Balloon atrial septostomy has become an essential palliative procedure in treating patients with transposition of the great arteries or other cyanotic congenital heart disease with restricted interatrial blood flow. This procedure entails the creation of a non-restrictive atrial communication, optimising atrial blood mixing and thus increasing oxygen saturation in the systemic circulation and lowering the left atrial pressure.Reference Mosca 1 This procedure plays an important role in rapidly stabilising these neonates before undergoing major surgery. Recent studies, however, have underlined a number of complications associated with balloon atrial septostomy.Reference McQuillen, Hamrick and Perez 2 The overall mortality rate of balloon atrial septostomy as reported by the National Institute for Clinical Excellency in 2004 was 3% before further surgery. 3 Among the complications commonly associated with balloon atrial septostomy are transient arrhythmias, necrotising enterocolitis, and cardiac injury or tear. 4 Although there has been an ongoing discussion about stroke as a complication after balloon atrial septostomy, a definitive conclusion is still awaited on this issue.Reference Mosca 1
In recent years, there has been some evidence that postponement of night-time surgical procedures can reduce the risk of undue adverse complications.Reference Faiz, Banerjee, Tekkis, Papagrigoriadis, Rennie and Leather 5 For example, a study related to orthopaedic surgery noted that after-hours procedures had a higher rate of complications because of technical errors associated with non-ideal conditions and shorter operative times.Reference Ricci, Gallagher and Brandt 6 In acute appendicitis, Yardeni et al. concluded that a delay in surgery until the daytime hours did not substantially increase complication rates and operating time. Instead, the delayed management of patients proved to be a more effective and efficient use of hospital resources.Reference Yardeni, Hirschl and Drongowski 7
To our knowledge, it is not yet known whether the timing of a balloon atrial septostomy has an impact on outcome or complication rates. Through the analysis of data collected retrospectively, this study aims to determine whether the performance of balloon atrial septostomy out-of-hours has a significant impact on the incidence of adverse outcome measures in infants.
Methods
Patients
A total of 113 consecutive neonates who underwent balloon atrial septostomy were identified from our departmental electronic database (Heart Suite, Systeria Limited, Glasgow, United Kingdom). All infants who had undergone balloon atrial septostomy between January 2004 and June 2010 were considered for inclusion in the study. Owing to incomplete patient records, five patients were excluded from the study, whereas two other neonates were excluded because of attempted but unsuccessful procedures. Patient data evaluated included birth weight, pre- and post-balloon atrial septostomy arterial oxygen saturations measured transcutaneously, number of intubation days before and after the procedure, infant survival and complications probably related to balloon atrial septostomy, including transient tachycardia, atrial dysrhythmias – for example, atrial flutter – rupture or thrombosis of the femoral vein, atrial thrombosis, seizures, intracranial haemorrhage, heart failure, pericardial effusion and tamponade, pneumothorax, anaemia, and acidosis. Mortality was assumed to be related to the procedure if the patients died before further surgery, related to surgery if the patients died shortly after surgery, or unrelated if it occurred later than 6 months after surgery. Similarly, complications were considered to be directly related to balloon atrial septostomy if they occurred before further surgery.
The institutional audit committee approved the study protocol on the 25th of May 2010.
Time of procedure
Procedure data including the type, timing, duration of the procedure performed, and the cardiologists involved were recorded. We divided our sample into two groups according to the time of the day the procedure was performed: procedures performed during routine hours (9 am to 6 pm) or out-of-hours (6:01 pm to 8.59 am).
Balloon atrial septostomy
Indications for balloon atrial septostomy were based on echocardiographic assessment – patency and size of the interatrial communication, patency and size of the arterial duct, and systemic arterial oxygen saturation. The urgency for performing the procedure was based on the clinical situation and the anticipated delay until further surgery. All procedures were performed under general anaesthesia using the Rashkind pull-back technique under echocardiographic guidance. Successful vascular access was achieved either via the umbilical vein or femoral vein. A Fogarty (Baxter Healthcare Corporation, Irvine, California, United States of America) or Miller (Edwards Lifesciences, Irvine, California, United States of America) septostomy balloon catheter was introduced either directly through the umbilical vein or via a 6 French/7 French inguinal sheath and the balloon catheter was then placed across the atrial septum. The balloon was inflated and then rapidly withdrawn across the septum. This technique was repeated with increasing balloon sizes until a satisfactory atrial communication was obtained.Reference Rashkind and Miller 8 Heparin was not given routinely for the procedure at our institution.
Data analysis
Clinical variables of neonates who underwent the procedure in routine hours and out-of-hours were compared using SPSS 18.0, version 2009 (SPSS, Chicago, Illinois, United States of America) with t-test used for continuous parametric data, Mann–Whitney test for continuous non-parametric data, and chi-square test applied for categorical data. A p-value of <0.05 was considered to be significant.
