Counselling parents of foetuses or neonates with a diagnosis of hypoplastic left heart syndrome is challenging. For foetuses with hypoplastic left heart syndrome, the options are:
• termination of pregnancy,
• intention to manage with comfort care,
• intention to treat with staged surgical palliation, and
• intention to treat with primary cardiac transplantation.
For those with a postnatal diagnosis, the latter three options remain.
In our previous report,Reference Elliott1 we suggested that important differences existed in the perceptions of physicians, medical caregivers, and society with regard to the best option for the management of patients with hypoplastic left heart syndrome. The many potentially important factors in this regard include the attitudes of physicians and their estimates of outcomes for different options of management in both the short term and long term. A number of studies have examined the attitudes of surgeons, physicians, and other medical caregivers towards the management of patients with hypoplastic left heart syndrome. In particular, these studies have focussed on the recommended treatment put forward to parents of affected children as the outcome of interest and have looked at possible “independent variables”, which might influence these recommendations.Reference Kon, Ackerson and Lo2 An important limitation of these studies, however, is that the final choice made by parents may differ significantly from the recommendations made. Thus, we asked for estimates of surgeons of the actual choices made by parents at their own institutions where either an antenatal or a postnatal diagnosis of hypoplastic left heart syndrome had been made. Using the “estimates of surgeons of the actual choices made by parents at their own institutions” as our outcome of interest, we also surveyed a number of potential factors or variables influencing this outcome, including
• parental status of surgeons,
• hypothetical choice for their own children with a diagnosis of hypoplastic left heart syndrome,
• volumes for the number of Norwood (Stage I) operations performed each year at the centre, and
• estimates at their own institutions for the early, mid-, and late survival and risk of adverse neurological events and whether an acceptable 10-year quality of life was likely.
We examine the current trends in outcomes for hypoplastic left heart syndrome in the context of attitudes among surgeons in European centres performing the Norwood sequence of palliative surgery, review the literature in this area, and discuss implications for the future treatment of patients with hypoplastic left heart syndrome.
Methods
We conducted a review of the literature on hypoplastic left heart syndrome published by global geographical location, as well as trends in the activity for Norwood palliation for hypoplastic left heart syndrome in recent years across European centres, as well as early mortality. The search string “hypoplastic left heart” was used to interrogate the PubMed database for total number of citations up until January, 2011. The citations were then examined individually to determine the country in which the work had been conducted.
To examine European – excluding the United Kingdom – activity for Norwood (Stage I) operations of hypoplastic left heart syndrome, data were taken from the European Association for Cardio-Thoracic Surgery Congenital Heart Surgery Database Report. Both the surgical volume and annual mortality for years 2002 to 2010 were extracted. The European Association for Cardio-Thoracic Surgery Congenital Heart Surgery Database is the largest database in Europe dealing with congenital cardiac malformations. By July, 2010, the European Association for Cardio-Thoracic Surgery Congenital Heart Surgery Database contained data on 100,265 operations performed in 84,257 patients, including 20,027 operations in neonates, 32,851 in infants, 40,020 in children, and 7367 in adults. As of July, 2010, the European Association for Cardio-Thoracic Surgery Congenital Heart Surgery Database has 334 Centres from 63 countries registered, with 140 active Centres from 37 countries submitting data. Centres from the United Kingdom do not currently submit data to the European Association for Cardio-Thoracic Surgery Congenital Heart Surgery Database; instead, they submit data to the United Kingdom Central Cardiac Audit Database.
We then performed a survey of surgeons across 14 centres – 12 European and 2 non-European – to ascertain the attitudes of surgeons to surgical palliation of patients with hypoplastic left heart syndrome in the following domains:
• how they would treat their own children;
• their estimates of choice of management by parents where an antenatal or postnatal diagnosis had been made; and
• their estimates of surgical outcomes including early and late survival and neurological risk, and whether patients were likely to have an acceptable quality of life at 10 years.
In addition, participants were questioned about the volume of their centre and how they thought this volume might influence surgical outcome. The personnel comprising the teams counselling parents at different stages were also ascertained for the centres of the respondents. Addresses for e-mail for participants were obtained from the database of the list of members of the European Congenital Heart Surgeons Association. The survey was administered in April, 2011 and closed after 3 months. Reminders were sent at 1-month intervals where responses had not been obtained.
