The reported incidence of cardiac tumours is 0.027–0.08% in paediatric autopsiesReference Tzani, Doulamis, Mylonas, Avgerinos and Nasioudis1 and 0.08–0.2% in the foetuses.Reference Carrilho, Tonni and Araujo2 The growing incidence reported over the last decades reflects, most likely, improvements in imaging diagnostic methods.Reference Yadava3 More than 90% are benign, and rhabdomyomas, fibromas, and teratomas are responsible for the majority of this age group.Reference Sánchez Andrés, Insa Albert, Carrasco Moreno, Cano Sánchez, Moya Bonora and Sáez Palacios4 Malignant tumours are even rarer, and metastases are 100-fold more common than primary lesions.Reference Castillo and Silvay5 Tumours can be found in myocardium with extending to cardiac chambers, or within the pericardial sac with or without invasion of the great vessels. The clinical presentation is varied, ranging from asymptomatic and accidental imaging diagnosis to sudden death. Symptoms may be constitutional, due to distal embolisation or due to its direct effect.Reference Poterucha, Kochav, O’Connor and Rosner6 The latter can be due to obstruction of the cardiac valves or outflow tracts, invasion of the conduction system with arrhythmias, and cardiac tamponade. The definitive diagnosis is only possible following histological analysis. In the exceptional cases of strongly suspected malignancy, an elective biopsy can be done. However, in the majority of patients the differential diagnosis relies on both echocardiography and cardiac MRI aspects. Treatment is advocated in those who have symptoms, cardiac dysfunction, or in those at greater risk of distal embolisation.Reference Uzun, Wilson, Vujanic, Parsons and De Giovanni7 Total surgical resection is the treatment choice, not always possible in large or invasive tumours, due to the risk of structurally damaging the heart. In these cases, partial resection is advocated to control the symptoms and preserve the cardiac function.Reference Günther, Schreiber, Noebauer, Eicken and Lange8 Cardiac transplant is reserved for unresectable tumours or multiple recurrences.Reference Kewcharoen, Prasongdee and Sinphurmsukskul9
We present our single-centre experience in cardiac tumours in paediatric age, as well as a literature review. A summary of the main characteristics of the cardiac tumours and diagnosis features is presented in Table 1.
Table 1. Characteristics of paediatric cardiac tumours.
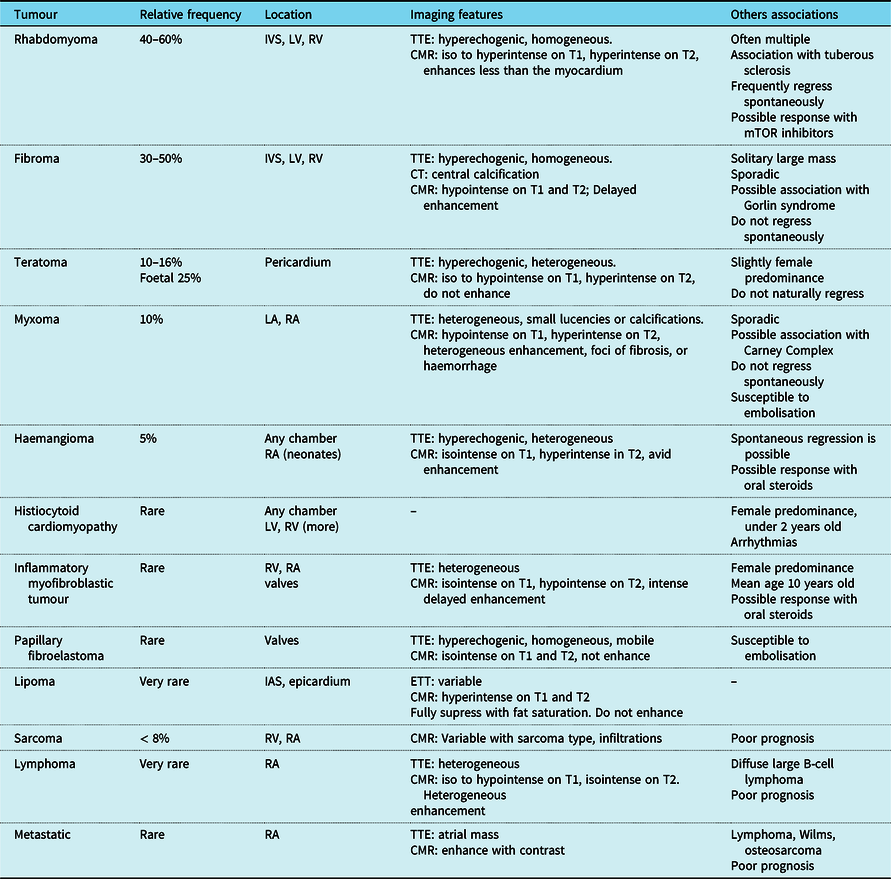
CMR = cardiac magnetic resonance; IAS = interventricular septum; IVS = interventricular septum; LA = left atrium; LV = left ventricle; mTOR = mammalian target of rapamycin; RA = right atrium; RV = right ventricle; TTE = transthoracic echocardiography
Single-centre experience
As a referral centre for CHDs and paediatric cardiology, we are one of four centres in Portugal that manage and follow children with cardiac tumours. We reviewed the patients with cardiac tumours in the last 16 years, from January 2005 to December 2020 (Table 2). In 16 years, our centre followed 17 born patients, 11 with rhabdomyomas, 3 with fibromas, 2 with myxomas, and a pericardial teratoma. Rhabdomyomas were the most common tumours and 45% presented in the context of tuberous sclerosis, a relatively low incidence compared to that described in the literature.Reference Paramés, Freitas and Martins10,Reference Mariano, Pita and León11 One patient with cardiac rhabdomyoma developed symptomatic frequent premature ventricular contractions. Among the three fibroma cases, two were surgical resected, one obstructing the left ventricle outflow tract presenting with syncope and low exercise tolerance, and the other causing significant mitral valve impairment. The patient with a rare left ventricle myxoma was submitted to surgical resection due to embolic risk. Finally, a 14-year-old boy was diagnosed with a pericardial teratoma causing right atrial compression and was diagnosed in the context of acute pericarditis with significant pericardial effusion. After the tumour resection, the patient developed two further episodes of acute pericarditis. We have no cardiac tumour-related deaths to report. With the exception of the four resected tumours, in which a biopsy of the surgical piece was performed, in the others the diagnosis was assumed based on the sum of imaging characteristics, tumour location, capacity of spontaneous regression, and clinical outcome. We suggest the algorithm illustrated in Flow chart 1 for the diagnostic approach of cardiac tumours.
Table 2. Cardiac tumours in our centre.

