Kawasaki disease is an acute vasculitis syndrome of infants and young children predominantly affecting small and medium-sized arteries with predilection for coronary arteries. Reference Newburger, Takahashi and Gerber1,Reference McCrindle, Rowley and Newburger2 Coronary artery abnormalities in Kawasaki disease can occur in 15–25% of untreated children and at least 3–5% of children who received appropriate treatment with intravenous immunoglobulin. Long term complications include persistence of aneurysms, stenosis, occlusion, and thrombosis leading to myocardial infarction and death. Reference Newburger, Takahashi and Gerber1–Reference Tsuda and Singhal4
Kawasaki disease leads to endothelial dysfunction in acute phase and this has been well documented in published literature. Reference Ghelani, Singh and Manojkumar5–Reference Routhu, Singhal and Jindal6 Whether Kawasaki disease predisposes to premature atherosclerosis is still not clearly established. Reference Noto, Okada and Karasawa7–Reference Chen, Zannino and Curtis10 However, there are concerns that patients with Kawasaki diseasemay go on to develop atherosclerosis in early adulthood.
Computed tomography coronary angiography is an upcoming modality to evaluate coronary arteries in children with Kawasaki disease. Till recently, radiation exposure after computed tomography coronary angiography had been the major limiting factor for carrying out this investigation in children. Reference Brenner and Hall11–12 However, with advent of high detector and dual source computed tomography scanners, radiation concerns have largely been addressed. Reference Khan, Khosa and Nasir13–Reference Singhal, Singh and Gupta17 Moreover, computed tomography coronary angiography has been shown to perform much better than echocardiography for assessment of aneurysms in left circumflex artery and distal portions of coronary arteries. Reference van Stijn-Bringas Dimitriades, Planken and Groenink18
We have conducted a prospective study to evaluate the status of coronary arteries on computed tomography coronary angiography at least 10 years after the acute episode of Kawasaki disease. Calcium scoring (Agatston’s algorithm) was used as a surrogate marker for premature atherosclerosis.
Materials and methods
Study population
Study was carried out on 21 patients with Kawasaki disease who had been on follow-up for more than 10 years at the Paediatric Rheumatology Clinic of our institute, which is a federally funded not-for-profit tertiary care teaching center. Diagnosis of Kawasaki disease was based on the American Heart Association 2004 criteria. Reference Newburger, Takahashi and Gerber1 Patients were treated using standardised protocols – intravenous immunoglobulin infusion (2 g/kg) and aspirin (initially in high doses, and then in anti-platelet doses).
All participants were interviewed, and clinical history related to cardiovascular diseases including history of myocardial infarction, angina, coronary artery bypass graft or angioplasty, transient ischemic attack, cerebral vascular accident, peripheral vascular disease, and congestive heart failure was recorded. Relevant risk factors including dyslipidemia, hypertension, active smoking, diabetes, and family history of cardiovascular disease were also noted.
Study protocol conforms to the ethical guidelines of the 1975 Declaration of Helsinki. Study protocol was approved by the Institute Ethics Committee and Institute Thesis Committee. The final manuscript was approved by the Department Review Board. Assent was taken from the patients and written informed consent was taken from parents of patients.
CT scanner
Study was carried out on 128 Slice Dual Source computed tomography scanner (Somatom definition flash, Siemens, Erlangen, Germany) with gantry rotation time 0.28 seconds with temporal resolution of 75 ms.
Measurement of coronary artery calcification
Non-contrast electrocardiography-gated scans with prospective electrocardiography gating and breath holding were obtained with area coverage from floor of carina to base of heart for measurement of calcifications in coronary arteries. Calcification in arterial wall is considered as surrogate marker of atherosclerosis. Reference Lara, Ros and Sierra19,Reference Malguria, Zimmerman and Fishman20
Images were analysed on dedicated workstation using proprietary software (Syngovia, Siemens, Erlangen, Germany). Calcium scores were calculated by algorithm suggested by Agatston et al by determining the density of the highest density pixel in each plaque taking the threshold of 130 Hounsfield Units and applying a weighting factor to each plaque, depending upon peak density in the plaque: (area.cofactor; 1:130–199 Hounsfield Units; 2:200–299 Hounsfield Units; 3:300–399 Hounsfield Units; 4:>400 Hounsfield Units). Reference Agatston, Janowitz and Hildner21 An electronic region of interest was placed around each highlighted coronary arterial calcification and location assigned as under: left main coronary artery, left anterior descending, left circumflex, or right coronary artery. Branches of the respective arteries were considered parts of these arteries. Similarly, calcium volume was also calculated automatically by the software for each specified artery.