Results
Search of the PubMed database revealed a total of 2392 citations for “hypoplastic left heart” up until January, 2011. Of these, the plurality, 764 were from the United States of America (Fig 1). The United Kingdom, Germany, Italy, and Japan were the centres with the most citations after the United States of America. The European Association for Cardio-Thoracic Surgery Congenital Heart Surgery Database showed that the number of Norwood (Stage 1) operations has been steadily increasing up until 2009 with 272 Norwood (Stage 1) operations in 2009, reaching a plateau with 205 procedures in 2010 (Fig 2). There has, however, been a steady reduction in the mortality for the Norwood (Stage 1) operations from 2003–2007 across European centres, with a plateau from 2008–2010 (Fig 2).

Figure 1 Number of citations in PubMed for the search string: “hypoplastic left heart” by country as of January 2011.

Figure 2 Data from The European Association for Cardio-Thoracic Surgery Congenital Heart Surgery Database documenting the Number of Norwood (Stage 1) operations and their 30-day Mortality by Year.
With regard to the data obtained from the survey of surgeons, of the 14 centres, two were from non-European centres (Melbourne, Australia and Riyadh, Saudi Arabia). Of these, six were low-volume centres for Norwood (Stage I) operations, defined as less than 10 procedures per year. Of the remainder, two were high-volume centres performing greater than 20 procedures per year, and the others were mid-volume centres performing 11 to 20 procedures per year (Table 1). Only 4 out of 14 centres, however, reported that the number of Norwood (Stage I) operations had increased, with six reporting unchanged numbers and four centres reporting reduced numbers.
Table 1 Number of Norwood procedures per year and perceptions of effects of the volume of Norwood procedures on outcome.

Volume-outcome: 1 = yes, 0 = no; number of Norwoods changed: 1 = up, 2 = down, 3 = similar
The reported estimates of survival provided by surgeons varied widely, with estimates of survival at 1 year ranging from 30% to 90%. Estimates of survival at 5 and 10 years were in the range from 25% to 80% and 20% to 75%, respectively (Table 2).
Table 2 Estimates of surgeons of survival, neurological outcome, and quality of life by centre.

0 = no; 1 = yes; 2 = only if asked; nr = no response; ns = not stated
With respect to neurological outcomes, the quoted risk of serious adverse neurological outcome was 10–30%. Of 13 surgeons, nine would provide this information, one would not, and three centres would provide these data only if asked. Of 14 centres, five advised that the quality of life at 10 years would be acceptable (Table 2).
All respondents reported being parents. If a hypothetical antenatal diagnosis of hypoplastic left heart syndrome would be made for their own offspring,
• 11 out of 16 surgeons (68.75%) would choose termination of pregnancy,
• 4 out of 16 surgeons (25%) would choose Norwood palliation, and
• 1 out of 16 surgeons (6.25%) would choose continued pregnancy and comfort care.
If a hypothetical postnatal diagnosis of hypoplastic left heart syndrome would be made for their own offspring,
• 50% would choose Norwood palliation and
• 50% would choose comfort care.
Overall, two-third of respondents reported that attitudes to the management of hypoplastic left heart syndrome had changed in their country, with 56.2% reporting that attitudes had changed in their individual centre. All except one of these centres where attitudes were reported to have changed replied that number of Norwood procedures had increased; a single centre with changing attitudes reported a decline in the number of Norwood procedures.
Reported estimates of termination of pregnancy for an antenatal diagnosis of hypoplastic left heart syndrome varied widely across centres from 2.5% to 95% (Fig 3). Paris, Seville, Oslo, and Melbourne reported the highest estimated rate of termination of pregnancy at their centres for antenatal diagnosis of hypoplastic left heart syndrome. The highest estimates for intention to treat by surgical palliation were reported from Leicester (United Kingdom), Warsaw (Poland), Riyadh (Saudi Arabia), and Saint Augustin (Germany). The latter three centres also reported estimates that the majority of parents at their centres would opt for Norwood palliation in the case of a postnatal diagnosis (Fig 4). Paris, Prague, and Denmark reported estimates of equipoise – an even distribution of choice – between Norwood palliation and comfort care where a postnatal diagnosis had been made.

