Focal atrial tachycardia is a rare cause of supraventricular tachycardia in children, originating from automatic, rapidly firing, non-sinus foci within the atrium. Reference Case and Gillette1,Reference Rosso and Kistler2 Although this tachycardia is benign in most instances, it could lead to tachycardia-induced cardiomyopathy in incessant cases, albeit it is generally reversible with the control of the arrhythmia. Reference Chiladakis, Vassilikos, Maounis, Cokkinos and Manolis3,Reference Medi, Kalman and Haqqani4 Younger children generally respond to antiarrhythmic therapy and present a higher incidence of focal atrial tachycardia resolution; hence, pharmacological therapy is the recommended first-line treatment for focal atrial tachycardia in infants. Reference Brugada, Blom and Sarquella-Brugada5 In children ≥3 years, focal atrial tachycardia is unlikely to resolve spontaneously, and antiarrhythmic medications are usually ineffective. Reference Salerno, Kertesz, Friedman and Fenrich6 Hence, catheter ablation should be considered early, especially in older children with recurrent symptoms, incessant tachycardia, or tachycardia-induced cardiomyopathy that is refractory or intolerant to medical treatment. Reference Brugada, Blom and Sarquella-Brugada5,Reference Salerno, Kertesz, Friedman and Fenrich6 Three-dimensional electroanatomical mapping system provides more precise localisation of ectopic foci and successful catheter ablation with limited fluoroscopy. Reference Campbell, Strieper and Frias7,Reference Kottkamp, Hindricks, Breithardt and Borggrefe8 Although several studies reported that this system can significantly decrease or even eliminate fluoroscopy exposure during catheter ablation of the supraventricular tachycardia substrates, Reference Steinbeck and Hoffmann9,Reference Toyohara, Fukuhara, Yoshimoto, Ozaki and Nakamura10 there is limited data regarding its use in focal atrial tachycardia ablation in children. Reference Dieks, Muller and Schneider11–Reference Elkiran, Akdeniz, Karacan and Tuzcu14
This study summarises the authors’ experience with catheter ablation in focal atrial tachycardia that was performed using a three-dimensional surface electrode-based navigation system (EnSite™ Precision, St Jude/Abbott Medical, St Paul, MN, United States of America) for guidance with limited fluoroscopy in children. This is the largest paediatric series from a single centre evaluating the efficacy and safety of catheter ablation and limited fluoroscopy in focal atrial tachycardia.
Patients and methods
This study included 60 patients (18 females and 42 males) who were diagnosed with focal atrial tachycardia, and underwent electrophysiological study and catheter ablation procedure between February, 2014 and February, 2020. Data regarding clinical characteristics, echocardiographic examination, ablation procedures, and follow-up were obtained from hospital records using the Filemaker database. This retrospective cohort study was approved by the Institutional Review Board, and informed consent was obtained from all patients.
Electrophysiological study and catheter ablation
All patients and/or their legal guardians consented to the procedure. Antiarrhythmic medications were discontinued for at least five half-lives before the electrophysiological studies. Three-dimensional surface electrode-based navigation system was used in all patients.
Depending on the patient’s age, an electrophysiological study was performed either under local anaesthesia with mild sedation or under general anaesthesia without intubation. For left-sided foci, access to the left atrium was achieved via the patent foramen ovale or transseptal puncture. The procedure was started without fluoroscopy, and catheters were placed into the right atrium, coronary sinus, and right ventricle under the EnSite™ Precision system’s guidance. Three-dimensional images of the anatomy of the superior and inferior vena cava, right atrium, coronary sinus, and right ventricle were obtained.
Electroanatomic mapping was performed with multi-polar catheters (decapolar or duodecapolar) during tachycardia and recording local electrogram findings from the atria. Activation mapping was performed by comparing “local activation time values” with a fixed atrial “A” value. Usually, the atrial signal at the proximal electrode of the coronary sinus catheter; more rarely, the atrial signal at the distal end of the transesophageal electrode was considered as “A” reference. The location of atrial focus was assessed by the prematurity of local atrial activation compared to the stable “A” reference. Colour-coded electroanatomical mapping was also helpful in coding the potential target sites in 3D geometry. On the colour scale, early activation was colour coded in white with the latest activation points coded in purple. During tachycardia, the window of interest was determined to reveal whether the tachycardia was macroreentrant or focal/microreentrant. In focal/microreentrant tachycardia, it was assumed that there was radial propagation from a small focus. Amongst the earliest signals, the points at which propagation began were considered as the foci, and fractionated electrograms were simultaneously searched. In addition, a pure negative deflection (QS pattern) of unipolar atrial electrogram was determined. Finally, voltage mapping was performed during sinus rhythm or atrial pacing, if appropriate, to identify endocardial scars or fibrosis, which were defined as areas with endocardial signals <0.1 Mv.