Computed tomography coronary angiography protocol
Computed tomography coronary angiography was performed using non-ionic contrast (Omnipaque 350, GE Healthcare, Ireland) injected at a rate of 4 ml/second (through 20 gauge cannula) in right antecubital vein. This was followed by a saline push at the same rate of contrast for 10 seconds through dual head power injector. Acquisition was carried out using bolus tracking technique with circular region of interest set at level of the descending thoracic aorta with threshold attenuation value of 100 Hounsfield Units. Oral metoprolol (2 mg/kg body weight) was administered to all children 30 minutes prior to computed tomography coronary angiography. The aim was to achieve a low and stable heart rate.
Radiation exposure was optimised using adaptive prospective electrocardiography-gated sequence, automated tube current modulation (care dose 4D; Siemens health care), lower kilo-voltage (kVp) settings (fixed at 100 kVp), and iterative image reconstruction algorithms.
Post-processing was done on a dedicated Syngovia workstation for reconstruction of coronary arteries. Curved multi-planar reconstruction, maximum intensity projection, and volume rendered images were reviewed by a cardiac radiologist (MS) who was blinded to details of clinical profile and other investigations. A second radiologist (RKC) correlated computed tomography coronary angiography data with clinical data and other investigations.
Assessment of coronary arteries
Coronary arteries were evaluated for abnormalities that included aneurysms, thrombo-occlusive-stenotic lesions and mural calcifications.
Results
Twenty-one children who were diagnosed to have Kawasaki disease at least 10 years ago were enrolled in the study. All patients were free of known cardiovascular disease/s and 16 patients did not have family history of cardiovascular disease.
Mean age of enrolled patients was 15.76 (±3.72) years and male to female ratio was 5:2 (15 males; 6 females). Minimum and maximum age at diagnosis of Kawasaki disease was 0.5 and 8 years respectively. Mean age of patients at time of diagnosis was 3.21 (±2.48) years. Minimum and maximum time interval from the onset of Kawasaki disease to imaging was 10 years and 22.5 years, respectively, with mean of 12.59 (+2.89) years.
Effective Radiation Dose in millisieverts (mSv) was derived by multiplying dose length product by a conversion factor (0.014) as per International Commission on Radiological Protection 103 guidelines. 22 Dose length product value is automatically generated after completion of computed tomography scan.
The minimum and maximum dose length products were 100 and 587 mGycm with median 204 mGycm and mean dose length product 256.76 + 126.45 mGycm. The median dose length product was 204 mGycm. Estimated effective dose was 1.4–8.2 mSv, and the median was 2.85 mSv with mean 3.59 + 1.77 mSv.
Coronary artery calcification scores
Coronary artery calcification was seen only in one patient (P1) (4.76%). Calcification was noted in saccular aneurysm in proximal segment of right coronary artery and fusiform aneurysm in proximal left anterior descending artery (Figs 1 and 2). Coronary artery calcification was noted only in aneurysmal portion with high calcium scores (volume score- 495 mm3 and Agatston’s score- 484.4) corresponding to coronary artery age >70 years. This patient also had fusiform aneurysm in proximal left circumflex artery. However, no calcification was seen in this segment (Fig 2). He had no cardiac risk factor.

Figure 1. Computed tomography derived coronary artery calcification images in a 13-year-old male with Kawasaki disease diagnosed at 2.5 years of age (P1) show focal calcification in proximal segments of right coronary artery and left anterior descending arteries (arrows in a and b). Coronary artery calcification Agatston’s score was 484.4 (c). Note: CX = circumflex artery; LAD = left anterior descending artery; LM = left main artery; RCA = right coronary artery.

Figure 2. Computed tomography coronary angiography curved reformatted maximum intensity projection images of patient described in Figure 1 (P1) shows a peripherally calcified medium size (5.3 mm in diameter) saccular aneurysm in proximal segment of right coronary artery (arrow in a ) and partially calcified fusiform aneurysm in proximal segments of left anterior descending (arrow in b ). Volume rendered image (c) shows small fusiform aneurysms (thin arrows) in proximal segments of left anterior descending and circumflex arteries. Note: saccular aneurysm in proximal segment of right coronary artery (thick arrow).