Figure 3 Reported estimates of surgeons by centre for parental choice of management of hypoplastic left heart syndrome where an antenatal diagnosis had been made.
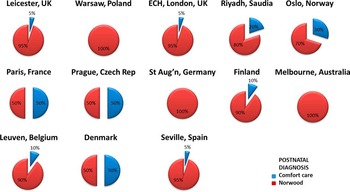
Figure 4 Reported estimates of surgeons by centre for parental choice of management of hypoplastic left heart syndrome where a postnatal diagnosis had been made.
With regard to counselling parents of a foetus with the antenatal diagnosis of hypoplastic left heart syndrome at individual centres (Table 3)
Table 3 Counsellors by speciality for antenatal or postnatal diagnosis of hypoplastic left heart syndrome by centre.

ICU = intensive care unit
1 = obstetrician; 2 = cardiologist; 3 = cardiac surgeon; 4 = psychologist; 5 = all; paeds = paediatrician
• all except one centre involved a cardiologist,
• 8 out of 14 centres involved a surgeon,
• 3 out of 14 centres involved a psychologist, and
• one centre only involved a nurse-counsellor.
Most centres used cardiologists and surgeons to counsel for a postnatal diagnosis of hypoplastic left heart syndrome, with two centres involving intensive care physicians and only 3 out of 14 centres involving psychologists (Table 3).
Discussion
As of January, 2011, the European Association for Cardio-Thoracic Surgery Congenital Heart Surgery Database shows that the number of Norwood (Stage I) operations increased from 2003 to 2009, whereas 30-day mortality has decreased. Research focussing on hypoplastic left heart syndrome has also increased since 2004, with 2392 citations in the PubMed database for the search string “hypoplastic left heart”. The majority of these were from the United States of America and European centres. European rates of antenatal detection vary widely between centres, as do the rates of termination of pregnancy for a prenatal diagnosis of hypoplastic left heart syndrome as estimated by the surgeons surveyed in this study. We similarly observed a wide variation in reported estimates by surgeons for early and late survival, neurological outcomes, quality of life, and rates of termination of pregnancy.
Survival, temporal trends, risk factors, centre volume
Although the number of Norwood (Stage I) operations has been increasing in recent years, with a concomitant decline in peri-operative mortality, the estimates of survival reported by the surgeons surveyed in this study varied widely with estimates of survival at 1 year ranging from 30% to 90%. Whether this reflects the true individual institutional data would be interesting to ascertain. Estimates of survival at 5 and 10 years varied from 25% to 75% or 80%. Interestingly, the two centres in our study with the highest volume (Warsaw and Saint Augustin) did not have the highest estimates of survival at 1 year, and the reasons for this finding are not clear. Of the 14 centres in this study, four reported increasing numbers of Norwood (Stage I) operations per year. A study from Belgium has examined survival across eras for patients with congenital cardiac disease and demonstrated that this survival is improving, although that for hypoplastic left heart syndrome lags behind other complex congenital cardiac disease including transposition of the great arteries and atrioventricular septal defect.Reference Moons, Bovijn, Budts, Belmans and Gewillig3
A number of studies have shown marked improvement in the early outcomes following the Norwood (Stage I) operations in recent years, with many centres reporting 30-day survival as greater than 80%, with 1 year survival in the region of 75%.Reference Furck, Uebing and Hansen4, Reference Sano, Huang, Kasahara, Yoshizumi, Kotani and Ishino5 The major reported risk factors appear to be weight at birth, size of the ascending aorta, and the presence of associated chromosomal anomalies and extracardiac congenital anomalies.Reference Sano, Huang, Kasahara, Yoshizumi, Kotani and Ishino5, Reference Murtuza, Wall and Reinhardt6 The two main current surgical strategies for the Norwood (Stage I) operations are the Norwood (Stage I) operations using the modified Blalock–Taussig shunt and the Norwood (Stage I) operations using the Sano modification with a conduit from the right ventricle to the pulmonary artery. The recent randomised study from North America suggests that survival at 1 year is significantly better using the Sano conduit, although this difference is less apparent after 1 year.Reference Ohye, Sleeper and Mahony7 Another strategy that has been recently available is the hybrid route where bilateral bands are placed on the branch pulmonary arteries with stenting of the arterial duct, followed by a subsequent comprehensive Stage II reconstruction, thus delaying the time for more extensive surgery.Reference Galantowicz, Cheatham and Phillips8 The mid-term and long-term outcomes for this strategy are awaited, and as yet the number of centres offering this approach is limited. This hybrid approach was not therefore examined in the survey described in this manuscript, although the hybrid approach may emerge as being more important in the future. Finally, in utero approaches are a possibility for future salvage of some foetuses with hypoplastic left heart syndrome, with creation or enlargement of an interatrial communication in utero being a potential treatment that may serve to improve outcomes.Reference Marshall, Levine and Morash9