If an adequate spontaneous atrial activity was not present at the beginning of the procedure, standard atrial and ventricular pacing manoeuvres were conducted and orciprenaline bolus was administered to stimulate atrial ectopy when necessary.
Radiofrequency energy application was used in majority of the patients. A steerable radiofrequency catheter was used for mapping and energy delivery. Irrigated radiofrequency was used when standard radiofrequency failed or in cases with focal atrial tachycardia scar-related lesion. Fixed curve or steerable long sheaths were used in right atrial foci where catheter stabilisation was difficult during radiofrequency.
Cryoablation was performed using 7 F 6-mm-tip or 9 F 8-mm-tip catheters (Medtronic, Minneapolis, MN, United States of America) in patients with foci close to the atrioventricular node and phrenic nerve.
All data regarding ablation procedures, numbers of lesions, extra arrhythmia substrates, and complications were recorded. After successful ablation, patients were observed for a 30-minutes waiting period. The possibility of recurrence was assessed using pacing manoeuvres, and with orciprenaline or adenosine in some cases. When additional tachycardia mechanisms were deemed to have potential clinical relevance, mapping and ablation procedures were repeated.
Follow-up
As per standard practice, all patients underwent continuous telemetry monitoring, 12-lead electrocardiogram, 24-hour ambulatory electrocardiogram, and echocardiography before discharge. All patients were hospitalised following the ablation procedure as required by standard practice. They were examined at the outpatient clinic for symptoms suggestive of arrhythmia after 1, 3, and 6 months of the procedure and then every 12 months. At each visit, a 12-lead electrocardiogram, and if necessary, a 24-hour ambulatory electrocardiogram monitoring were performed. Recurrence was defined as the relapse of clinical symptoms consistent with episodes before the ablation, as well as documented focal atrial tachycardia with an electrocardiogram, a 24-hour ambulatory electrocardiogram, or an event recorder.
Statistical analysis
Statistical Package for the Social Sciences version 21.0 was used to analyse the data. Descriptive features were represented as percentages and mean ± standard deviation or as median according to the distribution of the data determined by the Kolmogorov–Smirnov test. The data were compared using χ2 or Fisher’s exact tests and independent t-test or Mann–Whitney U-test depending on the distribution of the data. P-values <0.05 were considered statistically significant.
Results
General observations
All demographic and clinical characteristics of the included patients are listed in Table 1. During the study period, 60 patients underwent electrophysiological study for symptomatic focal atrial tachycardia. The median age of the patients (42 males and 18 females) was 12.01 years (16 days–18 years). Seven (11.6%) patients were aged <1 year, and two of them were newborns during the procedure. The children aged <1 year in this study had tachycardia complicated by drug resistance, drug intolerance, or tachycardia-induced cardiomyopathy, despite treatment with two or more antiarrhythmic drugs. The median weight of the patients was 41.5 kg (3–98 kg). CHD was present in 12 of (20%) patients, while focal atrial tachycardia with tachycardia-induced cardiomyopathy was found in 15 (25%). The mean ejection fraction in these patients was 39% (20–45). Before undergoing electrophysiological study, 8 patients (13.3%) were not under any regular antiarrhythmic medication, 23 (38.3%) were regularly taking 1 antiarrhythmic drug (beta blocker or class 1c antiarrhythmic), 17 (28.3%) were taking 2 different antiarrhythmic drugs (beta blocker + class 1c/class 3 antiarrhythmic [amiodarone/sotalol]), and 12 (20%) were taking 3 different antiarrhythmic drugs (beta blocker + class 1c + class 3 antiarrhythmic [amiodarone/sotalol]). Of the 60 patients, 5 (8.3%) had undergone previous electrophysiological study at different institutions. Furthermore, 13 (21.7%) patients had other coexisting tachycardia conditions in addition to the focal atrial tachycardia, including typical atrioventricular nodal re-entrant tachycardia (n = 6), intra-atrial re-entrant tachycardia (n = 2), atrial flutter (n = 1), junctional ectopic tachycardia (n = 2), frequent premature ventricular contraction (n = 1), and Wolf–Parkinson–White syndrome (n = 1). All 13 patients underwent concurrent ablation for the other tachycardia conditions.