Results
Pre-procedural data
Patient details are depicted in Table 1.
Table 1 Characteristics of infants who underwent balloon atrial septostomy in the daytime compared with those who underwent the procedure out-of-hours.
The values for birth weight, age at septostomy, pre-procedure arterial oxygen saturations, and intubation days before balloon atrial septostomy are mean values. Where appropriate, a range/standard deviation has been provided
In all, 42 infants (39.6%) had the procedure performed out-of-hours and 64 infants (60.4%) had the procedure performed in the daytime (see Table 1). There was no significant difference in the characteristics of infants in the two groups with regard to sex distribution, birth weight, age at septostomy, pre-procedural arterial oxygen saturations, or mean intubation days before the procedure. The arterial oxygen saturations in patients who underwent balloon atrial septostomy in routine hours was 61% (confidence interval, 13%) and 45% (confidence interval, 13%) in patients treated out-of-hours (p = 0.109). The difference, however, was not statistically significant.
Neonates in each group were also compared in terms of their diagnosis, and no significant difference was present in terms of the distribution of neonates among the two groups (Table 1).
Infants were also compared with regard to the access sites to rule out any significant difference between the groups. In the routine-hours group, 16 out of 64 septostomies were carried out via umbilical access, whereas in the out-of-hours group 10 out of 42 septostomies were performed via umbilical access. The jugular vein was used in one patient in each group and the remainder were done from the femoral venous approach. There were no statistically significant differences.
Post-procedural data
Neonates who underwent the procedure in routine hours compared with those who underwent the procedure out-of-hours had similar outcome results in terms of post-procedural arterial oxygen saturation values and number of intubation days. The mean value of the post-procedural arterial oxygen saturations in both groups was 86%. Intubation days after balloon atrial septostomy differed slightly, with a mean value of 4 (0–11) in the routine-hours group and a mean value of 5 (0–10) in the out-of-hours group. There was, however, no statistically significant difference (see Table 2).
Table 2 Post-procedural outcome in newborns who underwent balloon atrial septostomy in routine hours compared with those who underwent the procedure out-of-hours.

Complications after balloon atrial septostomy
Complications immediately related to the procedure occurred in 12 out of 64 (18.8%) infants from the routine-hours group and in 20 out of 42 (47.6%) infants from the out-of-hours group. During follow-up after surgery, seven more infants (10.9%) suffered complications after balloon atrial septostomy in the routine-hours group, whereas four more infants (9.5%) suffered complications in the out-of-hours group. This totalled the complication rate in the routine-hours group to 19 infants (29.7%) and 24 infants (57.1%) in the out-of-hours group (p = 0.001).
There was a statistically significant higher incidence of thrombus formation in the femoral vein immediately after balloon atrial septostomy in patients who underwent the procedure out-of-hours. All five incidents of thrombosis in the out-of-hours group occurred after balloon atrial septostomy, whereas in the routine-hours category only one of the three incidents of thrombosis happened after balloon atrial septostomy, the remaining occurred after surgery. In another incident, a balloon atrial septostomy performed in routine hours resulted in a ruptured balloon and the infant developed atrial thrombosis.
Neurological problems were identified in five neonates in the routine-hours group, three of whom experienced immediate complications after balloon atrial septostomy while two other neonates had neurological problems after surgery. These included episodes of generalised tonic–clonic seizures, episodes of focal seizures, short-span seizures, and two cases of ischaemic brain injury.
In the out-of-hours group, two neonates experienced neurological problems immediately after balloon atrial septostomy and before further surgery. This included one infant who experienced focal seizures and another neonate who experienced repeated episodes of seizures, probably because of hypocalcaemia. However, the difference between the groups was not significant.
There was also a higher incidence of necrotising enterocolitis in newborns who had the procedure out-of-hours. A total of two incidents of necrotising enterocolitis occurred in routine hours, all of which were immediately related to balloon atrial septostomy, whereas three out of the five reported cases of necrotising enterocolitis in the out-of-hours group occurred immediately after balloon atrial septostomy.
Further complications in the out-of-hours group – but not in routine hours – included one incident of an accidental insertion of the sheath into the femoral artery by an experienced consultant paediatric cardiologist, and in two other infants their oxygen saturations dropped after balloon atrial septostomy. In the out-of-hours group, two infants also had acute pericardial tamponade with effusion after balloon atrial septostomy. All complications are depicted in Table 3.
Table 3 Mortality and complications after balloon atrial septostomy in neonates who underwent the procedure in routine hours compared with those who underwent the procedure out-of-hours.