One option currently not offered in any European centre is primary transplantation for the management of hypoplastic left heart syndrome. Studies from North America, where this strategy is offered, suggest that although early outcomes are good and comparable with initial survival following the Norwood (Stage I) operation, the number of patients offered this option is declining, whereas Norwood (Stage I) operations are increasing, with concomitant decreasing mortality as in Europe.Reference Karamlou, Diggs, Ungerleider and Welke10 Transplantation is, however, an important option that should be discussed with parents, as a growing pool of patients with failing Fontan circulations in the future are likely to require transplantation, even though at present the pool of donor organs is severely limited. Another option that may emerge is long-term mechanical circulatory assistance for these patients. It is difficult to determine when these options are best discussed, as parents are overwhelmed even with the initial information given to them with regard to options after first diagnosis.
An important potential determinant of peri-operative mortality is the volume of the individual surgeon and the volume of the centre. Only two of the surveyed centres were defined as high-volume centres. A number of studies, including from our own institution, have suggested that the relationship between volume and outcome is a complex relationship influenced by a number of institutional and systematic aspects.Reference Hirsch, Gurney, Donohue, Gebremariam, Bove and Ohye11, Reference Welke, O'Brien, Peterson, Ungerleider, Jacobs and Jacobs12 It appears that the more complex a procedure for congenital cardiac disease, the more likely is the importance of higher volume, and this finding is perhaps intuitive.Reference Hirsch, Gurney, Donohue, Gebremariam, Bove and Ohye11, 13 This consideration has important implications in terms of surgical result, predicted outcomes, and therefore information provided to families during counselling for hypoplastic left heart syndrome and other conditions. This relationship of volume and outcome is also important in the context of proposals in the United Kingdom, the Netherlands, and Scandinavian countries to reconfigure services for paediatric cardiac surgery in order to achieve a smaller number of higher-volume centres with a critical mass of surgeons at each centre, as is occurring in the United Kingdom at present under the “Safe and Sustainable” national review of paediatric cardiac surgery services.Reference Hirsch, Gurney, Donohue, Gebremariam, Bove and Ohye11, 13
Functional outcomes and quality of life
Among the surgeons surveyed here, the quoted risk of major adverse neurological outcome for the Norwood (Stage I) operation varied from 10% to 30% among survey respondents. Only 9 out of 13 surgeons replied that they would electively provide this information to parents during counselling. Only 5 out of 14 centres advised that an acceptable quality of life at 10 years would be attainable. These perceptions of quality of life clearly need to be modified by the increasingly available data. Gaynor et alReference Gaynor, Gerdes and Nord14 have examined neurodevelopmental outcome after cardiac surgery in infancy and found that patients with hypoplastic left heart syndrome tended to have lower scores for cognition, fine motor skills, executive function, and mathematics skills compared with patients with transposition of the great arteries, tetralogy of Fallot, and ventricular septal defect, although these differences appeared not to be significant after correction for demographic, pre-operative, and intra-operative variables. Interestingly, although the use of deep hypothermic circulatory arrest may partly account for these differences, it has been shown in a study using magnetic resonance imaging that the brains of patients with hypoplastic left heart syndrome are less developmentally mature before surgery when compared with controls as assessed by degrees of myelination, cortical infolding, and other parameters,Reference Licht, Shera and Clancy15 thus providing evidence of an organic substrate for worse neurodevelopmental outcome.