ASD = atrial septal defect; CHD = congenital heart disease; IVS = interventricular septum; LA = left atrium; LV = left ventricle; PND = prenatal diagnosis; PVC = premature ventricular contraction; RA = right atrium; RV = right ventricle; TS = tuberous sclerosis; VSD = ventricular septal defect

Flow chart 1. Diagnostic approach to cardiac tumours. CT = computerized tomography; MRI = magnetic resonance imaging; TTE = transthoracic echocardiogram
Benign tumours
Rhabdomyomas
Rhabdomyomas are the most common primary heart tumours in infants and children and represent 40–60% of paediatric heart tumours.Reference Burke and Virmani12 Some authors do not considered it a real tumour but rather a non-neoplastic paediatric hamartomatous lesion.Reference Burke and Virmani12,Reference Freedom, Lee, MacDonald and Taylor13 It has a close association with tuberous sclerosis, an autosomal dominant disorder.Reference Scollon, Anglin, Thomas, Turner and Wolfe Schneider14 It is estimated that 80% of patients with rhabdomyomas have tuberous sclerosis, while 50% of patients diagnosed with tuberous sclerosis have cardiac hamartomas.Reference Thomas-de-Montpréville, Nottin, Dulmet and Serraf15 However, it can also occur sporadically or in association with CHDs. Depending on the size and location, they can obstruct the ventricular outflow tracts mimicking pathologies like tetralogy of Fallot or left heart hypoplastic syndrome, depending on the site of obstruction.Reference Lefort, Lothion, Arid and El16,Reference Mir, Ikemba and Reddy17 Heart failure can develop not only in the setting of an obstructive mass but also precipitated by an arrhythmia secondary to conduction system invasion.Reference Sadoh, Obaseki and Amuabunos18 In foetal life, atrioventricular reentrant tachycardia is the most common and can precipitate foetal hydrops.Reference Wakai, Strasburger, Li, Deal and Gotteiner19 In fact, even asymptomatic foetuses with rhabdomyomas can present with conduction disorders, especially associated with Wolff–Parkinson–White pattern, which implies that the tumours can effectively form an accessory pathway.Reference Wacker-Gussmann, Strasburger, Cuneo, Wiggins, Gotteiner and Wakai20 A remarkable characteristic of these tumours is their spontaneous regression over the first years of life.Reference Mendes, Araújo, Anjos and Teixeira21 This is due to their hormone dependency involving the ubiquitin pathway, losing their mitotic potential after birth.Reference Yadava3 They can present as either single or, often, multiple masses, with a predilection for the interventricular septum and ventricular cavities. They are hyperechogenic and homogeneous on echocardiography (Fig 1), and cardiac magnetic resonance features include iso to hyperintense signals on T1, hyperintense on T2-weighted images, and enhance less than myocardium after contrast administration (Fig 2).Reference Tao, Yahyavi-Firouz-Abadi, Singh and Bhalla22 Definitive diagnosis is by histology which shows pathognomonic spider cells with myofibrils radiating to the cell wall.Reference Kewcharoen, Prasongdee and Sinphurmsukskul9 An expectant approach is recommended in asymptomatic cases. Surgical resection is advocated only when there is vulvar impairment, ventricular dysfunction, or refractory dysrhythmias. Successful induced regression was reported with the use of mammalian target of rapamycin inhibitors everolimusReference Martínez-García, Michel-Macías and Cordero-González23,Reference Shibata, Maruyama and Hayashi24 and sirolimus.Reference Lee, Song, Cho, Choi, Ma and Cho25,Reference Weiland, Bonello and Hill26 A phase II trial for the use of everolimus for rhabdomyomas regression in children with tuberous sclerosis is ongoing.Reference Stelmaszewski, Parente and Farina27
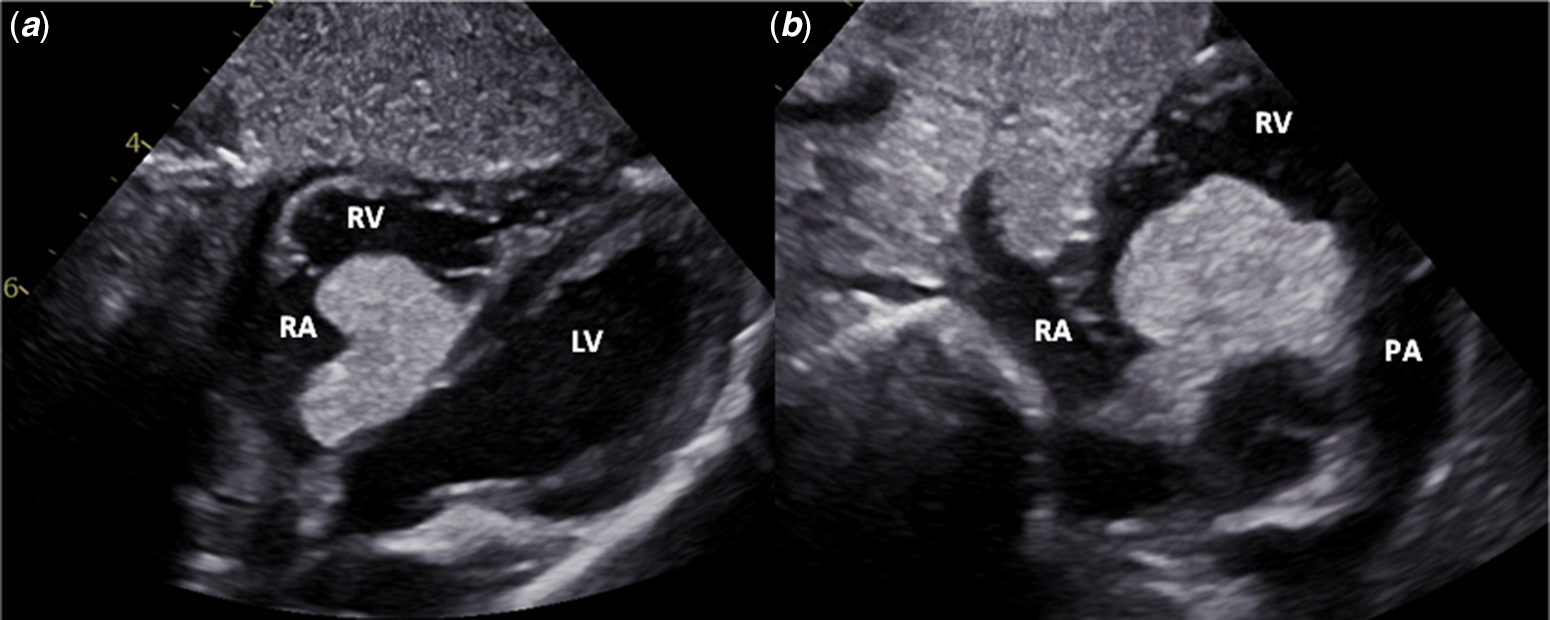
Figure 1. Transthoracic echocardiogram – A) Subcostal, long-axis view. B) Subcostal, short-axis view. Large rhabdomyoma adherent to the triscuspid valve, prolapsing into both the right atrium and right ventricle. LV – left ventricle; PA – pulmonary artery; RA – right atrium; RV – right ventricle.
