis of carditis, nonetheless, is important, as timely management can normalize the situation in up to two-fifths of cases, preventing recrudescence of rheumatic activity and further damage to the valves. Despite the fact that carditis can more accurately be diagnosed echocardiographically than with traditional auscultatory findings,Reference Narula, Chandrasekhar and Rahimtoola6, Reference Vijayalakshmi, Mithravinda and Deva7 and can prevent both over-and under-diagnosis,Reference Vijayalakshmi and Manoria8 the efficacy of echocardiography remains in doubt.Reference Albert, Harel and Karrison9, Reference Park10 Hence, the committee revising the Jones’ criterions remains sceptical about the inclusion of echocardiographic evaluation as a major criterion, for fear of prompting over-diagnosis of carditis.Reference Ferrieri11 The need remains, therefore, to prove the validity of echocardiographic evaluation in the diagnosis of clinical and subclinical carditis. The aim of this prospective study, therefore, was to test the utility, efficacy, specificity and sensitivity of echocardiographic criterions for the precise and early diagnosis of both clinical carditis and subclinical valvitis in patients with acute rheumatic fever.
Material and methods
From January, 2006, through June, 2007, we enrolled 333 consecutive patients with suspected acute rheumatic fever, of whom 165 were males and 168 were females. In our double-blinded study, the detailed clinical examination and laboratory tests were undertaken by 3 experienced paediatricians. Echocardiographic evaluation was performed by one expert echocardiographer, who did not know the clinical diagnosis. All forms then contained both clinical and echocardiographic findings, the latter used as the gold standard. During the final analysis, the paediatric cardiologist assessed the sensitivity and specificity of the Jones’ criterions for diagnosis of carditis and valvitis.
Clinical methods: The detailed clinical data of all patients was entered in a specially designed database. The prolapsing leaflets of the mitral valve in patients with rheumatic fever produce muffled heart sounds and a pansystolic murmur. After echocardiographic confirmation, therefore, we excluded from the study any patients with the classical auscultatory findings of myxomatous mitral valvar prolapse, such as a midsystolic click, or multiple clicks followed by a midsystolic to late systolic murmur at the apex of the left ventricle. Careful auscultation was done in sitting and bending forward position to detect the early diastolic murmur of aortic regurgitation. The clinically detected systolic murmur of tricuspid regurgitation was noted. All the patients were auscultated carefully to identify any pericardial rub or cooing murmur.
Echocardiographic methods: All the patients underwent meticulous cross-sectional echocardiographic and Doppler interrogation using a commercially available Philips Sonos 5500 system interfaced with a 3.5 megaherz transducer . The data was entered in a specially designed database. The thickness of the mitral valvar leaflets was measured at the base, the middle parts, and the tips of the leaflets in diastole. The thickest portions of the aortic and mural leaflets of the mitral valve, along with the leaflets of the tricuspid and aortic valves, were measured in millimetres in the parasternal long axis, apical four chamber, and five chamber views. The valvar thicknesses equal to or less than 4 millimetres were taken as normal, and thicker leaflets deemed to be abnormal. The presence or absence of hyperechogenicity of the tension apparatus was noted. Excursion of the leaflets was recorded to establish whether mobility was normal, reduced, or increased. Mitral valvar prolapse was diagnosed by measuring the maximal superior systolic displacement of the leaflets relative to the line connecting the annular hinge points. Displacements of the leaflets were measured in the parasternal long-axis and apical four chamber views. It is an easy matter echocardiographically to differentiate the redundant, elongated myxomatous prolapsing leaflets from rheumatic leaflets, which have thickened and shortened cords, with reduced mobility and a beaded appearance. We noted prolapse of either the aortic, mural, or both leaflets, also noting any cordal tears, rolled cords, or flail leaflets. Mitral regurgitation was considered pathological only when the colour mosaic jet persisted throughout systole, and could be identified in at least two planes. The length of the jets was greater than 1 centimetre in all cases. We used the criterions of the American Society of Echocardiography for grading mitral regurgitation, Reference Zoghbi, Enriquez-Sarano and Foster12 noting whether the regurgitation jet was central or eccentric, and measuring its velocity. In similar fashion, we noted and recorded evidence of aortic or tricuspid regurgitation, using four grades of severity. The thickness of the leaflets of the mitral valve were measured in parasternal long-axis view, taking note of any beaded appearances. We also noted any evidence of pericardial effusion, and measured the dimensions of the chambers and the ejection fraction in all cases.