Mortality
Procedure-related mortality occurred only out-of-hours and was low (less than 3%). The overall mortality rate in the group of neonates who underwent balloon atrial septostomy out-of-hours was significantly higher compared with that of the neonates who underwent the procedure in routine hours (see Fig 1, Table 3). A total of four deaths were accounted for in the routine-hours group, whereas 12 deaths were recorded in the out-of-hours group.
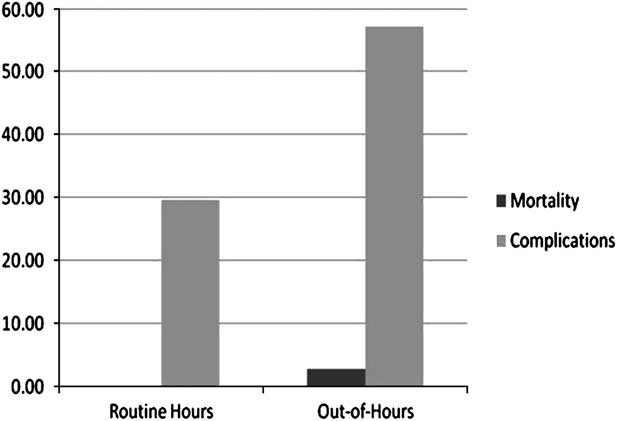
Figure 1 Bar graph comparing mortality rates (immediately after balloon atrial septostomy) and complication rates in patients undergoing the procedure during routine hours and out-of-hours.
Routine hours
All patients survived to further surgical treatment. Within 30 days after balloon atrial septostomy, three neonates died, of whom two were brain dead after surgery and one died because of cardiac failure. The fourth death was 3 years after the procedure, and the cause of death remains unknown. This infant was diagnosed with Hypoplastic Left Heart Syndrome (HLHS), and experienced complications during balloon atrial septostomy – balloon rupture and atrial thrombosis.
Out-of-hours
In all, three infants died after balloon atrial septostomy before surgery: two were in poor pre-procedural condition and another baby was hypotensive with poor peripheral perfusion. This particular neonate with hypoplastic left heart showed pulmonary overcirculation after balloon atrial septostomy requiring paralysis and hypoventilation to balance the systemic and pulmonary circulation, but without long-term success. In all, seven infants died after surgery, of whom two were brain dead, three suffered cardiac arrests and could not be resuscitated, one infant did not recover from a critical haemodynamic condition, and another had malignant atrial and ventricular arrhythmias. It is noteworthy that this infant who was in critical haemodynamic condition suffered from acute pericardial tamponade after balloon atrial septostomy. One of the infants who suffered a cardiac arrest had a known diagnosis of Hypoplastic Left Heart Syndrome, and underwent a Hybrid procedure consisting of bilateral pulmonary artery bands, stenting of the arterial duct, and subsequent balloon atrial septostomy, and also had necrotising enterocolitis. Two babies died 8 and 9 months later, respectively, but the cause of death remains unknown. The underlying diagnoses of the deceased patients are depicted in Table 4.
Table 4 Diagnosis of deceased infants (overall mortality).

Discussion
The time of the day when a balloon atrial septostomy is performed seems to have an influence on the outcome. We found that complications were observed more frequently and that both mortality and morbidity occurred at a significantly higher rate when balloon atrial septostomy was carried out out-of-hours.
Rashkind Balloon Atrial Septostomy is a fairly common procedure, performed with the aim of improving systemic saturation levels in newborns with cyanotic congenital heart defects.Reference Penny and Shekerdemian 9 However, recent reports on the safety of this procedure have raised some concern about the necessity of this procedure in some cases.Reference Mukherjee, Lindsay and Zhang 10 The decision and urgency to perform balloon atrial septostomy in neonates remains a complex one, usually determined by clinical features of hypoxia and echocardiographic assessment.Reference Baellan and Gleason 11 The influence of the timing of the intervention on complications, morbidity, and mortality has not been determined so far, although for some surgical procedures over a decade ago a group of surgeons in a multi-centre study had come to the consensus that up to one-third of emergency procedures performed during the night could have been safely deferred to the following day.Reference McKee, Priest, Ginzler and Black 12
One important reason to carry out a balloon atrial septostomy is because the clinical situation requires urgent therapy to allow adequate mixing of the oxygen saturated with desaturated blood. Patients in the out-of-hours group of our study generally had lower arterial oxygen saturations pre-procedurally, even though this was not statistically significant. Another reason for a balloon atrial septostomy is to allow adequate mixing until surgery is carried out electively – these procedures are commonly carried out electively in the daytime.