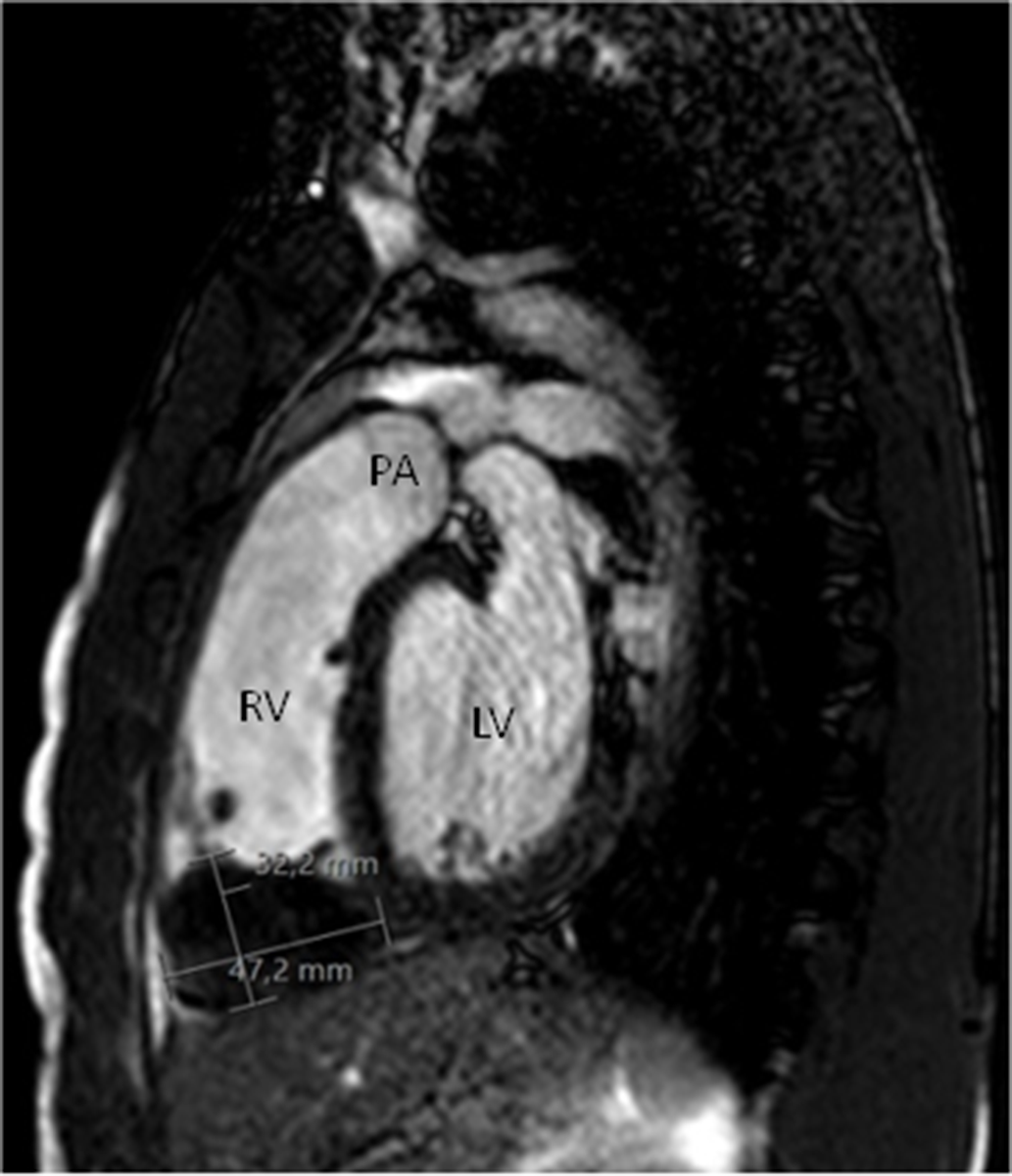
Figure 2. Cardiac magnetic resonance – Sagittal view. Large rhabdomyoma in the right ventricle. LV = left ventricle; PA = pulmonary artery; RV = right ventricle.
Fibromas
Fibromas are the second most common cardiac tumours in infancy and account for 30–50% of paediatric heart tumours.Reference Paramés, Freitas and Martins10 The vast majority occur sporadically but cardiac fibromas are present in 3–5% of patients with Gorlin’s syndrome.Reference Scollon, Anglin, Thomas, Turner and Wolfe Schneider14 The tumour’s cells derive from connective tissue fibroblasts and normally appear as a giant single mass in the interventricular septum or both the left and right ventricular free walls.Reference Castillo and Silvay5 Despite its benignity, they tend to cause obstructionReference Marshall, Dabal and Law28 to blood flow and sudden death can be a form of presentation.Reference Dominguez, Perkins, Duque and Bravo29 Several patients have accidental diagnoses but even these can present with symptoms later in life or electrocardiographic abnormalities.Reference Cordinhã, Pereira and Silva30–Reference Varlamis, Chalemis and Haritandi32 A large heterogeneous solid mass observed echocardiographically (Fig 3) strongly suggests this tumour type, but the most pathognomonic sign is the existence of central calcification on CT.Reference Uzun, Wilson, Vujanic, Parsons and De Giovanni7 The calcification occurs because of lack of blood supply to the mass, hence related to ischaemic changes. At cardiac magnetic resonance, in relation to the myocardium, it appears as hypo to isointense on T1 and hypointense on T2-weighted images (Fig 4). With contrast administration and first-pass perfusion, a hypoperfused image is revealed, different from the surrounding perfused myocardium.Reference Tao, Yahyavi-Firouz-Abadi, Singh and Bhalla22 Histologically fibromas are made up of unencapsulated masses of fusiform cells that blend with or infiltrate the normal myocardium. Areas of calcification, necrosis, and cystic degeneration are common.Reference Freedom, Lee, MacDonald and Taylor13,Reference Dominguez, Perkins, Duque and Bravo29 Fibromas do not spontaneously regress and, as a group, represent the most resected cardiac tumour type in children.Reference Castillo and Silvay5 Total or partial resection is advocated in symptomatic patients and in asymptomatic with giant masses.Reference Xu, Wu, Li and Zhang33 Heart transplant may be needed in the setting of severe heart failure.Reference Shi, Wu and Fang34
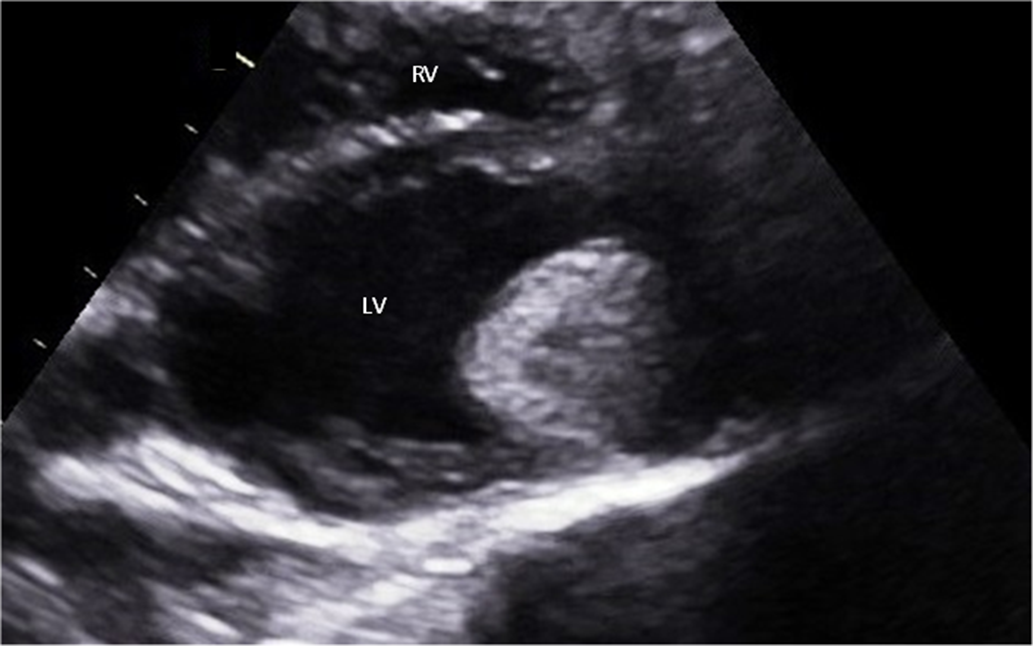
Figure 3. Transthoracic echocardiogram – Parasternal short-axis view. Giant fibroma in the left ventricle. LV = left ventricle; RV = right ventricle.