Table 1. Demographic and clinical characteristics of patients.

n (%)
and shortening fraction <28 or ejection fraction <50 and left ventricular end diastolic diameter z-score >2.
Number and localisation of focal atrial tachycardia foci
The anatomic localisation of the focal atrial tachycardia foci in this study is depicted in Fig 1. Amongst the 60 patients, 4 had 2 foci (60 patients, 64 arrhythmia foci). During the procedure, it was found that 45 of the focal atrial tachycardia foci were right-sided and 18 were left-sided. One case presented focal atrial tachycardia foci in both atria. Right-sided foci were located in clusters around the coronary sinus ostium (n = 11, 24.4%), along the crista terminalis (n = 10, 22.2%), tricuspit annulus (n = 9, 20%), and in or close to the right atrial appendage (n = 7, 15.5%). Left-sided foci were mainly found around the mitral annulus (n = 11, 57.8%) and pulmonary vein orifices (n = 5, 26.3%).
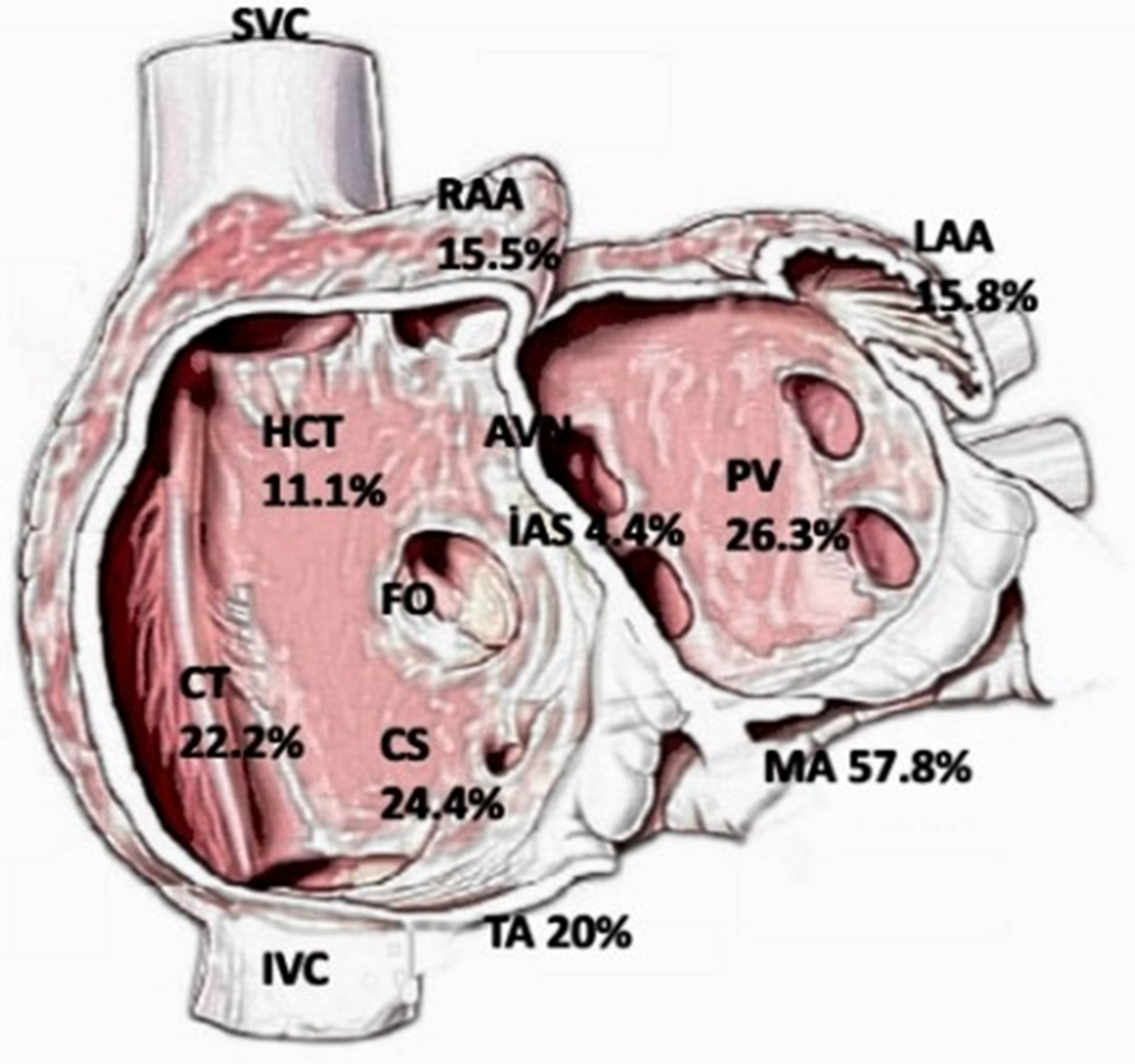
Figure 1. Anatomic location: a schematic representation of atrial ectopic foci distribution in the study population. AVN = atrioventricular node; CS = coronary sinüs; CT = crista terminalis; FO = fossa ovalis; HCT = high crista terminalis; IAS = interatrial septum; IVC = inferior vena cava; LAA = left atrial appendage; MA = mitral annulus; PVs = pulmonary veins; RAA = right atrial appendage; SVC = superior vena cava; TA = tricuspid annulus.
Procedure characteristics
Procedural characteristics of the patients included in this study are listed in Table 2. After the electrophysiological study, radiofrequency ablation was performed in 47 patients (irrigated radiofrequency was performed simultaneously in 7 cases that did not respond favourably with radiofrequency, or when deep ablation lesion was required, or focal atrial tachycardia developed due to scar-related lesion), cryoablation was performed in 9 patients, and both radiofrequency and cryoablation were performed in 4 patients. The median procedural time was 163.5 minutes (82–473 minutes), including a 30-minute waiting period.
Table 2. Procedural characteristics and results of ablation.

Median (range) and n (%)
* 1> ectopic focus; right-sided n = 3 and left-sided n = 1
** mean
Limited fluoroscopy exposure