Our echocardiographic criterions (Table 1) for diagnosis of carditis and valvitis have previously been described.Reference Vijayalakshmi, Mithravinda and Deva7, Reference Vijayalakshmi and Manoria8 The total score was calculated by giving two points for each of the eight features of carditis in rheumatic fever. The patients with a score equal to or greater than 6 out of 16 were taken as being positive for carditis in the presence of rheumatic fever. Other causes of mitral regurgitation, including functional mitral regurgitation, were excluded, since they produce scores less than 6.
Table 1 The echocardiographic criterions.

Clinical, laboratory and echocardiographic evaluations of each episode were recorded in a specially designed computerized database and analyzed systematically. Out of 333 patients suspected of having acute rheumatic fever, only 272 fulfilled the criterions for carditis and subclinical valvitis. These patients forming the focus group, with the remaining 61 patients serving as controls.
Results
In Table 2, we show the incidences of the various observed echocardiographic features. An increase in thickness of the aortic leaflet of the mitral valve was the commonest feature, found in 279 cases (83.8% – Fig. 1). A thickened leaflet was detected in 310 cases (93%) with the use of tissue harmonics, but we excluded this data from our study. A thickened mural leaflet was identified in 188 cases (56.5%) with echocardiography, but in 250 cases (75%) when tissue harmonics were used. Reduced mobility of the mural leaflet was observed in 121 cases (36%), but of the aortic leaflet in only 55 cases (16.5%).
Table 2 The incidence of various echocardiographic features.

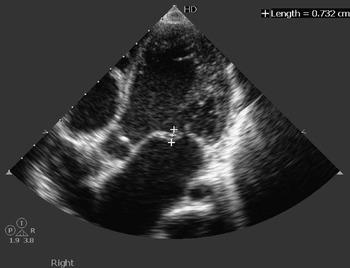
Figure 1 The echocardiogram in the apical five chamber view shows thickened leaflets of the aortic and mitral valves.
Out of the 333 patients, 272 fulfilled our echocardiographic criterions. Of the total group, 220 (66.06%) patients were diagnosed positively using these criterions and the Jones’ criterions. Of the others, 52 (15.61%) had no murmur, but were positive as assessed using echocardiography. They were taken as subclinical carditis presenting late, as they had arthralgia with negative titres of antistreptolysin, and hence were negative when assessed using the Jones’ criterions. In 4 patients, diagnosed as having carditis using the Jones’ criterions, echocardiographic study revealed an atrial septal defect with mitral valvar prolapse, myxomatous mitral valvar prolapse, aortoarteritis with mitral regurgitation, and a subaortic fibrous shelf, respectively. In the remaining 57 suspected patients who were considered negative using the Jones’ criterions (17.11%), echocardiographic study also proved negative. These patients, therefore, became our control group (Fig. 2). Using this data, our echocardiographic criterions had a sensitivity of 81%, and specificity of 93%.

Figure 2 .Results.
Out of 239 patients with pathological mitral regurgitation revealed echocardiographically, only 144 had a systolic murmur on auscultation. Aortic regurgitation was detected echocardiographically in 60 patients, whereas a soft blowing early diastolic murmur was heard clinically in only 11. We detected tricuspid regurgitation echocardiographically in 60 patients, but heard a corresponding murmur in only 9 cases (Fig. 3).

Figure 3. Clinical and echocardiographic correlation in mitral, aortic and tricuspid regurgitation.