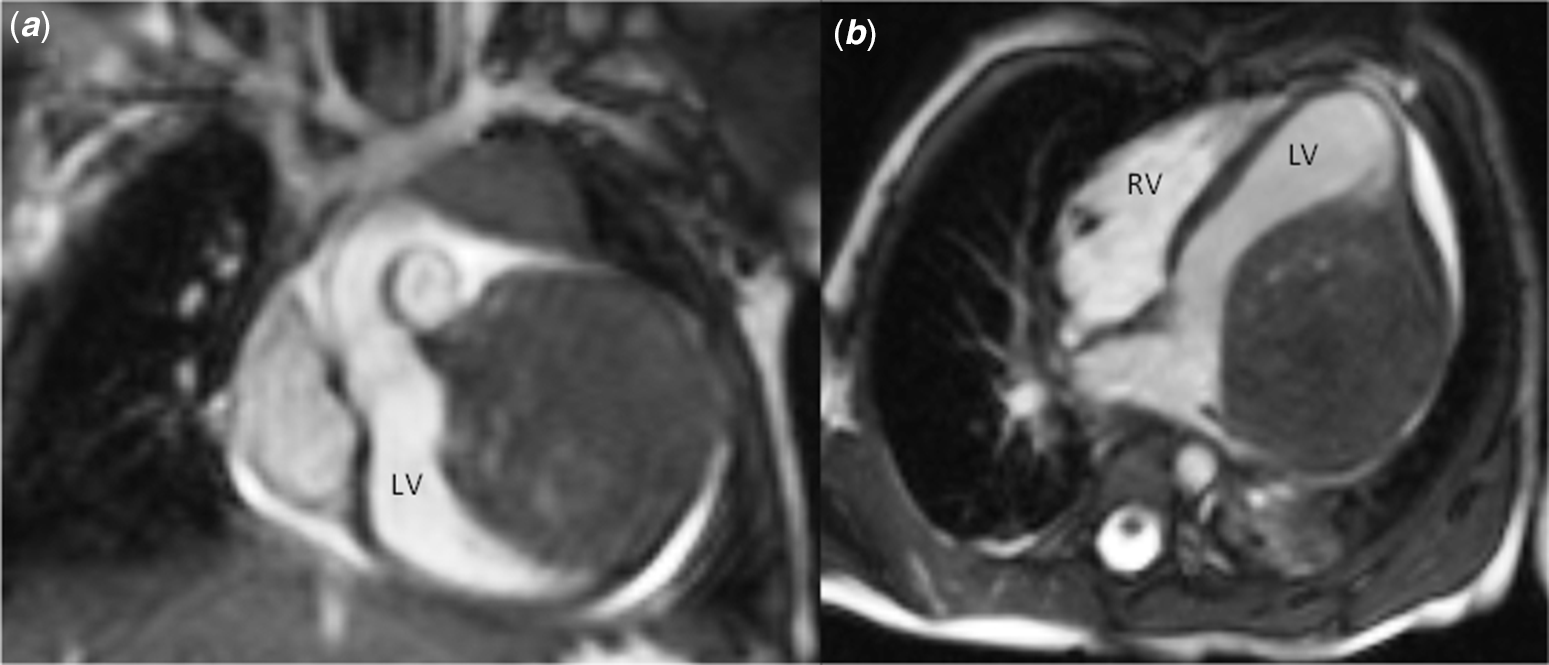
Figure 4. Cardiac magnetic resonance. ( a ) Coronal view; ( b ) axial view. Large fibroma in the left ventricle. LV = left ventricle; RV = right ventricle.
Teratomas
Teratomas are the third most common cardiac tumours in children, accounting for 1–16% of cases, and have a slightly female predominance.Reference Poterucha, Kochav, O’Connor and Rosner6,Reference Burke and Virmani12 However, in foetuses and neonates, it can represent up to 25% of all cardiac tumours, being second to rhabdomyomas.Reference Carrilho, Tonni and Araujo2,Reference Uzun, Wilson, Vujanic, Parsons and De Giovanni7 Although teratomas are essentially benign tumours, 15% are malignant based on the amount of immature neuroepithelium.Reference Pratt, Cohen, Mutabagani, Davis and Wheller35 They are extracardiac masses, within the pericardial cavity, in close relationship with the great vessels or venous return (Fig 5), carrying the risk of pericardial effusions and tamponade.Reference Pratt, Cohen, Mutabagani, Davis and Wheller35,Reference Moura Garcia, Nery Dantas Junior, Kai Chi and Rodrigues Parga36 The main concerns are hydrops and stillbirth in the foetus and respiratory distress, cyanosis, and congestive heart failure in the neonate.Reference Uzun, Wilson, Vujanic, Parsons and De Giovanni7 There are rare cases of reported intracardiac teratomas, most commonly related to the interventricular septum. They may protrude into right ventricle, potentially causing obstruction or dysrhythmias.Reference Kahlbau, Gomes, Pinto and Fragata37–Reference De Bellaing, Houyel and Bonnet39 Diagnosis is made in setting of an heterogeneous mass at echocardiography, most likely in the pericardial sac. At cardiac magnetic resonance, they show up as iso or hypointense on T1, hyperintense on T2-weighted images, being hypointense after the enhanced contrast phase.Reference Tao, Yahyavi-Firouz-Abadi, Singh and Bhalla22 Histologically teratomas are typically multicystic lesions composed of a combination of the three germ layers, the endoderm, mesoderm, and ectoderm. Surgical resection is the only treatment if the patient is symptomatic and removal of the entire mass should be attempted due to their high recurrence rate, only surpassed by myxomas.Reference Tzani, Doulamis, Mylonas, Avgerinos and Nasioudis1

Figure 5. Angio computerised tomography. ( a ) Coronal view; ( b ) axial view. Large teratoma in the pericardial sac, compressing the superior vena cava and the right atrium.