Brosig et alReference Brosig, Mussatto, Kuhn and Tweddell16 have conducted a study on the psychosocial outcomes for patients and their families following surgery for complex congenital cardiac disease and included patients with hypoplastic left heart syndrome and transposition of the great arteries. Parents of patients with palliated hypoplastic left heart syndrome reported greater stress on the family and negative impact on the family compared with parents of patients with transposition of the great arteries. Further, patients with hypoplastic left heart syndrome had higher rates of behavioural disorders.Reference Brosig, Mussatto, Kuhn and Tweddell16 A similar study from Alberta, Canada, also found that patients after the Norwood (Stage I) operation had lower intelligence quotient scores compared with patients with transposition of the great arteries, and those patients with chromosomal abnormalities also had lower intelligence quotient and verbal scores at 5 years compared with those who did not.Reference Creighton, Robertson and Sauve17
With regard to somatic growth of patients after surgical palliation for hypoplastic left heart syndrome, one study has found that somatic growth is significantly retarded after the Norwood (Stage I) operation, although somatic growth recovers following Stage II palliation.Reference Srinivasan, Jaquiss and Morrow18 With regard to exercise capacity, both the uptake of oxygen at the anaerobic threshold and maximal uptake of oxygen are reduced in patients following Stage III palliation compared with healthy controls; these patients also exhibited a reduced maximal heart rate and stroke volume increment response, as well as evidence of an abnormal ventilatory response to exercise.Reference Moller, Weitz and Jensen19 These investigators concluded, however, that the degree of impairment should not result in discouraging these patients from participating in activities at school and sports.
A study from Sweden has examined quality of life in children with hypoplastic left heart syndrome using a survey questionnaire to ascertain socio-economic status, structures and function of familial networks, and psychosocial well-being. This study found that patients, compared with healthy children as controls, had lower self-esteem, more psychological symptoms, lower peer-group acceptance, and a significantly lower quality of life.Reference Mellander, Berntsson and Nilsson20 As a consequence of these adverse effects on patients and their parents and siblings, it is clear that one area that has possibly not received as much attention as is perhaps necessary is advice on strategies of parenting for parents of children with surgically palliated hypoplastic left heart syndrome. One study has found that “extraordinary parenting in a context of uncertainty” was evident in their interviews with parents and that promotion of better parenting strategies is also an important aspect of counselling and care for these families.Reference Rempel and Harrison21
Antenatal diagnosis and termination of pregnancy
Mahle et alReference Mahle, Clancy, McGaurn, Goin and Clark22 have examined the impact of antenatal diagnosis on survival and early neurological morbidity after Norwood palliation and found that antenatal diagnosis had no significant impact on survival; however, on multivariable analysis, fewer adverse peri-operative neurological events occurred in those in whom an antenatal diagnosis had been made. In contrast, one study from the United States of America has reported that antenatal detection of hypoplastic left heart syndrome does lead to reduced peri-operative mortality after the Norwood (Stage I) operation; indeed, those with an antenatal diagnosis not only had an improved early survival, but had lower early rates of acidosis, ventricular dysfunction, and tricuspid regurgitation.Reference Tworetzky, McElhinney, Reddy, Brook, Hanley and Silverman23 One potential confounding factor, however, is that those foetuses with more severe congenital abnormalities and those foetuses with other associated extracardiac abnormalities are more likely to be detected antenatally.Reference McBrien, Sands, Craig, Dornan and Casey24
The recent Single Ventricle Reconstruction trial in the United States has examined rates of antenatal diagnosis and risk factors for the Norwood (Stage I) operation. It was found that rates of antenatal detection vary widely across centres from 59% to 89%, although the presence or absence of an antenatal diagnosis did not appear to influence peri-operative mortality, whereas the presence of major extracardiac congenital abnormalities did.Reference Atz, Travison and Williams25 Although antenatal diagnosis for hypoplastic left heart syndrome does seem to be reliable, others have also reported that antenatal diagnosis does not appear to influence early outcome.Reference Galindo, Nieto, Villagra, Graneras, Herraiz and Mendoza26