Rheumatic nodules, or a beaded appearance (Fig. 4) were seen in 159 cases (47.7%). Mitral valvar prolapse, with thickened leaflets, was seen in 202 cases (83.69%), while tricuspid valvar prolapse with thickened leaflets was seen in only 42 cases (12.6%). We identified torn cords in 5 patients (1.5%), of whom 3 had severe mitral regurgitation due to flail leaflets (0.9%). Although a pericardial rub was not appreciated clinically in any of the patients, pericardial effusions were detected echocardiographically in 12 cases (3.6%).

Figure 4 Histopathological examination (Panel a) shows a beaded appearance of the mitral valve. The short axis echocardiographic view (b) shows a similar appearance.
Discussion
According to the World Health Organisation, at least 15.6 million people have rheumatic heart disease, and 0.3 million out of 0.5 million individuals who acquire acute rheumatic fever every year develop rheumatic heart disease later. In each year, 233,000 deaths are directly attributable to acute rheumatic fever or rheumatic cardiac disease. Hence, detection of active rheumatic carditis is of great prognostic and therapeutic importance. This is currently based on the use of the Jones’ criterions.5, Reference Vijayalakshmi, Mithravinda and Deva7 The diagnosis of carditis in acute rheumatic fever traditionally depends on characteristic auscultatory findings, like the detection of a new murmur which was not present earlier, cardiomegaly, congestive cardiac failure, and findings of a pericardial rub. These auscultatory findings are unreliable in developing countries, where it is difficult to identify a new murmur from preexisting murmur. Cardiomegaly could be due to any other cause, and not necessarily acute rheumatic fever. Similarly, congestive cardiac failure could be due to viral myocarditis or cardiomyopathy. Especially in India, a pericardial rub could be due to tubercular pericarditis. Hence, rheumatic carditis cannot be diagnosed clinically with precision, especially in an era when cardiac auscultation is taught less extensively, and is used with less confidence by young clinicians. Of our cohort, 108 patients were shown echocardiographically to have subclinical carditis, but not by clinical auscultation. Of these, only 56 patients would be deemed positive using the Jones’ criterions. Even highly skilled clinicians, therefore, do not always hear the murmur in patients with subclinical carditis.
It is estimated that more than seven-tenths of patients with established rheumatic heart disease do not receive secondary prophylaxis.Reference Strasser, Dondog and El Kholy13 The carditis, especially subclinical valvitis, is mostly missed by the best of clinicians. There is no single laboratory test that definitely establishes the diagnosis of carditis. Our study clearly shows that the simple, non-invasive and reproducible technique of echocardiography combined with Doppler interrogation can effectively overcome the limitations of the Jones’ criterions in detecting carditis. Rheumatic carditis is almost always associated with valvitis. The valvitis constitutes the phenotypic feature of rheumatic carditis, hence echocardiographic documentation of valvar and subvalvar changes can be of significant help (Fig. 5).

Figure 5. The images from a 12 year old girl with acute rheumatic fever show thickened leaflets of the aortic and mitral valves, which have a beaded appearance, hyper-echogenicity of the submitral structures, mitral valvar prolapse with mitral regurgitation, giving an overall echocardiographic score of 10, with 2 points each for the mitral valvar prolapse, regurgitation, thickened leaflets, hyper-echogenicity of the submitral structures, and the beaded appearance.
The American Heart Association recommends not making the diagnosis of acute rheumatic carditis without audible murmurs of mitral regurgitation or aortic regurgitation, but this is debatable.Reference Park10 Significant echocardiographic abnormalities may be present in the absence of any audible murmur. The echocardiographic findings can determine the severity of cardiac enlargement, the presence and degree of mitral regurgitation and aortic regurgitation and the presence of pericardial effusion more objectively. Inclusion of echocardiographic findings, therefore, may enhance the correct diagnosis of carditis in acute rheumatic fever.Reference Narula, Chandrasekhar and Rahimtoola6, Reference Park10 In our study, 239 cases of mitral regurgitation were detected by echocardiography, but an audible murmur of mitral regurgitation was present only in 144 cases. This means that 95 patients with mitral regurgitation would have remained undetected, and would not have received penicillin prophylaxis, if not for echocardiographic diagnosis.