Myxomas
Myxoma are, by far, the most common cardiac tumour in adults.Reference Castillo and Silvay5 However, in children they represent only 10% of all cardiac tumours, mainly found during adolescence. Myxomas typically arise from the region of the fossa ovalis and can be pedunculated or have a broad attachment base. In 75%, they protrude to the left atrial cavity and in 10–15% into the right atrial cavity.Reference Poterucha, Kochav, O’Connor and Rosner6,Reference Freedom, Lee, MacDonald and Taylor13,Reference Younes, Al-Dairy and Albadr40 Other locations are possible but occur less often,Reference Mani, Gopalakrishnan, Ayyappan and Valaparambil41,Reference Kumagai, Sai, Endo and Tabayashi42 like our 14-year-old boy presenting with a fast growing myxoma in the left ventricle (Fig 6). Although 90% occur sporadically, the remainder is associated with Carney complex, an autosomal dominant inherited disease.Reference Burke and Virmani12 Myxomas fragments are prone to embolisation, and constitutional symptoms are the main form of presentation in adults. Although cerebral vascular events may be a form of presentation during childhood in the context of left atrial myxomas,Reference Wu, Fu and Liao43 congestive heart failure due to valvular obstruction has been reported to be the leading cause in children.Reference Padalino, Basso, Moreolo, Thiene and Stellin44 Another form of presentation is with a paraneoplastic syndrome, such as vasculitis, usually carrying a poorer prognosis.Reference Macias, Nieman and Yomogida45 At echocardiography, in addition to their typical location, they are heterogeneous masses with small lucencies or calcifications (Fig 6). At cardiac magnetic resonance, they are hypointense on T1, hyperintense on T2-weighted images, demonstrate heterogeneous contrast enhancement, and may present foci of fibrosis or haemorrhage.Reference Tao, Yahyavi-Firouz-Abadi, Singh and Bhalla22 Histologically, they are made up of eosinophilic cells dispersed or agglomerated in a myxoid stroma that can undergo fibrosis or calcification.Reference Freedom, Lee, MacDonald and Taylor13 Although there are reported cases of natural regression,Reference Guntheroth, Fujioka and Reichenbach46 surgical resection is indicated due to the associated risk of cerebral embolisation or sudden cardiac death.Reference Shi, Wu and Fang34 Myxoma is known to have the highest recurrence rate,Reference Tzani, Doulamis, Mylonas, Avgerinos and Nasioudis1 either related to its incomplete resection or due to inherited conditions. Patients with Carney complex can have several recurrences and cardiac transplant may be the only option.Reference Kewcharoen, Prasongdee and Sinphurmsukskul9 In sporadic myxomas, the survival of patients submitted to complete surgical resection is not different from that of an age and gender match population.Reference Elbardissi, Dearani and Daly47
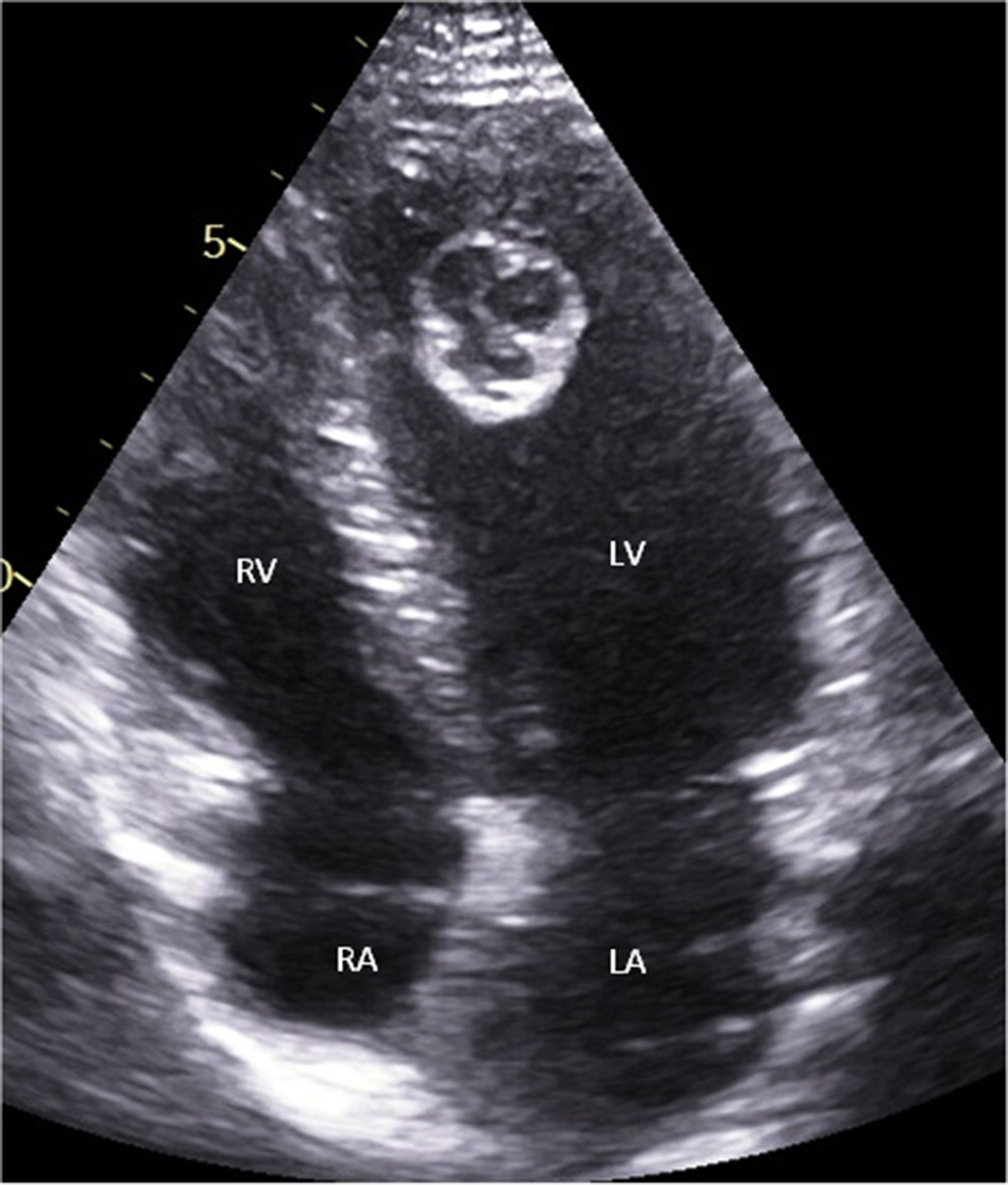
Figure 6. Transthoracic echocardiogram – Apical view. Pedunculated myxoma in left ventricle. LA = left atrium; LV = left ventricle; RA = right atrium; RV = right ventricle.