In our study, the indication to perform a balloon atrial septostomy was discussed with the consultant paediatric cardiologist in the department, who was always present during the procedure. However, the condition of the patient during each procedure could vary markedly. For example, four of the neonates diagnosed with Hypoplastic Left Heart Syndrome – three of whom underwent balloon atrial septostomy during the night – did not do well after balloon atrial septostomy and after surgery. A report on the need for balloon atrial septostomy in Hypoplastic Left Heart Syndrome infants with restrictive interatrial communication highlighted the importance of timing when performing this procedure.Reference Mulla and Osher 13 According to that study, balloon atrial septostomy performed in infants with very small interatrial communication with severe cyanosis were at higher risk of the procedure failing and the risk for patient death was considerable. It was noted that balloon atrial septostomy should ideally be performed before the infant reached severe desaturation values for better outcome rates.Reference Mulla and Osher 13 The oxygen saturation values in all Hypoplastic Left Heart Syndrome infants in our present study were critically low, which could have contributed to the poor outcome. However, it is useful to note that even if the Hypoplastic Left Heart Syndrome neonates were excluded from analysis, the difference in mortality would still be statistically significant between the two groups (p = 0.011). Thus, we conclude that no specific diagnosis was a risk factor for balloon atrial septostomy.
Another key factor for daytime procedures is the presence of adequately rested personnel. In our study, an incident occurred during a procedure performed at night where the sheath was inserted accidentally into the femoral artery instead of the femoral vein. Although this was a solitary case, such accidents are more prone to happen when the staff are deprived of sleep. To support the influence of timing on procedures, the National Confidential Enquiry into Patient Outcome and Death have advocated caution regarding unnecessary out-of-hours procedures in the 2003 “Who Operates When? II” report. 14
A higher proportion of patients experienced thrombi in the femoral vein after balloon atrial septostomy out-of-hours and a significantly higher proportion suffered from necrotising enterocolitis. Interestingly, this was independent of the underlying heart disease. It can be questioned whether the babies undergoing night-time procedures were sicker anyway. In procedures performed out-of-hours, the oxygen saturation in two infants also deteriorated after balloon atrial septostomy.
We took even minor complications into account, and thus the relatively high overall complication rate. This is otherwise comparable to previous studies; for example, Akagi and colleagues reported the rate of common complications such as arrhythmias, vascular and bleeding complications in post-balloon atrial septostomy to be between 0% and 11%.Reference Akagi, Tananari and Maeno 15 , Reference Vitiello, McCrindle, Nykanen, Freedom and Benson 16
Our overall mortality rate is higher than in the report of the National Institute for Clinical Excellency in 2004, but this is due to the fact that we took all deceased children into account, regardless of the time between balloon atrial septostomy and death. The National Institute for Clinical Excellency data only accounts for mortality from balloon atrial septostomy until the next planned procedure, for example during or immediately after procedure. If our data are analysed in the same way, our procedure-related mortality rate was 2.8% and therefore within the expected limits. Nevertheless, we included later mortality to highlight the severity of congenital heart disease initially leading to balloon atrial septostomy. Again, it seems to reflect the fact that children undergoing balloon atrial septostomy out-of-hours are more severely affected by their congenital heart disease. If the atrial septum is more restrictive, the pulmonary vascular resistance is likely to be higher, thus complicating post-operative management. In these patients, an immediate/urgent intervention may be recommended.
Limitations
Although this is a retrospective study with a limited sample size of only 106 patients included, it is comparable in size to other published reports looking at complication rates and adverse outcomes of balloon atrial septostomy. For example, a recently published report to determine the risk of balloon atrial septostomy causing brain injury in infants by Beca comprised 64 newborns.Reference Beca and Gunn 17 They found brain injury in 19 out of 64 (30%) patients.
Another significant but inevitable limitation of this study is that infants who had the procedure out-of-hours appeared generally clinically more critically ill, although none of the parameters tested showed statistically significant differences. There was only a trend towards lower arterial oxygen saturation values. Comparison between the outcome of neonates who underwent balloon atrial septostomy and neonates who did not undergo balloon atrial septostomy was not done in this present study, but this has been evaluated in numerous other published reports.Reference Applegate and Lim 18
Conclusion
Balloon atrial septostomy performed out-of-hours produced higher adverse outcome rates as opposed to balloon atrial septostomy performed in routine hours. This may be due to the fact that these patients were considered ill enough to do the procedure as an emergency intervention. Nonetheless, in view of our findings, it seems important to review the patients carefully, so that only essential cases are undertaken in the night time while all other cases should be deferred to the daytime to limit unnecessary adverse complication.
Acknowledgements
We would like to thank Thomas Witter for his help with the data collection.