European data, in concordance with reports from the United States, show that the overall mortality for surgical palliation of hypoplastic left heart syndrome is decreasing (Fig 2).Reference Karamlou, Diggs, Ungerleider and Welke10 One centre from the United Kingdom has reported a concomitant marked decrease in the rate of termination of pregnancy for hypoplastic left heart syndrome from 43.7% to 25.3%, comparing a recent cohort with one from 5 years previously.Reference Rasiah, Ewer and Miller27 The EUROSCAN group have examined the rates of antenatal detection for congenital cardiac disease across 20 European centres and found a wide variation in rates of diagnosis, with Eastern European centres having a rate as low as 8%; rates in Western European centres varied from 19% to 48%. The mean rate for hypoplastic left heart syndrome was 45%, with a rate of termination of pregnancy of 23%.Reference Garne, Stoll and Clementi28 More recently, the same group have examined rates of termination of pregnancy for foetal anomalies in general performed less than 24 weeks and also found a wide variation in rates of termination of pregnancy across Europe, with France reporting the highest rate of almost 7 per 1000, and the Netherlands reporting the lowest rates of 1–1.5 per 1000 births.Reference Garne, Khoshnood, Loane, Boyd and Dolk29 In one study from Melbourne, Australia, parents were counselled jointly by an ultrasonographer and paediatric cardiologist for the diagnosis of serious cardiac disease, and over 3 years of the study 13 out of 40 opted for termination of pregnancy. Importantly, counselling focussed on the functional outcomes, need for further interventions, and quality of life. The parents, however, reported that the most important factor in choosing termination of pregnancy was the perceived anticipated distress to the affected child and effects on parents and siblings.Reference Menahem and Grimwade30
Attitudes of surgeons, counselling, and factors affecting choice
Potential determinants of the decision-making process of the parents include the medical personnel who counsel them, as well as the perceived estimates of the surgeon of outcome. Outcome in this context may in turn be defined to include early survival, late survival, and quality of life. Quality of life includes
• morbidity related to the procedure/need for further surgery or interventions;
• potential for somatic growth;
• functional outcome including neurodevelopment and exercise capacity; and
• psychosocial impact on the patient and family.
In colouring these estimates, the attitudes of surgeons are influenced potentially by multiple factors:
• whether they are parents themselves,
• their perception of success of surgical palliation at their own institution, and
• possibly what their hypothetical choice of treatment would be for their own child if a diagnosis of hypoplastic left heart syndrome was made.
Other potential important factors not directly ascertained in this study that have been highlighted by others include race and/or ethnicity, religious denomination, years in medical practice, and medical speciality.Reference Kon, Ackerson and Lo2, Reference Prsa, Holly, Carnevale, Justino and Rohlicek31
Overall, in this study, two-third of respondents reported that attitudes to the management of hypoplastic left heart syndrome had changed in their country, just over half reporting that attitudes had changed for their individual centre. One study has found that increasing numbers of parents are choosing surgical palliation and that this choice appears to be partly attributable to better counselling, familial support groups, and improving surgical outcomes for patients with hypoplastic left heart syndrome.Reference Corrow, Lapuk, Mazzarella, Sable, Leopold and Eisenfeld32 Others have made similar observations, with an increase in the number of parents choosing either Norwood palliation or primary transplantation as opposed to comfort care.Reference Osiovich, Phillipos, Byrne and Robertson33 Importantly, in their study, Prsa et alReference Prsa, Holly, Carnevale, Justino and Rohlicek31 reported that only 36.5% of cardiologists and surgeons surveyed across North America counselled parents by presenting all possible options for management.
In a survey of paediatric residents and nurses, Renella et alReference Renella, Chang, Ferry, Bart and Sklansky34 found that the volume of the centre was an important factor that influences whether those surveyed would opt for surgery. Perceived estimates of survival and quality of life also appeared important in this regard. Greater experience predicted termination of pregnancy in this study, although this did not emerge as an important factor in the study by Prsa et al. In another survey of mothers of children with hypoplastic left heart syndrome, more years in education also emerged as being associated with choosing comfort care over surgery; the main reason for choosing this option was to prevent the child from suffering.Reference Vandvik and Forde35 The team of counsellors involved is likely therefore to play a key role in how parents respond. A multi-disciplinary team will be more balanced with regard to advice given; certainly, in the centres surveyed here, the majority would employ teams for counselling comprising different specialities for the either antenatal or postnatal diagnosis of hypoplastic left heart syndrome, as shown in Table 3.