Haemangiomas
Cardiac haemangiomas are vascular benign tumours which affect children and adults and represent around 5% of all cardiac tumours in paediatric age groups.Reference Uzun, Wilson, Vujanic, Parsons and De Giovanni7,Reference Burke and Virmani12 They can originate in the pericardial sac, any cardiac chamber, or valve. The endocardium is more affected than the myocardium,Reference Onan, Haydin, Onan, Akdeniz, Odemis and Bakir48 and there seems to be a predilection for the right atrium in neonates.Reference Uzun, Wilson, Vujanic, Parsons and De Giovanni7 The clinical presentation is varied, ranging from the asymptomatic patient to sudden cardiac death.Reference Cohen, Collazo, Firan, Dangol and Atkins49,Reference Zerbo, Argo, Maresi, Liotta and Procaccianti50 There is also an increased risk of bleeding. Echocardiographically, the tumour appears as a heterogeneous mass and at cardiac magnetic resonance it is isointense on T1, hyperintense on T2-weighted images, and show avid enhancement following intravenous gadolinium injection.Reference Tao, Yahyavi-Firouz-Abadi, Singh and Bhalla22 These image signals may be no different from other vascular tumours, namely malignant ones, thus requiring histological analysis for its differentiation. The procedure may be potentially complicated because of the bleeding propensity of the tumour. This analysis may differentiate the tumours in cavernous, capillary, or arteriovenous types, where multiple, dilated, thin-walled vessels are found in the cavernous type and small capillary-like vessels in capillary type.Reference Onan, Haydin, Onan, Akdeniz, Odemis and Bakir48 Although spontaneous regression is possible, mainly in the neonates,Reference Mackie, Kozakewich, Geva, Perez-Atayde and Mulliken51,Reference Heifetz, Faught and Bauman52 the natural course of cardiac haemangiomas is unpredictable and surgical resection is advisable with excellent prognosis and no recurrence.Reference Yadava3 When resection is not feasible, response to steroids has also been reported.Reference Uzun, Wilson, Vujanic, Parsons and De Giovanni7
Histiocytoid cardiomyopathy
Also known as oncocytic cardiomyopathy or Purkinje cell tumour, this benign tumour is very rare and is exclusive to children, specially under the age of 2 years.Reference Burke and Virmani12 It has a female predominance (3:1) and presents with a multivariate of a difficult to control and sometimes fatal arrhythmias, caused by multifocal hamartomatous proliferation of cardiac cells with oncocytic features. Ventricular fibrillation, ventricular tachycardia, and junctional tachycardia are the main electrical disturbances.Reference Paramés, Freitas and Martins10 Cardiomegaly is inadvertently seen at autopsies and is caused by the endocardial infiltration of multiple yellow-tan nodules, mainly in the ventricular wall, but all cardiac layers may be affected, including valvular tissue.Reference Zerbo, Argo, Maresi, Liotta and Procaccianti50 Microscopically, these nodules are composed of polygonal cells with a foamy to granular cytoplasm. Typically, myocytes are filled with abnormal mitochondria that replace the normal myofibrils, hence the term oncocytic.Reference Uzun, Wilson, Vujanic, Parsons and De Giovanni7 The distinction between histiocytoid cardiomyopathy and mitochondrial cardiomyopathy is that, in the former, only focal regions of the heart are involved in the disease process but all myocytes show the described pattern, while in the latter all myocytes are affected but with different degrees of affection.Reference Shehata, Patterson, Thomas, Scala-Barnett, Dasu and Robinson53 The treatment is based on electrophysiological mapping, surgical or percutaneous ablation of the arrhythmogenic foci, and surgical resection of the nodules. As a last resource, transplantation may be necessary.Reference Zangwill, Trost, Zlotocha, Tweddell, Jaquiss and Berger54
Inflammatory myofibroblastic tumours
Inflammatory myofibroblastic tumours are benign lesions that occur mainly in the lung, soft tissue, and viscera of children and young adults, the heart being a rare site of its manifestation.Reference Burke and Virmani12 Inflammatory myofibroblastic tumours is more frequent in females and usually manifest at the 10 years mean.Reference Eilers, Nazarullah, Shipper, Jagirdar, Calhoon and Husain55 Although this endocardial tumour can develop in any chamber, there appears to be a right-sided predominance, and the valves can also be affected. Obstruction of coronary arteries due fragments embolisation is a possible complication, resulting in myocardial infarction.Reference Kheiwa, Turner and Schreiber56 In addition to myocardial infarction and tumour site derived symptoms, one-third of patients present with constitutional symptoms, such as fever, weight loss, malaise, and unspecific viral respiratory or gastrointestinal viral symptoms.Reference Eilers, Nazarullah, Shipper, Jagirdar, Calhoon and Husain55,Reference Pang, Merritt, Shkrum and Tijssen57 Echocardiographically, inflammatory myofibroblastic tumours appear as a heterogeneous mass arising from the endocardium. At cardiac magnetic resonance, the mass appears as isointense on T1, hypointense on T2 weight images and demonstrates intense delayed contrast enhancement.Reference Tao, Yahyavi-Firouz-Abadi, Singh and Bhalla22 Blood analysis is also important, since an elevated sedimentation rate, thrombocytosis, iron-deficiency anaemia, and hypergammaglobulinemia are commonly present and contribute to the diagnosis, even in the absence of constitutional symptoms.Reference Kheiwa, Turner and Schreiber56 Macroscopically, the appearance is either a solid yellow glistening pedunculated mass or with a base broad attachment. Histological analysis allows for the correct diagnosis, as the findings of spindled myofibroblastic proliferation and chronic inflammatory infiltrate are pathognomonic features.Reference Eilers, Nazarullah, Shipper, Jagirdar, Calhoon and Husain55 Surgical resection is advocated, when feasible, otherwise there are reported cases of successful regression with oral steroids.Reference Ferbend, Abramson and Backer58 Although carrying a good prognosis after resection, the tumour may recur, eventually leading to the patient’s demise.Reference Andersen, DiBernardo, Linardic, Camitta and Lodge59
Papillary fibroelastomas
Papillary fibroelastomas are the third most common benign cardiac tumour in the adult population with the highest rate of valvular involvement.Reference Karimi, Vining, Pellenberg and Jajosky60,Reference Chadha, Cooke, Shillingford and Ceithaml61 Despite this incidence in adults, which has its highest cadence in the eighth decade of life, it is extremely rare in children, with only a few cases reported.Reference Chadha, Cooke, Shillingford and Ceithaml61–Reference Wang, Gong, Xie and Wang64 Overall, the vast majority occur in the left-sided valves, mainly in the aortic. However, in the paediatric population, several have been reported in the tricuspid valve. This tumour shows a great propensity to embolise, either due to tumour fragments or thrombi formed around the mass, with consequent stroke or pulmonary thromboembolism. It is thought that the origin of papillary fibroelastoma may be secondary to endothelial lesions in adults; however, the existence of congenital and infantile presentations raise the possibility of an underlying hamartomatous origin.Reference Dénes, Daron and Behaeghe62 Papillary fibroelastomas appears as a well-circumscribed homogeneous mass at echocardiography, pedunculated in half the cases.Reference Sun, Asher and Yang65 At cardiac magnetic resonance, it is isointense in relation to the myocardium on both T1- and T2-weighted images, reflecting its fibroelastic composition, and absence of low gadolinium enhancement, typical of an avascular tumour.Reference Hoey, Shahid and Ganeshan66 Macroscopically, the tumour resembles a sea anemone when immersed in water. Histologically, it is composed of a central core of connective tissue surrounded by a layer of acid mucopolysaccharide.Reference Sun, Asher and Yang65 Surgical resection, often requiring valvar replacement, is the treatment of choice.Reference Shi, Wu and Fang34 An expectant approach may be used to asymptomatic patients with small (infracentimetric), left-sided, non-pedunculated tumours, but the general consensus is to resect these in early life, due to the high risk of embolisation.Reference Sun, Asher and Yang65
Lipomas
Primary cardiac lipomas were thought to be exclusive of adults.Reference Uzun, Wilson, Vujanic, Parsons and De Giovanni7 However, a few reported paediatric cases have been published.Reference Shi, Wu and Fang34,Reference Friedberg, Chang, Silverman, Ramamoorthy and Chan67,Reference Husain, McCanta and Batra68 These tumours are encapsulated masses of adipose tissue, accidentally diagnosed at autopsies or, rarely, with symptoms triggered by arrhythmias, namely ventricular tachycardias.Reference Friedberg, Chang, Silverman, Ramamoorthy and Chan67,Reference Husain, McCanta and Batra68 They can develop anywhere in the heart but are usually seen in the atrial septum and epicardium growing into the pericardial space. Their appearance on echocardiography is varied, so the most adequate exam is cardiac magnetic resonance, where they typically are hyperintense on both T1- and T2-weighted images which fully supress with fat saturation. There is no first pass or late contrast enhancement, coincident with the avascular nature of the tumour.Reference Hoey, Shahid and Ganeshan66 Surgical resection is only needed in symptomatic patients.