Fluoroscopy is not often used unless transseptal puncture is needed, and especially in children weighing <10 kg or those with complex CHD whose catheter position needs to be confirmed. Fixed curve or steerable long sheaths were used in right atrial foci where catheter stabilisation was difficult. Additionally, limited fluoroscopy was used in these cases.
All electrophysiological procedures in this study were performed using the EnSite™ Precision system.
Fluoroscopy was used in 29 of the 60 patients (48.3%). The mean fluoroscopy time was 8.64 ± 6.2 minutes, and median fluoroscopy dosage was 1.4 mGy (0.35–6.67 mGy). Of the 29 patients undergoing fluoroscopy, 15 had left-sided and 1 had bilateral atrial tachycardia. Transseptal puncture was performed in 16 patients (Fig 2a–e). Before attempting the transseptal puncture, the presence of patent foramen ovale was investigated using the previously generated three-dimensional model as a reference. If it was present, the left atrium was accessed through the foramen ovale. Mean fluoroscopy time during transseptal puncture was 3.67 ± 1.7 minutes. In the other patients <1 year of age or those with complex CHDs, fluoroscopy was used for catheter position determination. The mean fluoroscopy time was 9.14 ± 8.1 minutes in those with left-origin focal atrial tachycardia, and 8.1 ± 3.59 minutes in those with right-origin focal atrial tachycardia (p = 0.672). Comparative data between patients with left or right-side-originated foci of focal atrial tachycardia are presented in Table 3.

Figure 2. (a) During FAT, atrial p-waves appear on the ground with the AV block effect of IV adenosine. (b) During the electrophysiological study, the a-waves appear distally in the distal front of the diagnostic coronary sinus (CS) catheter (eccentric pattern; from the left). (c) Fluoroscopy image taken during the patient’s EPS ablation procedure (cardiomegaly due to tachycardia-induced cardiomyopathy is remarkable). (d) During EPS ablation, centrifugal propagation of the focal atrial tachycardia originating from left atrial appendage–left anterolateral annulus junction in 3D electroanatomic mapping with EnSite Precision (St Jude Medical Inc.) (e) Two-years after successful ablation, cardiomegaly completely improved in the patient’s telecardiography.