Coronary artery abnormalities
Four children had echocardiography evidence of coronary artery abnormalities at time of diagnosis of Kawasaki disease. Two had transient dilatation of left main coronary artery (2–2.5 z score), while the remaining two children (P1, P2) continued to have persistent coronary artery abnormalities. Patient P1 had echocardiography evidence of giant aneurysm in proximal left anterior descending artery (10 × 9 mm) and moderate-sized aneurysm in right coronary artery (maximum dimension: 5.8 mm) at time of diagnosis. Size of aneurysms in left anterior descending and right coronary arteries regressed (maximum dimension noted at 3rd year follow up: 4.3 and 2 mm, respectively) on follow-up echocardiography examination. Patient P2 had evidence of fusiform aneurysm in mid-portion of left anterior descending artery (maximum dimension: 5 mm) at time of diagnosis that regressed on follow-up echocardiography (maximum dimension at 2nd and 4th year follow-up was 3.2 and 2.7 mm, respectively).
Computed tomography coronary angiography done in patients P1 and P2, 10.5 years and 13 years after diagnosis of Kawasaki disease, respectively, showed abnormalities in form of aneurysm: saccular aneurysm-1; fusiform aneurysms-3. Patient P1 had medium sized (5 to <8 mm) saccular aneurysm noted in proximal segment of right coronary artery that measured ˜5.3 mm in diameter with neither a filling defect (to suggest thrombus) nor a stenosis (Fig 2). Left anterior descending and left circumflex arteries in the same patient showed small (<5 mm)fusiform aneurysms in their proximal segments measuring 3.1 and 3.4 mm in diameter, and 22 and 13 mm in length, respectively (Fig 2). Small fusiform aneurysm was present in proximal left anterior descending artery in the second patient (P2) measuring ˜4.4 mm in diameter and ˜22 mm in length (Fig 3). No calcification was, however, observed in aneurismal or normal segments of the coronary arteries in this patient.
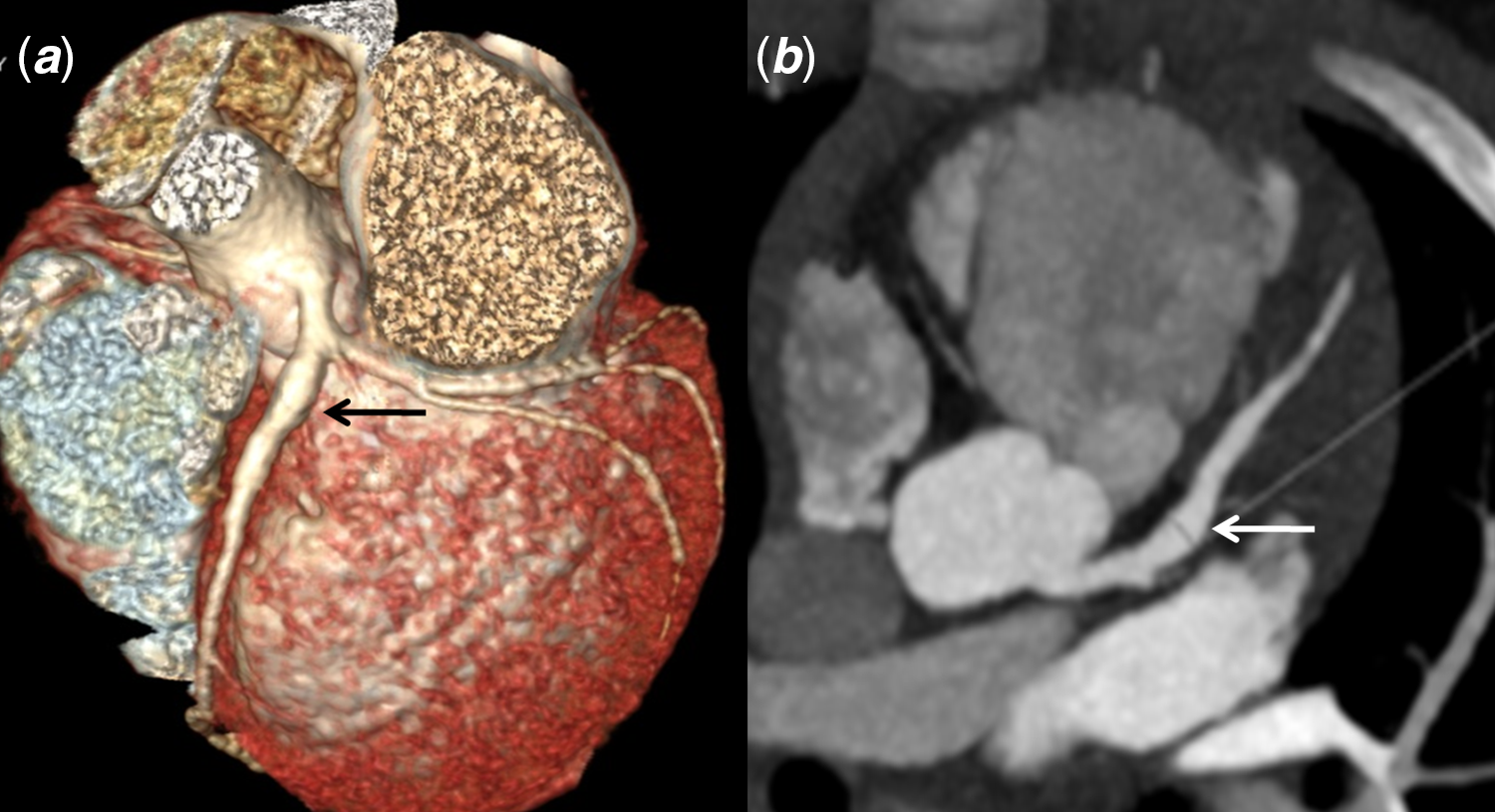
Figure 3. Volume rendered and axial maximum intensity projection computed tomography coronary angiography images of 14-year-old boy with a history of Kawasaki disease at 1 year of age (P2) show a fusiform aneurysm in proximal segment left anterior descending artery (arrows).
Discussion
Kawasaki disease predisposes to development of coronary artery abnormalities especially when there have been delays in diagnosis or treatment. While some coronary artery abnormalities are transient, others are persistent. There is no consensus on imaging modality of choice for long term follow-up of these patients. Reference Dajani, Taubert and Takahashi23,Reference de La Harpe, di Bernardo and Hofer24 While 2-dimensional echocardiography has, hitherto, been the preferred imaging modality for Kawasaki disease, it