Malignant tumours
Sarcomas
Malignant cardiac tumours account for 8% of cardiac tumours in the paediatric populationReference Padalino, Reffo and Cerutti69 and are mainly secondary. Although rare, sarcomas represent 95% of primary tumours.Reference Uzun, Wilson, Vujanic, Parsons and De Giovanni7 There are only a few reported cases of cardiac sarcomas in children,Reference Thomas-de-Montpréville, Nottin, Dulmet and Serraf15,Reference Itoh, Matsumura and Egawa70–Reference Gehrmann, Kehl, Diallo, Volker and Johannes72 the majority, as in adults, are right-sided, although some involved the mitral valve.Reference Itoh, Matsumura and Egawa70 There are several types of sarcomas; the most common in adults is the angiosarcomaReference Thomas-de-Montpréville, Nottin, Dulmet and Serraf15 which has a male predominance. However, the most common in children is the rhabdomyosarcoma which typically affects the myocardium and the pericardium.Reference Shanmugam73 Besides these two types, undifferentiated sarcomasReference Itoh, Matsumura and Egawa70,Reference Ludomirsky, Vargo, Murphy, Gresik, Ott and Mullins71 and one leiomyosarcomaReference Gehrmann, Kehl, Diallo, Volker and Johannes72 have been reported in children. These tumours are extremely aggressive, invading locally, obstructing the valves and the outflow tracts, causing pericardial and pleural effusion, and invading the great vessels and veins. At the time of the diagnosis, distant metastasis is a frequent finding.Reference Shanmugam73 At echocardiography, they often appear as broad-based masses.Reference Mendes, Araújo, Anjos and Teixeira21 Cardiac magnetic resonance images vary depending on tumour type. The undifferentiated sarcoma is typically isointense in relation to the myocardium; the rhabdomyosarcoma and fibrosarcoma are isointense or present with heterogeneous signal intensity; leiomyosarcoma presents an intermediate signal intensity on T1 which increases on T2-weighted images; angiosarcoma presents with a sun ray appearance with linear contrast enhancement.Reference Shanmugam73 Due to their aggressive nature, these patients need adjuvant chemotherapy and or radiotherapy, as complete tumour excision is often impossible.Reference Shi, Wu and Fang34 They carry a poor prognosis.Reference Uzun, Wilson, Vujanic, Parsons and De Giovanni7
Lymphomas
Primary cardiac lymphomas make up the remaining 5% of primary malignant tumours in general population.Reference Uzun, Wilson, Vujanic, Parsons and De Giovanni7 They are extranodal, non-Hodgkin lymphomas that arise from the heart and/or the pericardium, with a predilection for the right atrium.Reference Carras, Berger and Chalabreysse74 These extremely rare tumours may present with heart failure or pericardial effusion.Reference Uzun, Wilson, Vujanic, Parsons and De Giovanni7 Echocardiography may evidence one or more masses that are hypo- to isointense on T1 and isointense relative to myocardium on T2-weighted images in cardiac magnetic resonance. Heterogeneous enhancement may be seen after contrast administration.Reference Tao, Yahyavi-Firouz-Abadi, Singh and Bhalla22 The most common type is the diffuse large B-cell lymphoma.Reference Carras, Berger and Chalabreysse74 Treatment is based on chemotherapy with or without surgical resection.