Table 3. Comparative data between patients with left or right-side-originated foci of focal atrial tachycardia**.

Median (range) and n (%)
* mean
** The patient with focal atrial tachycardia foci in both atria is not included in the table.
Success, complications, and follow-up
Acute success was achieved in 57 out of the 60 patients (95%). Successful ablation could not be achieved in three patients, of which right-sided focal atrial tachycardia was seen in two patients (one at the crista terminalis and one at the high crista terminalis) and left-sided in one (mitral annulus).
During a median follow-up of 17 months (2–69 months), two patients (3.5%) experienced recurrence, and both recurrences occurred within the first 6 months after ablation. The location of focal atrial tachycardia in these two patients was at the right appendage in one and at the orifice of the pulmonary vein in the other. Medical therapy was administered in one of these two patients (beta blocker and propafenone) because his symptoms could be controlled by medical treatment. Ablation was performed for the second time in one patient with recurrence and three patients in whom the procedure had previously failed, and three of these cases reported success. In one patient, radiofrequency ablation was unsuccessful because the tachycardia focus was located epicardially in the right atrium. The final success rate was 96.6%. Minimal pericardial effusion was observed in one patient, which did not require intervention. No other major complications were seen. Significant improvement in the left ventricular function was observed after successful ablation in patients who developed tachycardia-induced cardiomyopathy. The follow-up revealed that all patients showed normal left ventricular function in 6 months.
Discussion
This is the largest paediatric study evaluating the efficacy and safety of catheter ablation using three-dimensional electroanatomical mapping in children with focal atrial tachycardia from a single centre. The most noteworthy findings were as follows:
-
Catheter ablation of focal atrial tachycardia in children, including infants, can be performed safely and effectively with limited fluoroscopy using three-dimensional electroanatomical mapping systems.
-
A significant number of patients with tachycardia-induced cardiomyopathy showed normalised cardiac functions after successful focal atrial tachycardia ablation.
-
Irrigated type radiofrequency ablation catheters can be safely used in children when deeper and larger ablation lesions are needed in the atrial tissue.
Focal atrial tachycardia is a rare cause of supraventricular tachycardia in children, which accounts for 5–10% of supraventricular tachycardia cases in adults, with higher rates seen in children. Reference Rosso and Kistler2 Medical therapy has been the primary treatment for focal atrial tachycardia, especially in young children who are more likely to have spontaneous resolution. Reference Salerno, Kertesz, Friedman and Fenrich6,Reference Balla, Foresti and Ali15,Reference Bauersfeld, Gow, Hamilton and Izukawa16 In children aged ≥3 years, focal atrial tachycardia is unlikely to resolve spontaneously, and antiarrhythmic medications are usually ineffective. Reference Salerno, Kertesz, Friedman and Fenrich6 Therefore, catheter ablation of focal atrial tachycardia is considered as the first-line therapy in patients with recurrent symptoms, conditions refractory to medical treatment, or incessant tachycardia or tachycardia-induced cardiomyopathy. Reference Roberts-Thomson, Kistler and Kalman17,Reference Walsh, Saul and Hulse18
There is limited data regarding the use of catheter ablation for focal atrial tachycardia in younger children. Initial studies of radiofrequency ablation in young or small children suggested that there might be a lower success and higher complication rates. However, subsequent literature showed better outcomes of the procedure when performed with electroanatomical mapping as compared to the conventional strategy in terms of acute success rate and recurrences. Reference Cummings, Mahle and Strieper12,Reference Kang, Etheridge and Kantoch13 Toyohara et al reported acute success in all of their paediatric focal atrial tachycardia patients (35/35) and 11% recurrence in patients undergoing radiofrequency ablation using the three-dimensional mapping system. Reference Toyohara, Fukuhara, Yoshimoto, Ozaki and Nakamura10 Dieks et al reported acute success in 14 of the 16 patients (87.5%) using modern mapping systems. Reference Dieks, Muller and Schneider11 Elkıran et al reported acute success in 34 of the 39 patients (87.2%). Reference Elkiran, Akdeniz, Karacan and Tuzcu14 In this study, acute success was achieved in 57 of the 60 patients (95%). During a median follow-up of 17 months (2–69 months), focal atrial tachycardia recurred in two patients (3.5%). Ablation was performed for the second time in one patient with recurrence and three patients in whom the procedure had previously failed. Of these cases undergoing the repeat procedure, three cases were successful. In one patient, radiofrequency ablation was unsuccessful because the tachycardia focus was located epicardially in the right atrium. The final success rate was 96.6%.