Study limitations
This survey included only 14 centres, that is, 12 European and 2 non-European. Meanwhile, the European Association for Cardio-Thoracic Surgery Congenital Heart Surgery Database includes 140 active Centres from 37 countries submitting data. Thus, this survey represents a limited number of European centres.
Many of the data reported in this manuscript are estimates of survival, rather than actual survival; therefore, these reported estimates may not be precise and are not verified or validated data.
The main measure of outcome in this study was the estimate made by the surgeon of parental choice at their institution. As such, this measure of outcome is only a perceived estimate and may not accurately reflect the data for the centre. A similar case may be argued for the estimates of volume at the centre as one of the factors colouring the way in which surgeons counsel parents and how parents respond to this information. The response rate of less than 50% may be an important source of bias in the results. One aspect that was not examined in our study was the recommendations that surgeons made to parents and how this correlated with the actual choices made by the parents. This information would be of interest in providing a more complete picture of the parental process of making decisions and how recommendations relate to the decisions made. More detailed data concerning the geographical variation in antenatal rates of detection and rates of termination at different centres would also be important in helping to outline the landscape upon which parental decisions rest.
Implications/conclusions
In our previous report, we highlighted the differences in the European and North American attitudes to management of patients with hypoplastic left heart syndrome and reported that quality of life was more important in Europe, whereas in the United States of America life at any cost was seen as the primary objective.Reference Elliott1 Significant costs are associated with staged surgical palliation, with the highest costs being associated with Stage I reconstruction. One study from the United States of America estimated the cost per patient for Stage I treatment as being greater than $50,000 (United States of America dollars).Reference Williams, Gelijns and Moskowitz36 Regarding the total burden of disease, according to World Health Organisation estimates, 40% of deaths in children worldwide occur in the neonatal period, with most of these being due to prematurity, asphyxia, and sepsis, with congenital cardiac disease accounting for only 3% of the 41% total neonatal deaths.37 Although surgical palliation of hypoplastic left heart syndrome likely represents less than 5% of the volume of cases for even high-volume centres, the activity for staged palliation of patients with hypoplastic left heart syndrome appears to be increasing. Despite this increase in activity, the long-term outcomes in terms of survival and quality of life for patients with Fontan circulations for surgically palliated hypoplastic left heart syndrome are still uncertain. Living with this uncertainty, which persists even from the time of diagnosis, is a particularly difficult emotional state to live with for families of those with hypoplastic left heart syndrome. Improving survival following surgical palliation for hypoplastic left heart syndrome, with decreasing morbidity and better functional status and quality of life for patients and their families, as well as changing attitudes to these more favourable results and how best to counsel parents of affected children will, it is hoped, lead to better-informed parental choices and lives for patients with hypoplastic left heart syndrome. It is also clear from this report that massive inconsistency exists in the information given to parents and families, and this inconsistency cannot be appropriate. We must present the truth to them to allow these very complex and life challenging decisions to be fairly made. We argue that surveys such as this one should be performed regularly, over a larger scale, and with greater rigour. They would provide a basis for auditing the accuracy and appropriateness of the information given to families affected by complex congenital conditions.
Acknowledgements
We are grateful for to all the following Paediatric Cardiac Surgeons at the centres included in this study for their participation in the survey: Pascal Vouhe (Paris, France); Bohdan Maruszewski (Warsaw, Poland); David Anderson (London, UK); Zohair Al Halees (Riyadh, Saudia Arabia); Harald Lindberg (Oslo, Norway); Victor Hraska (St Augustin, Germany); Christian Brizard (Melbourne, Australia); Mark Hazekamp (Leuven, Belgium); Reza Hosseinpour (Seville, Spain); Yves D'udekem (Melbourne, Australia); Vibeke Hjortkal (Aarhus, Denmark); Giles Peek (Leicester, UK); Tomas Tlaskal (Prague, Czech Republic); Heikki Sairenen (Helsinki, Finland); Bart Meyns (Leuven, Belgium); Christo Tchervenkov (Montreal, Canada).