Metastatic cardiac tumours
In the general population, secondary cardiac tumours are 10–20 times more prevalent than the primary counterparts.Reference Uzun, Wilson, Vujanic, Parsons and De Giovanni7 Shi et alReference Shi, Wu and Fang34 analysed 166 paediatric cardiac tumours and they found that cardiac metastases represented 3.6% of the cases. In adults, melanoma is the neoplasm with the greatest affinity for cardiac involvement; however, lung tumours are the principal source of cardiac metastases in men and breast tumours in women.Reference Castillo and Silvay5 Huh et alReference Huh, Noh and Kim75 reported eight cases of secondary cardiac tumours in children, and the primary tumours were lymphoma (three), Wilms’ tumour (two), malignant teratoma, neuroblastoma, and pleuropulmonary blastoma. Besides these osteosarcomas also appear to be an important primary lesion in children.Reference Gross, Postovsky and Khoury76–Reference Hartemayer, Kuo and Kent78 Cardiac involvement occurs mainly through the lymphatic and haematogenous routes, and the right side of the heart is more affected. Unexplained cardiomegaly, congestive heart failure, arrhythmia, or symptoms of right or left cardiac dysfunction in an oncological patient without previous heart disease should prompt an investigation for cardiac metastases. At echocardiography, an atrial mass is the most common finding which enhances with contrast at cardiac magnetic resonance.Reference Tao, Yahyavi-Firouz-Abadi, Singh and Bhalla22 Chemotherapy with or without surgical resection is the treatment of choice but the prognosis is poor. In a review of 21 patients with cardiac metastases secondary to osteosarcoma, the median disease-free survival time was 12 months.Reference Hartemayer, Kuo and Kent78
Foetal cardiac tumours
The incidence of foetal cardiac tumours is slightly superior to that in children, estimated to be 0.08–0.2%.Reference Carrilho, Tonni and Araujo2 The relative frequency among the tumours types is similar to that found in children, with the exceptions of a higher incidence of rhabdomyomas (60%), which can naturally regress before birth, and a higher incidence of teratomas (25%), which is the second more frequent in this age, instead of fibromas (12%).Reference Carrilho, Tonni and Araujo2 The mechanisms for cardiac dysfunction are the same as in children, but a higher grade of suspicious is required for detection. Reverse flow in the ascending aorta or in the pulmonary trunk, or an increased flow in the circumflex artery, should prompt the physician to look out for causes of obstruction to the outflow tracts.Reference Carrilho, Tonni and Araujo2 Diagnosis can be made using foetal echocardiography (Fig 7) and magnetocardiography has proven to be a sensible exam to detect arrhythmias and conduction disorders even in asymptomatic foetuses.Reference Wacker-Gussmann, Strasburger, Cuneo, Wiggins, Gotteiner and Wakai20 Drug treatment of the malignant arrhythmias should start immediately and sotalol seems better for this purpose than digoxin in supraventricular tachycardia.Reference Wakai, Strasburger, Li, Deal and Gotteiner19,Reference Wacker-Gussmann, Strasburger, Cuneo, Wiggins, Gotteiner and Wakai20 If foetal hydrops is present, intrauterine pericardiocentesis may be necessary. A tumour size greater than 20 mm and foetal dysrhythmia seem to be predictors of increased neonatal morbidity.Reference Chao, Chao and Wang79
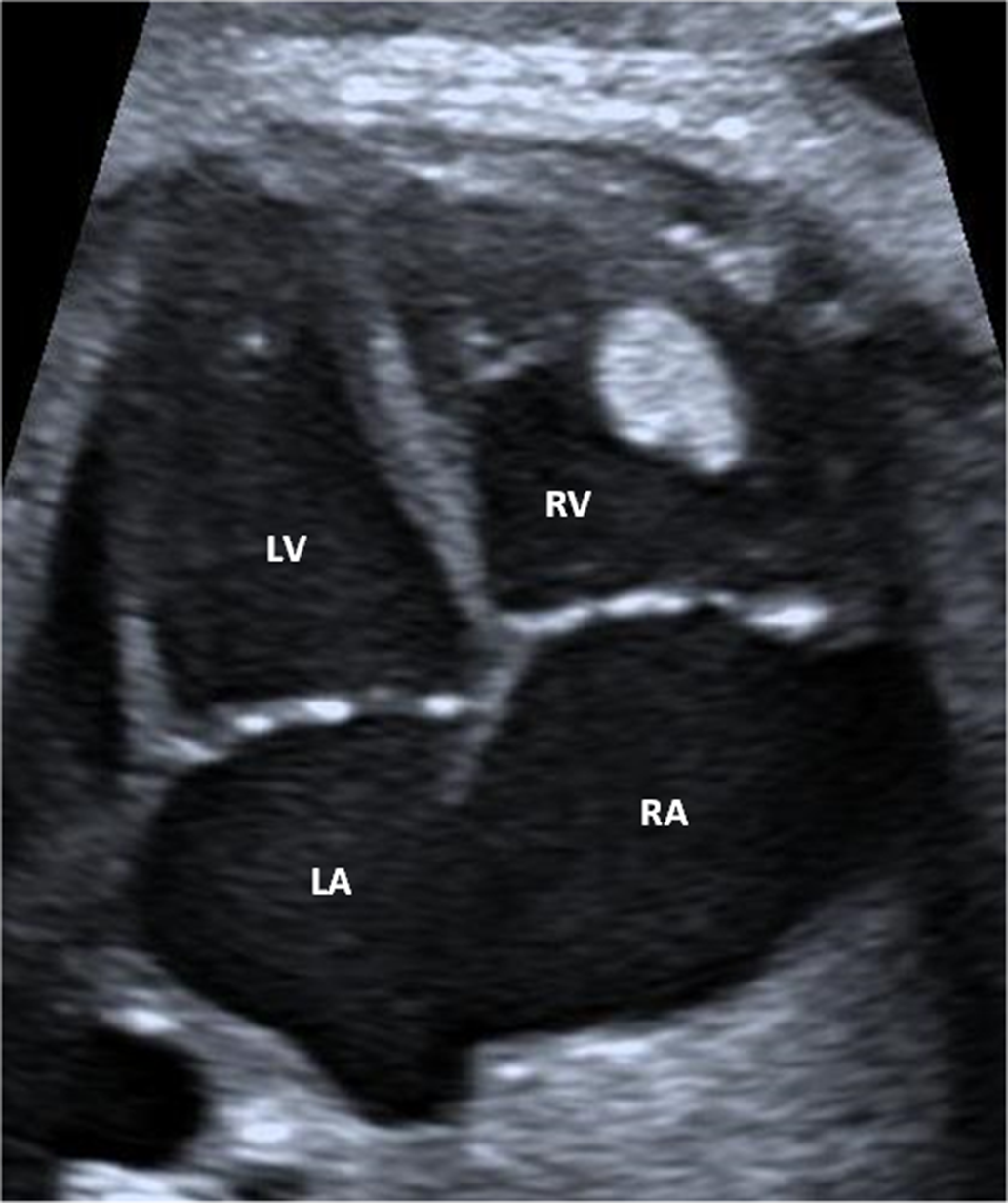
Figure 7 Foetal echocardiogram. Rhabdomyoma adherent to the interventricular septum and extending into the right ventricle. LA = left atrium; LV = left ventricle; RA = right atrium; RV = right ventricle.
Lesions mimicking cardiac tumours
Cardiac thrombus is the main differential diagnosis of a cardiac tumour. The suspicious should be higher in patients with central venous catheters. At echocardiography, a thrombus is typically a mobile intraluminal mass. Its characteristics at cardiac magnetic resonance depend on its duration. An acute thrombus is hyperintense on T1- and T2-weighted images, a subacute thrombus is hyperintense on T1 but hypointense on T2-weighted images, and chronic thrombus is usually hypointense in both T1- and T2-weighted images.Reference Tao, Yahyavi-Firouz-Abadi, Singh and Bhalla22
Pericardial cysts are part of the differential diagnosis. It typically occurs in the right cardiophrenic angle in the mediastinum. At cardiac magnetic resonance, they are hyperintense on T2-weighted images and do not enhance after contrast administration.Reference Tao, Yahyavi-Firouz-Abadi, Singh and Bhalla22
Conclusion
Cardiac tumours are extremely rare in children and the majority are benign lesions. Despite their benignity, the clinical presentation may range from accidental diagnosis to malignant arrhythmias, obstructive symptoms and ultimately, sudden death. The definitive diagnosis is only possible through histological analysis; however, it is possible to infer about tumour type and respective natural history based on the patient’s age, its location, and imaging characteristics. When indicated, surgical resection is the main treatment of choice; however, when it is not feasible, other non-invasive treatments have shown promising results, depending on tumour type.
Acknowledgements
The authors would like to thank all the medical staff of the Paediatric Cardiology Department of Centro Hospitalar e Universitário de Coimbra, for their fine contribution with the echocardiographic images.
Financial support
This research received no specific grant from any funding agency, commercial, or not-for-profit sectors.
Conflicts of interest
None.