Although a 4 mm tip radiofrequency ablation catheter is adequate to ablate the arrhythmia focus located near the endocardium, it does not readily ablate the deeper tachyarrhythmia substrate. With 8- and 10 mm tip radiofrequency ablation electrodes, the ablation lesions are larger, but these catheters are associated with increased risk of coagulum, char, and thrombus formation, as well as myocardial steam rupture. Irrigated radiofrequency ablation tips prevent excessive temperatures at the electrode tip–tissue interface, and thus allow continued delivery of the radiofrequency current into the surrounding tissue. This ablation system creates larger and deeper ablation lesions and minimises steam pops and thrombus formation. Reference Houmsse and Daoud19 In this study, irrigated radiofrequency ablation was used in seven cases that did not get sufficient current with standard radiofrequency ablation. There were no complications observed in the procedures where irrigated radiofrequency ablation was used. Highly acute and long-term success rates reported in this study could be associated with the use of irrigated radiofrequency ablation. Hence, irrigated tip catheters should be considered as adjunct tools when needed. Triedman et al pointed out that the extent of lesion depth limits the clinical success of ablation outcomes, and the use of irrigated ablation may result in improved rates of acute success with ablation. Reference Triedman, DeLucca, Alexander, Berul, Cecchin and Walsh20
It is well recognised that focal atrial tachycardia foci do not occur randomly throughout the atria, but tend to cluster at characteristic anatomic locations. Reference Kistler, Roberts-Thomson and Haqqani21 As described by Lee et al, Reference Lee, Sanders and Kalman22 the most common site of focal atrial tachycardia foci in adult patients is the right atrium (75%), with the most common origin areas being the superior and middle parts of the crista terminalis. In the left atrium, foci are most often noted at the ostium of the pulmonary veins. Reference Lee, Sanders and Kalman22 Additionally, ectopic foci were found predominantly in the right atrium in the present study, mostly as clusters around the coronary sinus ostium along the crista terminalis and tricuspid annulus. Left-sided foci were mainly found around the mitral annulus and pulmonary vein orifices. These findings corroborated with the data from the previous studies. Reference Salerno, Kertesz, Friedman and Fenrich6,Reference Dieks, Muller and Schneider11 The location of focal atrial tachycardia foci clusters differs between paediatric and adult patients. Lee et al reported that foci around the atrial appendage were rare in adult patients (0.6%). Reference Lee, Sanders and Kalman22 Toyohara et al demonstrated that in children aged <7 years, ectopic foci were mostly localised in the left and right appendages, because of the presence of residual embryonic tissue. Reference Toyohara, Fukuhara, Yoshimoto, Ozaki and Nakamura10 In this study, the percentage of foci around the right and atrial appendages were 15.5 and 15.8%, respectively. Toyohara et al also demonstrated that patients with crista terminalis-related focal atrial tachycardia were aged >7 years, suggesting that the substrate of focal atrial tachycardia originating in the crista terminalis might be acquired with age. Reference Toyohara, Fukuhara, Yoshimoto, Ozaki and Nakamura10 In this study, the mean age of the patients with crista terminalis-related focal atrial tachycardia was 12.4 years.
A longer procedural time duration was observed in the left-sided focal atrial tachycardia ablations as compared to the right-sided ones in the present study. However, existing literature shows that the total procedural time duration in this study was shorter than that of other studies (median procedural time = 163.5 minutes [82–473 minutes]). Reference Dieks, Muller and Schneider11,Reference Cummings, Mahle and Strieper12 The procedural time in the left-sided cases was slightly longer because of the time needed to catheterise the left atrium either through a patent foramen ovale or through a transseptal puncture in case of the absence of a patent foramen ovale. Although the procedural time was longer in those with left-sided focal atrial tachycardia foci, no significant difference between the fluoroscopy time was observed (p = 0.672).
