Published online by Cambridge University Press: 21 January 2005
Scimitar syndrome is a rare congenital anomaly that affects classically the right lung and the heart. We present a rare variant that involves both lungs in association with totally anomalous pulmonary venous connection, horseshoe lung, and right pulmonary cyst.
Scimitar syndrome, or the hypogenetic lung syndrome, is a rare congenital anomaly. In the complete form, the syndrome is characterized by hypoplasia of the right lung, anomalous systemic arterial supply to its lower lobe, abnormalities in pulmonary venous drainage of part or all the right lung into the inferior caval vein, hypoplasia of pulmonary arteries and abnormalities in the bronchial tree.1 To date, the syndrome has been described almost exclusively involving the right side. Left-sided variants, and the bilateral form, are rarely reported in medical literature.2, 3 Because of its complex make-up, various diagnostic modalities are often needed to confirm the diagnosis.4, 5 In this report, we describe a unique case seen in an infant with involvement of both lungs, totally anomalous pulmonary venous connection, horseshoe lung and a right pulmonary cyst.
A newborn boy was referred to our hospital with the suspicion of having congenital cardiac disease. On admission, he required intubation and mechanical ventilation. Saturations of oxygen measured by pulse oximetry were 95% on room air. Examination revealed a grade 3/6 murmur with hepatomegaly. The plain chest radiograph showed shifting of the enlarged heart to the right side, a cystic radiolucent lesion in the right middle lobe adjacent to the right cardiac border, and an unusual vertical curvilinear shadow resembling the shape of a scimitar in the left lung (Fig. 1).
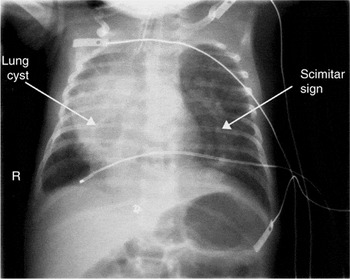
Figure 1. The chest radiograph shows a left scimitar, right lung cyst, and right-sided heart.
An echocardiographic study was performed and showed a right-sided heart with the apex pointing to the left and an unrestricted atrial septal defect with right-to-left shunting. There was a large aorto-pulmonary collateral artery of 3–4 mm diameter arising from the descending abdominal aorta that fed the lower lobe of the right lung. No connection could be seen between the pulmonary veins and the left atrium. The right-sided pulmonary veins were seen to drain to the inferior caval vein near its junction with the right atrium. Furthermore, there was an unobstructed left-sided vein crossing the diaphragm and joining the inferior caval vein through the liver. The findings raised the suspicion of totally anomalous pulmonary venous connection.
To investigate further the cardio-pulmonary abnormalities, we performed a contrast enhanced computerized tomographic scan of the chest (Fig. 2).

Figure 2. Chest angio-computerized scan showing bilateral scimitars, along with the aberrant systemic arterial supply from the descending aorta. SCV: superior caval vein; AO: aorta.
This confirmed that a large vein extended from the middle of the left lung, crossed the diaphragm, and connected via the hepatic vein to the inferior caval vein at its junction with the right atrium. This vein also produced a shadow resembling a scimitar. A similar vein, but with a shorter course, drained the right lung to the inferior caval vein at the cavo-atrial junction. In addition, we identified two tortuous aberrant arteries arising from the descending abdominal aorta and supplying the lungs. The larger artery supplied the sequestered right lower lobe, and the smaller one supplied a small part of the left lower lobe. In addition to these vascular components of the scimitar syndrome, seen bilaterally, the chest computerized tomographic scan revealed absence of the right lower bronchus, sequestration of the right lower lobe, and a proportionally small right lung when compared to the left lung. The scan also revealed the presence of two distinctive abnormalities. The first anomaly was a cyst measuring 1.5 by 1.5 cm in the right middle lobe that communicated with the airway. The second anomaly was a bridge of abnormal lung tissue that, through the mediastinum, connected the posterobasal segments of the right and left lungs. This abnormal fusion of the posterobasal segments was equally evident on a nuclear perfusion scan, which confirmed the presence of horseshoe lungs, with hypoplasia of the right lung. Our patient later underwent a diagnostic and interventional cardiac catheterization, which confirmed the diagnosis of bilateral scimitar syndrome, totally anomalous pulmonary venous connection to the inferior caval vein, right pulmonary cyst, and horseshoe lungs. During catheterization, the large aberrant systemic artery supplying the right lower lobe was successfully embolized using a coil measuring 3 by 3 mm. The patient was subsequently extubated and remained in a stable condition. Because of the complexity of the lesions, the associated cardio-pulmonary anomalies and the young age, corrective surgery has presently been judged inadvisable in view of the life-threatening risks. The patient has been discharged for the present, but will be followed for further evaluation and assessment.
First described in 1836, albeit not named as such, scimitar syndrome is a rare association of congenital cardio-pulmonary anomalies.1 Its hallmark is an anomalous right pulmonary vein that drains all or part of the right lung into the inferior caval vein, with this vessel producing the scimitar sign on the chest radiograph. In our case, however, the scimitar sign was more obvious in the left side of the chest radiograph, although the computerized tomographic scan clarifies the presence of bilateral scimitars. Left-sided scimitar syndrome and the syndrome with bilateral scimitars, have rarely been reported.2 In addition to the vascular abnormalities, our patient has an unusual cyst in the right middle lobe, the etiology of which is not clear. It is possible that the structure is a congenital bronchogenic cyst that later became connected to the right middle bronchus. To the best of our knowledge, the association of pulmonary cyst and bilateral scimitar has never previously been reported. Another interesting finding in our patient is the fusion in the posterior-basal portions of the lungs, giving a horseshoe arrangement. This abnormality has been reported in association with a unilateral scimitar, and only recently was reported in one patient with bilateral scimitar syndrome.3
We elected to manage our patient by embolizing the right aorto-pulmonary collateral artery to minimize the left-to-right shunt. This palliative treatment also decreases the incidence of pulmonary hypertension, and improves the symptoms of cardiac failure. At this stage, definitive repair of the anomalous pulmonary venous connection in a baby weighing only 3 kg is judged to be complex and risky. Repair of such totally anomalous pulmonary venous connection has rarely been successful in infants with the scimitar syndrome, being associated with high morbidity and mortality.2, 6 In a published series of 6 cases, one group reported post-operative pulmonary venous stenosis in all cases following repair during infancy.6 Others have noted, nonetheless, that abolition of the systemic arterial flow to the lung minimizes the left-to-right shunt, and reduces the risk of pulmonary hypertension.7 Our patient showed some improvement after occlusion of the systemic-to-pulmonary artery with a coil, although the future prognosis is still in doubt.
Thus, scimitar syndrome is a rare cardiopulmonary disease. Its diagnosis requires a multi-disciplinary approach, and involves various investigational modalities. Management involves interruption of the systemic pulmonary flow, correcting the pulmonary venous return, and may require lobectomy. Prognosis depends on the severity of the vascular lesions and the associated anomalies. The prognosis needs to be guarded for those patients who present in infancy.

The chest radiograph shows a left scimitar, right lung cyst, and right-sided heart.

Chest angio-computerized scan showing bilateral scimitars, along with the aberrant systemic arterial supply from the descending aorta. SCV: superior caval vein; AO: aorta.