Others have concluded previouslyReference Cotrim, Macedo, Duarte and Lima14 that early echocardiographic interrogation is very important in all children suspected to have acute rheumatic fever, especially as mitral regurgitation can be demonstrated by colour flow mapping in absence of cardiac murmur. The pulse and colour Doppler echo provide a method to detect minor degree of pathological regurgitation without characteristic clinical signs.Reference Wilson and Neutze15 Doppler echocardiography is more sensitive than clinical assessment in the detection of carditis in acute rheumatic fever, and can also contribute to the early diagnosis.Reference Wilson, Neutze, Voss, Lennon and Ameratunga16, Reference Abernethy, Bass and Sharpe17 We detected the early diastolic murmur of aortic regurgitation clinically in only 11 cases, but aortic regurgitation was revealed echocardiographically in 60 cases. Similarly, the systolic murmur of tricuspid regurgitation was clinically detected only in 9 cases, but echocardiographic interrogation detected tricuspid regurgitation in 60 patients. All these patients had other evidence of rheumatic carditis. We are not over diagnosing the physiological regurgitation, because according to our echocardiographic criterions, we do not consider the regurgitation to be rheumatic unless we find more than 3 abnormal parameters, thus decreasing the chance of physiological valvar regurgitation being wrongly labeled as pathological. The echocardiographic study, therefore, not only helps in making a precise diagnosis, but also aids in determining the strategies for management when severe mitral regurgitation is due to cordal tear, as found in 5 of our patients. The cost of echocardiographic interrogation at the beginning of the disease, and the cost of penicillin prophylaxis, is negligible, when compared to the human suffering and cost of the management with valvar repair or replacement. We have shown in this study that our echocardiographic criterions are both sensitive and specific. We submit that such echocardiographic findings should now be accepted as a major criterion for the diagnosis of carditis in rheumatic fever.
Long-term follow-up is necessary, nonetheless, to determine the outcome in young children with subclinical echocardiographic evidence of valvar disease.Reference Tani, Veasy, Minich and Shaddy18 As stated by Kaplan, ‘The fact that penicillin has clearly failed to eradicate this disease process is irrefutable proof to many of the need for more laboratory, epidemiological, and clinical research’.Reference Kaplan19 In fact, it is the lack of precise diagnosis of carditis, and lack of penicillin prophylaxis, rather than the failure of penicillin. If echocardiography is used as a primary diagnostic modality, and is included in the Jones’ criterions for diagnosis, it is likely to change the epidemiological face of acute rheumatic fever and rheumatic heart disease completely, as more patients can be brought into the net of penicillin prophylaxis. The Australian and New Zealand Guidelines for Rheumatic Fever Diagnosis, Management and Secondary Prevention recommends that all patients with suspected or definite acute rheumatic fever, should undergo echocardiography, if possible, to identify evidence of carditis.20, 21 The incidence of Erythema marginatum was shown to be less than 0.4% in our earlier study.Reference Vijayalakshmi, Mithravinda and Deva7 No patient with Erythema marginatum was seen in this large study. Today, Erythema marginatum is irrelevant as a major criterion. It would be an easy matter, therefore, to replace this finding with abnormal echocardiographic findings as a major criterion.
In conclusion, we believe that early and precise diagnosis of carditis in acute rheumatic fever, though difficult, is very important in preventing serious consequences, morbidity and mortality in young. Echocardiographic criterions are now very important in providing precise diagnosis of carditis or subclinical valvitis. These subclinical changes, detected only by echo, can persist and probably belong to a large group of patients who present later as rheumatic heart disease, without the past history of acute rheumatic fever and prophylaxis. These echocardiographic criterions, therefore, should now be included as one of the major criterions in the Jones’ system to permit diagnosis of carditis in the setting of acute rheumatic fever.
Acknowledgements
We are grateful to Smt. B.V. Sumangala, who performed all the echocardiographic studies. We thank also Mrs. Maya and Dr.Vittal Shenoy, Charlotte, North Carolina, for financial assistance, and Mrs. Shreya and Mr. Shreyas for preparing the database and analyzing the data.