Systolic dysfunction associated with chronic tachyarrhythmia is known as tachycardia-induced cardiomyopathy. Reference Medi, Kalman and Haqqani4,Reference De Giovanni, Dindar and Griffith23 Of the 60 patients in this study, 15 (25%) presented with decreased ventricular function and tachycardia-induced myopathy, an incidence rate similar to that reported in the literature. Reference Toyohara, Fukuhara, Yoshimoto, Ozaki and Nakamura10,Reference Cummings, Mahle and Strieper12 At the same time, these findings did not show a significant difference in the development of tachycardia-induced myopathy between the right- and left-sided focal atrial tachycardia cases (p = 0.355). Children with focal atrial tachycardia are less likely to be aware of palpitations and tachycardia episodes. Reference Toyohara, Fukuhara, Yoshimoto, Ozaki and Nakamura10 Hence, the complication of focal atrial tachycardia with tachycardia-induced myopathy was more commonly observed in children than in adults. Medi et al reported a 10% incidence of tachycardia-induced myopathy with focal atrial tachycardia in adults. Reference Medi, Kalman and Haqqani4 In this study, 6 (40%) of the patients who developed tachycardia-induced myopathy were aged <1 year. The left ventricular function returned to normal or near-normal in all patients with tachycardia-induced myopathy during the follow-up. Medi et al reported that patients with rapid focal atrial tachycardia could, therefore, be recognised earlier and given quick treatment, leaving less time for tachycardia-induced myopathy to develop. In contrast, patients with slower incessant tachycardia may not present palpitations early on, but rather later with symptoms of cardiac failure. Reference Medi, Kalman and Haqqani4
Children undergoing conventional radiofrequency ablation are believed to be at increased risk of developing malignancy caused by radiation exposure. Reference Clay, Campbell, Strieper, Frias, Stevens and Mahle24 The increased lifetime risk of fatal malignancy was 0.02% with each radiofrequency ablation procedure. Reference Clay, Campbell, Strieper, Frias, Stevens and Mahle24 Thus, non-fluoroscopic or limited fluoroscopy electroanatomical mapping systems have become a focus of current research. In the present study, the mean fluoroscopy times (mean 8.64 ± 6.2 minutes) was significantly reduced with the routine use of modern three-dimensional mapping systems compared to previous studies. Reference Dieks, Muller and Schneider11,Reference Cummings, Mahle and Strieper12 Cummings et al compared two-dimensional and three-dimensional mapping and found no significant differences in the fluoroscopy times (47 ± 24 versus 40 ± 20 minutes). Dieks et al reported that their median fluoroscopy time was 13.1 minutes (4.5–22.5 minutes) for focal atrial tachycardia ablation with three-dimensional mapping systems in children. In one of the largest studies on the current management of paediatric focal atrial tachycardia, 134 patients (54%) underwent 167 catheter ablation procedures, with median fluoroscopy time of 23 minutes (95% confidence interval, 20–30). Reference Kang, Etheridge and Kantoch13 Fluoroscopy was performed in 29 of our patients for transseptal puncture or catheter position detection, especially in young children weighing <10 kg. The mean fluoroscopy time during transseptal puncture in this study was 3.67 ± 1.7 minutes. Although the procedural time in this study was longer in left-sided ablations, no significant difference between the left and right fluoroscopy times was found (p = 0.672).
Depending on the age, major complications have been reported during focal atrial tachycardia ablation in 3–8% of the cases. Reference Kugler, Danford, Houston and Felix25 Reported complications include 2° and/or 3° atrioventricular block, perforation, pericardial effusion, thrombus formation, damage to phrenic nerve, stroke, and cardiac arrest. In this study, minimal pericardial effusion was observed in one patient, which did not require intervention. No other major complications were seen.
Catheter ablation can be performed effectively and safely in paediatric focal atrial tachycardia patients, including infants, using a limited fluoroscopic approach with the help of an electroanatomical mapping system. Irrigated radiofrequency ablation should be considered as an alternate method in deep lesions or scar-related lesions, where sufficient current cannot be provided with standard radiofrequency ablation.
Acknowledgements
None.
Financial support
The authors received no financial support for the research and/or authorship of this article.
Conflicts of interest
All authors declare that they have no conflict of interest.
Ethical standards
The authors assert that all procedures contributing to this work comply with the ethical standards of the institutional research committee (Approval number: 2020/34) and with the Helsinki declaration of 1975, as revised in 2008, and has been approved by the institutional committees.