is associated with several lacunae. Reference Dajani, Taubert and Takahashi23–Reference Suzuki, Kamiya and Ono26 Echocardiography is highly operator dependent and is not suitable for delineation of middle and distal segments of coronary arteries. Further, it is difficult to visualise thrombi or coronary artery calcification on echocardiography. Catheter angiography is not suitable for young children as it is invasive and is associated with a significant radiation exposure. Reference Dajani, Taubert and Takahashi23–Reference Suzuki, Kamiya and Ono26
Over the last few years, computed tomography coronary angiography has been increasingly used in patients with Kawasaki disease. As there is paucity of literature on long term follow-up of children with Kawasaki disease using computed tomography coronary angiography, we carried out this study on a cohort of 21 children who had had Kawasaki disease at least 10 years ago. With the advent of newer generation higher slice and dual source computed tomography scanners, it is now possible to carry out computed tomography coronary angiography in children at any heart rate and with minimal radiation exposure. 12–Reference Sabarudin and Sun16 Coronary artery disease is reported to be an important cause of morbidity in patients with Kawasaki disease. Reference Dadlani, Gingell and Orie27 It is known that coronary artery calcification can be used as a surrogate marker of coronary artery disease. With the current computed tomography technology and advanced computed tomography scanners, accurate assessment of coronary artery calcification is now eminently feasible. Reference Khan, Khosa and Nasir13–Reference Malguria, Zimmerman and Fishman20
Computed tomography coronary angiography is associated with ionising radiation and its use in clinical management of Kawasaki disease should be customised according to need depending upon the presence of coronary artery abnormalities However, there is no consensus on its use in children with Kawasaki disease. In the authors’ experience, it is the best modality for assessment of longitudinal follow-up of coronary artery abnormalities in children with Kawasaki disease grow up and transthoracic echocardiography becomes difficult because of a limited acoustic window. Catheter angiography, which is otherwise a gold standard, is invasive, and is associated with inordinate radiation exposure and fails to demonstrate mural abnormalities. Further, it cannot be repeated often. Whenever computed tomography angiography is to be considered, it should always be a radiation optimised scan keeping ALARA (as low as reasonably achievable) principle with use of lower tube kilo-voltage (kVp) settings, automated tube current modulation, adaptive prospective electrocardiography-gated sequence, and iterative image reconstruction.
Presence of coronary artery calcification and its duration has been recognised as an independent risk factor for cardiovascular disease in patients with Kawasaki disease. Reference Kahn, Budoff and Daniels28 Postmortem studies have shown that extensive arterial wall dystrophic calcification occurs in coronary artery aneurysms late after Kawasaki disease. Reference Amano, Hazama and Hamashima29 Kahn et al have reported that calcification in Kawasaki disease patients occurs solely in abnormal segments of coronary arteries on electron beam computed tomography. The study concluded that significant calcifications develop after 10 years of acute episode of Kawasaki disease. Reference Kahn, Budoff and Daniels28 In another study, Kaichi et al have reported that in abnormally dilated coronary arteries, the prevalence of coronary calcification is 12% at 5 years, 44% at 10 years, and 94% at 20 years. Reference Kaichi, Tsuda and Fujita30
In our study out of total 21 subjects (all diagnosed at least 10 years back), only one (4.8%) had coronary artery calcification. We have noted calcification only in the aneurysmal segment and not in normal segments of coronary arteries. Previous studies have also noted that coronary artery calcifications were observed only in the region of coronary artery abnormalities. Reference Kahn, Budoff and Daniels28,Reference Kaichi, Tsuda and Fujita30 It appears that coronary artery calcification in Kawasaki disease is dystrophic rather than due to atherosclerosis. Coronary artery calcification is thus a long term sequel of the initial inflammation associated with abnormal dilatation and aneurysm formation in coronary arteries. Reference Dadlani, Gingell and Orie27–Reference Kaichi, Tsuda and Fujita30
Coronary artery abnormalities in Kawasaki disease are commonly noted in proximal segments as observed on serial catheter coronary angiograms. Reference de La Harpe, di Bernardo and Hofer24,Reference Amano, Hazama and Hamashima29 We have also noted coronary artery abnormalities only in proximal segments of coronaries in our study. van Stijn-Bringas Dimitriades et al compared computed tomography coronary angiography and 2-dimensional echocardiography in Kawasaki disease and noted that 56% of aneurysms were missed by echocardiography. Reference van Stijn-Bringas Dimitriades, Planken and Groenink18 Computed tomography coronary angiography identified four aneurysms in our study as compared to echocardiography that identified only one (25%) in the follow-up. Our study reiterates the fact that computed tomography coronary angiography is superior to echocardiography for evaluation of coronary artery abnormalities. Reference van Stijn-Bringas Dimitriades, Planken and Groenink18
Our study has also documented that children with Kawasaki disease with no, or only transient, coronary artery abnormalities at diagnosis had normal status of coronary arteries on long term follow-up. This finding is re-assuring for patients. Previous studies have also documented normal coronaries on 2-dimensional echocardiography on long term follow-up of children who had transient or absent coronary artery abnormalities at diagnosis. Reference Akagi, Rose and Benson31 Another important finding in our study is that there was no evidence of coronary artery calcification in segments of coronary arteries that are not involved in acute stage of Kawasaki disease. However, anatomical integrity of the vessels may not be equivalent to functional integrity. Future long term studies are needed to assess endovascular function of the normally appearing coronary artery segments in Kawasaki disease.
As this is a single-centre study on follow-up of children with Kawasaki disease10 years after the acute episode, the numbers are necessarily small. Further, the exact timing of calcium deposition remains unclear. The strength of our study is that the diagnosis of Kawasaki disease was made by the senior author in all cases. Further, standard treatment protocols were used in all patients.
Conclusions
Computed tomography coronary angiography on dual source computed tomography scanner is a feasible and appropriate imaging modality for evaluation of coronary artery abnormalities and mural calcification, on longitudinal follow-up of patients with Kawasaki disease. The modality is non-invasive, permits thorough evaluation of coronary arteries along their entire course, and demonstrates mural abnormalities.
Coronary artery calcification is seen only in the abnormal segments of coronary arteries and no calcification was documented in normal coronary artery segments. The calcifications are likely dystrophic mural calcification rather than due to atherosclerosis.
Our study suggests that computed tomography coronary angiography in follow-up may be needed only in children with Kawasaki disease who had coronary artery abnormalities at time of diagnosis. Also, if there is no evidence of coronary artery abnormalities or calcifications in computed tomography coronary angiography after 10 years of initial diagnosis, no further investigations may be necessary. Our results, however, need validation on larger cohorts and through multicentric studies.
Acknowledgements
None.
Financial support
This research received no specific grant from any funding agency, commercial or not-for-profit sectors.
Conflict of interest
None.
Ethical standards
The authors assert that all procedures contributing to this work comply with the ethical standards of the national guidelines on human experimentation (India) and with the Helsinki Declaration of 1975, as revised in 2008, and has been approved by the institutional committees (Institute Ethics Committee and Institute Thesis Committee).






